Abstract
Purpose of Review
A global study of multimorbidity in schizophrenia, especially of the association with physical conditions, might offer much needed etiological insights.
Recent Findings
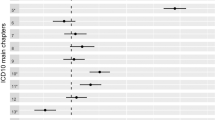
Our review suggests that life-style factors and medication related to schizophrenia are only part of the explanation of the increase in risk for cardiovascular, metabolic, pulmonary disorders, and some cancers. Positive associations with autoimmune disorders (with the exception of rheumatoid arthritis) and epilepsy are promising avenues of research but to date have not been fully exploited. The same holds for the negative comorbidity seen for rheumatoid arthritis and some cancers (e.g., prostate).
Summary
As a whole, our review suggests that most of the explored conditions have a different prevalence in schizophrenia than in the general population. Several hypotheses emerged from this review such as the role of immune and genetic factors, of sex hormones, and of more general variability factors.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009;7:357–63.
Caron C, Rutter M. Comorbidity in child psychopathology: concepts, issues and research strategies. J Child Psychol Psychiatry. 1991;32:1063–80.
Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry Allied Disciplines. 1999;40:57–87.
Lilienfeld SO, Waldman ID, Israel AC. A critical examination of the use of the term and concept of comorbidity in psychopathology research. Clin Psychol Sci Pract. 1994;1:71–83.
•• Wetterling T. Pathogenesis of multimorbidity—what is known? Z Gerontol Geriatr. 2021;54:590–6. Interesting article describing different putative mechanisms that might explain multimorbidity.
Font H, Roelandt J-L, Behal H, Geoffroy P-A, Pignon B, Amad A, et al. Prevalence and predictors of no lifetime utilization of mental health treatment among people with mental disorders in France: findings from the ‘Mental Health in General Population’ (MHGP) survey. Soc Psychiatry Psychiatr Epidemiol. 2018;53:567–76.
Fan Z, Wu Y, Shen J, Ji T, Zhan R. Schizophrenia and the risk of cardiovascular diseases: a meta-analysis of thirteen cohort studies. J Psychiatr Res. 2013;47:1549–56.
• Kowal C, Peyre H, Amad A, Pelissolo A, Leboyer M, Schürhoff F, et al. Psychotic, mood, and anxiety disorders and venous thromboembolism: a systematic review and meta-analysis. Psychosom Med. 2020;82:838–49. This systematic review and meta-analysis of the association between venous thromboembolism and psychiatric disorders revealed that psychotic disorders increased the risk of pulmonary embolism, deep veinous thrombosis and fatal issues.
•• Ali S, Santomauro D, Ferrari AJ, Charlson F. Excess mortality in severe mental disorders: a systematic review and meta-regression. J Psychiatr Res. 2022;149:97–105. The most recent estimation, based on meta-analytical data, of the excess mortality from cardiovascular and diabetes in subjects with schizophrenia.
Ali S, Santomauro D, Ferrari AJ, Charlson F. Schizophrenia as a risk factor for cardiovascular and metabolic health outcomes: a comparative risk assessment. Epidemiol Psychiatr Sci. 2023;32:e8.
Moran P, Stewart R, Brugha T, Bebbington P, Bhugra D, Jenkins R, et al. Personality disorder and cardiovascular disease: results from a national household survey. J Clin Psychiatry. 2007;68:69–74.
Quirk SE, El-Gabalawy R, Brennan SL, Bolton JM, Sareen J, Berk M, et al. Personality disorders and physical comorbidities in adults from the United States: data from the National Epidemiologic Survey on Alcohol and Related Conditions. Soc Psychiatry Psychiatr Epidemiol. 2015;50:807–20.
Mothi SS, Tandon N, Padmanabhan J, Mathew IT, Clementz B, Tamminga C, et al. Increased cardiometabolic dysfunction in first-degree relatives of patients with psychotic disorders. Schizophr Res. 2015;165:103–7.
• Suetani S, Honarparvar F, Siskind D, Hindley G, Veronese N, Vancampfort D, et al. Increased rates of respiratory disease in schizophrenia: a systematic review and meta-analysis including 619,214 individuals with schizophrenia and 52,159,551 controls. Schizophr Res. 2021;237:131–40. Recent meta-analysis of the association between schizophrenia and respiratory diseases (asthma, COPD, pneumonia).
Jaén-Moreno MJ, Rico-Villademoros F, Ruiz-Rull C, Laguna-Muñoz D, Del Pozo GI, Sarramea F. A systematic review on the association between schizophrenia and bipolar disorder with chronic obstructive pulmonary disease. COPD. 2023;20:31–43.
Mirabelli MC, Beavers SF, Chatterjee AB, Moorman JE. Age at asthma onset and subsequent asthma outcomes among adults with active asthma. Respir Med. 2013;107:1829–36.
Pedersen MS, Benros ME, Agerbo E, Børglum AD, Mortensen PB. Schizophrenia in patients with atopic disorders with particular emphasis on asthma: a Danish population-based study. Schizophr Res. 2012;138:58–62.
Wang WC, Lu ML, Chen VCH, Ng MH, Huang KY, Hsieh MH, et al. Asthma, corticosteroid use and schizophrenia: a nationwide population-based study in Taiwan. PLOS ONE. 2017;12:e0173063.
Wu Q, Dalman C, Karlsson H, Lewis G, Osborn DPJ, Gardner R, et al. Childhood and parental asthma, future risk of bipolar disorder and schizophrenia spectrum disorders: a population-based cohort study. Schizophr Bull. 2019;45:360–8.
Judd LL, Schettler PJ, Brown ES, Wolkowitz OM, Sternberg EM, Bender BG, et al. Adverse consequences of glucocorticoid medication: psychological, cognitive, and behavioral effects. AJP. 2014;171:1045–51.
Broberg BV, Sommer IE, Benros ME, Glenthøj BY, Gasse C, Köhler-Forsberg O. Glucocorticoids and the risk of schizophrenia spectrum disorder in childhood and adolescence – a Danish nationwide study. Schizophr Res. 2018;199:116–22.
Stevens JR. Schizophrenia and multiple sclerosis. Schizophr Bull. 1988;14:231–41.
Arneth BM. Multiple sclerosis and schizophrenia. Int J Mol Sci. 2017;18:1760.
• Cao Y, Ji S, Chen Y, Zhang X, Ding G, Tang F. Association between autoimmune diseases of the nervous system and schizophrenia: a systematic review and meta-analysis of cohort studies. Compr Psychiatry. 2023;122:152370. Recent meta-analysis on the association between autoimmune nervous disorders (more notably multiple sclerosis) and schizophrenia (complements an older meta-analysis ref. 64, Cullen et al. focusing on non-neurological autoimmune disorders).
Meier U-C, Ramagopalan SV, Goldacre MJ, Goldacre R. Risk of schizophrenia and bipolar disorder in patients with multiple sclerosis: record-linkage studies. Front Psychiatry [Internet]. 2020 [cited 2023 Dec 21];11. Available from: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.00662.
Clancy MJ, Clarke MC, Connor DJ, Cannon M, Cotter DR. The prevalence of psychosis in epilepsy; a systematic review and meta-analysis. BMC Psychiatry. 2014;14:75.
Gaitatzis A, Trimble MR, Sander JW. The psychiatric comorbidity of epilepsy. Acta Neurol Scand. 2004;110:207–20.
Qin P, Xu H, Laursen TM, Vestergaard M, Mortensen PB. Risk for schizophrenia and schizophrenia-like psychosis among patients with epilepsy: population based cohort study. BMJ. 2005;331:23.
Chang Y-T, Chen P-C, Tsai I-J, Sung F-C, Chin Z-N, Kuo H-T, et al. Bidirectional relation between schizophrenia and epilepsy: a population-based retrospective cohort study. Epilepsia. 2011;52:2036–42.
Wotton CJ, Goldacre MJ. Coexistence of schizophrenia and epilepsy: record-linkage studies. Epilepsia. 2012;53:e71–4.
Clarke MC, Tanskanen A, Huttunen MO, Clancy M, Cotter DR, Cannon M. Evidence for shared susceptibility to epilepsy and psychosis: a population-based family study. Biol Psychiat. 2012;71:836–9.
• Lindekilde N, Scheuer SH, Rutters F, Knudsen L, Lasgaard M, Rubin KH, et al. Prevalence of type 2 diabetes in psychiatric disorders: an umbrella review with meta-analysis of 245 observational studies from 32 systematic reviews. Diabetologia. 2022;65:440–56. The most recent and complete analysis of the association between T2DM and psychiatric disorders (including psychosis/schizophrenia).
Greenhalgh AM, Gonzalez-Blanco L, Garcia-Rizo C, Fernandez-Egea E, Miller B, Arroyo MB, et al. Meta-analysis of glucose tolerance, insulin, and insulin resistance in antipsychotic-naïve patients with nonaffective psychosis. Schizophr Res. 2017;179:57–63.
Rajkumar AP, Horsdal HT, Wimberley T, Cohen D, Mors O, Børglum AD, et al. Endogenous and antipsychotic-related risks for diabetes mellitus in young people with schizophrenia: a Danish population-based cohort study. Am J Psychiatry. 2017;174:686–94.
•• Morera D, Miller BJ. Meta-analysis of a family history of diabetes in schizophrenia. Schizophr Res. 2024;264:90–4. This study demonstrates that patients with schizophrenia compared with controls have more than a double increase in odds of a family history of T2DM versus controls.
Afzal M, Siddiqi N, Ahmad B, Afsheen N, Aslam F, Ali A, et al. Prevalence of overweight and obesity in people with severe mental illness: systematic review and meta-analysis. Front Endocrinol (Lausanne). 2021;12:769309.
Vancampfort D, Stubbs B, Mitchell AJ, De Hert M, Wampers M, Ward PB, et al. Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta-analysis. World Psychiatry. 2015;14:339–47.
Gurpegui M, Martínez-Ortega JM, Gutiérrez-Rojas L, Rivero J, Rojas C, Jurado D. Overweight and obesity in patients with bipolar disorder or schizophrenia compared with a non-psychiatric sample. Prog Neuropsychopharmacol Biol Psychiatry. 2012;37:169–75.
Manu P, Dima L, Shulman M, Vancampfort D, De Hert M, Correll CU. Weight gain and obesity in schizophrenia: epidemiology, pathobiology, and management. Acta Psychiatr Scand. 2015;132:97–108.
Tian Y, Wang D, Wei G, Wang J, Zhou H, Xu H, et al. Prevalence of obesity and clinical and metabolic correlates in first-episode schizophrenia relative to healthy controls. Psychopharmacology. 2021;238:745–53.
Bioque M, García-Portilla MP, García-Rizo C, Cabrera B, Lobo A, González-Pinto A, et al. Evolution of metabolic risk factors over a two-year period in a cohort of first episodes of psychosis. Schizophr Res. 2018;193:188–96.
Gerlach G, Loeber S, Herpertz S. Personality disorders and obesity: a systematic review. Obes Rev. 2016;17:691–723.
Maclean JC, Xu H, French MT, Ettner SL. Personality disorders and body weight. Econ Hum Biol. 2014;12:153–71.
•• Wootten JC, Wiener JC, Blanchette PS, Anderson KK. Cancer incidence and stage at diagnosis among people with psychotic disorders: systematic review and meta-analysis. Cancer Epidemiol. 2022;80:102233. This systematic review and meta-analysis found a pooled age-adjusted risk ratio of all cancer slightly higher than in the general population but with important variations according to the specific type of cancer (it also shows an increased risk of metastasis at diagnosis of cancer in schizophrenia subjects).
Zhuo C, Tao R, Jiang R, Lin X, Shao M. Cancer mortality in patients with schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2017;211:7–13.
Mitchell AJ, Pereira IES, Yadegarfar M, Pepereke S, Mugadza V, Stubbs B. Breast cancer screening in women with mental illness: comparative meta-analysis of mammography uptake. Br J Psychiatry. 2014;205:428–35.
Li H, Li J, Yu X, Zheng H, Sun X, Lu Y, et al. The incidence rate of cancer in patients with schizophrenia: a meta-analysis of cohort studies. Schizophr Res. 2018;195:519–28.
Ji J, Sundquist K, Ning Y, Kendler KS, Sundquist J, Chen X. Incidence of cancer in patients with schizophrenia and their first-degree relatives: a population-based study in Sweden. Schizophr Bull. 2013;39:527–36.
• Zhou K, Zhu L, Chen N, Huang G, Feng G, Wu Q, et al. Causal associations between schizophrenia and cancers risk: a Mendelian randomization study. Front Oncol. 2023;13:1258015. This is the most comprehensive study using Mendelian randomization to explore the causality link between cancer and schizophrenia.
Callaghan RC, Veldhuizen S, Jeysingh T, Orlan C, Graham C, Kakouris G, et al. Patterns of tobacco-related mortality among individuals diagnosed with schizophrenia, bipolar disorder, or depression. J Psychiatr Res. 2014;48:102–10.
Hunt GE, Large MM, Cleary M, Lai HMX, Saunders JB. Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990–2017: Systematic review and meta-analysis. Drug Alcohol Depend. 2018;191:234–58.
Godin O, Leboyer M, Schürhoff F, Llorca P-M, Boyer L, Andre M, et al. Metabolic syndrome and illness severity predict relapse at 1-year follow-up in schizophrenia: the FACE-SZ cohort. J Clin Psychiatry. 2018;79.
• Godin O, Pignon B, Szoke A, Boyer L, Aouizerate B, Schorr B, et al. 3-year incidence and predictors of metabolic syndrome in schizophrenia in the national FACE-SZ cohort. Prog Neuropsychopharmacol Biol Psychiatry. 2023;120:110641. One of the few existing longitudinal studies of a “real-world” schizophrenia cohort shows a 20.8% incidence in 3 years and identifies several risk factors (i.e. tobacco use, antidepressant).
Ajmal A, Joffe H, Nachtigall LB. Psychotropic-induced hyperprolactinemia: a clinical review. Psychosomatics. 2014;55:29–36.
• Hope JD, Keks NA, Copolov DL. Association between long-term use of prolactin-elevating antipsychotics in women and the risk of breast cancer: what are the clinical implications? Australas Psychiatry. 2023;31:205–8, A recent review of the potential role of antipsychotics and prolactin increase in the risk of breast cancer.
De Hert M, Peuskens J, Sabbe T, Mitchell AJ, Stubbs B, Neven P, et al. Relationship between prolactin, breast cancer risk, and antipsychotics in patients with schizophrenia: a critical review. Acta Psychiatr Scand. 2016;133:5–22.
Tang M, Wu X, Zhang W, Cui H, Zhang L, Yan P, et al. Epidemiological and genetic analyses of schizophrenia and breast cancer. Schizophr Bull. 2023;sbad106.
Cui Y, Lu W, Shao T, Zhuo Z, Wang Y, Zhang W. Severe mental illness and the risk of breast cancer: a two-sample, two-step multivariable Mendelian randomization study. PLoS ONE. 2023;18:e0291006.
Ren F, Shang Q, Zhao S, Yang C, Feng K, Liu J, et al. An exploration of the correlations between seven psychiatric disorders and the risks of breast cancer, breast benign tumors and breast inflammatory diseases: Mendelian randomization analyses. Front Psychiatry. 2023;14:1179562.
Zhang M, Tang J, Li W, Xue K, Wang Z, Chen Y, et al. Schizophrenia mediating the effect of smoking phenotypes on antisocial behavior: a Mendelian randomization analysis. CNS Neurosci Ther. 2023.
Wang L, Wang F-S, Gershwin ME. Human autoimmune diseases: a comprehensive update. J Intern Med. 2015;278:369–95.
Cooper GS, Bynum MLK, Somers EC. Recent insights in the epidemiology of autoimmune diseases: improved prevalence estimates and understanding of clustering of diseases. J Autoimmun. 2009;33:197–207.
Cullen AE, Holmes S, Pollak TA, Blackman G, Joyce DW, Kempton MJ, et al. Associations between non-neurological autoimmune disorders and psychosis: a meta-analysis. Biol Psychiat. 2019;85:35–48.
Benros ME, Pedersen MG, Rasmussen H, Eaton WW, Nordentoft M, Mortensen PB. A nationwide study on the risk of autoimmune diseases in individuals with a personal or a family history of schizophrenia and related psychosis. AJP. 2014;171:218–26.
de Bartolomeis A, Barone A, Vellucci L, Mazza B, Austin MC, Iasevoli F, et al. Linking inflammation, aberrant glutamate-dopamine interaction, and post-synaptic changes: translational relevance for schizophrenia and antipsychotic treatment: a systematic review. Mol Neurobiol. 2022;59:6460–501.
Torrey EF, Yolken RH. The schizophrenia–rheumatoid arthritis connection: infectious, immune, or both? Brain Behav Immun. 2001;15:401–10.
Benros ME, Nielsen PR, Nordentoft M, Eaton WW, Dalton SO, Mortensen PB. Autoimmune diseases and severe infections as risk factors for schizophrenia: a 30-year population-based register study. Am J Psychiatry. 2011;168:1303–10.
Wang L-Y, Chen S-F, Chiang J-H, Hsu C-Y, Shen Y-C. Autoimmune diseases are associated with an increased risk of schizophrenia: a nationwide population-based cohort study. Schizophr Res. 2018;202:297–302.
Chen S-F, Wang L-Y, Chiang J-H, Hsu C-Y, Shen Y-C. Assessing whether the association between rheumatoid arthritis and schizophrenia is bidirectional: a nationwide population-based cohort study. Sci Rep. 2019;9:4493.
• Prados-Ojeda JL, Luque-Luque R, Gordillo-Urbano RM, Guler I, López-Medina C, Collantes-Estévez E, et al. Assessment of subclinical psychotic symptoms in patients with rheumatoid arthritis and spondyloarthritis. J Clin Med. 2021;10:3461. A rare study using sub-clinical psychosis symptoms (psychometric schizotypy) to explore the association with a physical disorder.
Sellgren C, Frisell T, Lichtenstein P, Landèn M, Askling J. The association between schizophrenia and rheumatoid arthritis: a nationwide population-based Swedish study on intraindividual and familial risks. Schizophr Bull. 2014;40:1552–9.
Jeppesen R, Benros ME. Autoimmune diseases and psychotic disorders. Front Psychiatry [Internet]. 2019 [cited 2023 Dec 21];10. Available from: https://www.frontiersin.org/articles/10.3389/fpsyt.2019.00131.
Leucht S, Burkard T, Henderson J, Maj M, Sartorius N. Physical illness and schizophrenia: a review of the literature. Acta Psychiatr Scand. 2007;116:317–33.
McGrath JJ, Saha S, Chant DC, Welham J. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008;30:67–76.
Ferentinos P, Dikeos D. Genetic correlates of medical comorbidity associated with schizophrenia and treatment with antipsychotics. Curr Opin Psychiatry. 2012;25:381.
•• Szöke A, Pignon B, Boster S, Jamain S, Schürhoff F. Schizophrenia: developmental variability interacts with risk factors to cause the disorder: nonspecific variability-enhancing factors combine with specific risk factors to cause schizophrenia. Bioessays. 2020;e2000038. This article introduces the new concept of “variability factors” that might explain (part) of the multimorbidity in conditions with a developmental component.
Szöke A, Pignon B, Schürhoff F. Schizophrenia risk factors in exceptional achievers: a re-analysis of a 60-year-old database. Sci Rep. 2019;9:1294.
Gogos A, Sbisa AM, Sun J, Gibbons A, Udawela M, Dean B. A role for estrogen in schizophrenia: clinical and preclinical findings. Int J Endocrinol. 2015;2015.
Acknowledgements
The editors would like to thank Dr. Melvin McInnis for taking the time to review this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Szoke, A., Pignon, B., Godin, O. et al. Multimorbidity and the Etiology of Schizophrenia. Curr Psychiatry Rep 26, 253–263 (2024). https://doi.org/10.1007/s11920-024-01500-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11920-024-01500-9