Abstract
Concerns about possible over-diagnosis and over-treatment of attention deficit hyperactivity disorder (ADHD) have been prominent in media reports, as have various competing claims about the safety and efficacy of the various treatments for ADHD. Drawing upon the results of the recent National Institutes of Health Consensus Conference, this paper reviews the evidence concerning these controversial areas. Although there do appear to be pockets of over-prescribing in selected communities, the best available evidence suggests that across the United States substantial underdiagnosis continues to occur, and only 50% of all children with ADHD are being treated with stimulant medications. Among those who are treated with stimulant medications, inadequate treatment is quite common. Substantial evidence suggests that for ADHD symptoms, stimulants are more effective than behavioral therapies in head-to-head comparisons. Combined medication and behavioral treatments do not offer any meaningful advantages over medication treatments alone for ADHD symptoms. For other areas of functioning, however (social skills, academic performance, etc.), combined treatments appear to offer some modest advantages over single treatment approaches. Although research findings show that ADHD can indeed be rigorously and reliably diagnosed under optimal conditions, and that carefully delivered treatments can yield substantial benefits, such best practices do not appear to be taking place in the real world. Thus, although the above controversies are facing some resolution in principal, in practice much remains to be done.
Similar content being viewed by others
References and Recommended Reading
Popper CW: Disorders usually first evident in infancy, childhood, or adolescence. In Textbook of Psychiatry. Edited by Talbott JA, Hales RE, Yudofsky SC. Washington, DC: American Psychiatric Press; 1988:649–735.
Shaffer D, Fisher P, Dulcan M, et al.: The second version of the NIMH Diagnostic Interview Schedule for Children (DISC-2). J Am Acad Child Adolesc Psychiatry 1996, 35:865–877.
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, edn 4. Washington, DC: American Psychiatric Association; 1994.
Lahey BB, Applegate A, McBurnett K, et al.: DSM-IV field trials for attention-deficit hyperactivity disorder in children and adolescents. Am J Psychiatry 1994, 151:1673–1685.
Schachar RJ, Tannock R, Cunningham C, Corkum PV: Behavioral, situational, and temporal effects of treatment of ADHD with methylphenidate. J Am Acad Child Adolesc Psychiatry 1997, 36:754–763.
Biederman J, Newcorn J, Sprich S: Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. Am J Psychiatry 1991, 148:564–577.
Mannuzza S, Klein RG, Bassier A, et al.: Adult outcome of hyperactive boys. Arch Gen Psychiatry 1993, 50:565–576.
Klein RG, Mannuzza S: Long-term outcome of hyperactive children. J Am Acad Child Adolesc Psychiatry 1991, 30:383–387.
Pliszka SR: Effect of anxiety on cognition, behavior, and stimulant response in ADHD. J Am Acad Child Adol Psychiatry 1989, 28:882–887.
Richters J, Arnold LEA, Jensen PS, et al.: NIMH collaborative multimodal treatment study of children with ADHD (MTA): ADHD: I. Background and rationale. J Am Acad Child Adolesc Psychiatry 1995, 34:987–1000.
Shaffer D: Attention deficit hyperactivity in adults. Am J Psychiatry 1994, 151:633–638.
Barkley RA, Fischer M, Edelbrock CS, Smallish L: The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry 1990, 29:546–557.
Jensen P, Bhatara V, Vitiello B, et al.: Psychoactive medication prescribing practices for US children: gaps between research and clinical practice. J Am Acad Child Adolesc Psychiatry 1999, 38:557–565.
LeFever GB, Dawson KV, Morrow AL: The extent of drug therapy for attention deficit-hyperactivity disorder among children in public schools. Am J Public Health 1999, 89:1359–64.
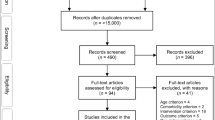
Multimodal Treatment Study of Children with ADHD Cooperative Group: 14-month randomized clinical trial of treatment strategies for attention deficit hyperactivity disorder. Arch Gen Psychiatry 1999, 56:1073–1086. Previous studies have demonstrated the short-term efficacy of pharmacotherapy and behavior therapy for ADHD, but no longerterm (> 4 months) investigations have compared these two treatments or their combination. This study, the so-called MTA, examined a group of 579 children with ADHD-combined type, who were assigned to 14 months of medication management (titration followed by monthly visits); intensive behavioral treatment (parent, school, and child components, with therapist involvement graduallt reduced over time); the two combined; or standard community care (treatments by community providers). All four groups showed sizable reductions in symptoms over time, with significant differences among them in degrees of change. For most ADHD symptoms, children in the combined and medication management groups showed significantly greater improvement than those given intensive behavioral treatment or community care. Combined and medication management treatments did not differ significantly on any direct comparisons, but in several instances (oppositional/aggressive symptoms, internalizing symptoms, teacher-rated social skills, parent-child relations, and reading achievement) combined treatment was superior to intensive behavioral treatment and community care, whereas medication management was not. Thus, for ADHD symptoms, a carefully crafted medication management was superior to behavioral treatment and to routine community care that included medication. Combined treatment did not yield significantly greater benefits than medication management for core ADHD symptoms, but may have provided some additional advantages for non-ADHD symptom and positive functioning outcomes.
Multimodal Treatment Study of Children with ADHD Cooperative Group: Moderator and mediator challenges to the MTA study: effects of comorbid anxiety disorder, family poverty, session attendance, and community medication on treatment outcome. Arch Gen Psychiatry 1999, 56:1088–1096. The first intent-to-treat (ITT) analyses of the MTS revealed that medication management (MedMgt), alone or in combination (Comb) with intensive behavioral treatment (Beh), was superior to Beh and community care (CC) in reducing ADHD symptomatology; but only Comb showed consistently greater benefit than CC across other outcome domains (disruptive and internalizing symptoms, achievement, parent-child relations, social skills). MTA investigators examined response patterns in subgroups defined by baseline variables or variables related to treatment implementation. Study outcomes (n=579) were upheld in most subgroups (boys/girls, children with/without prior medication, children with/without comorbid disruptive disorders). However, comorbid anxiety disorder did moderate outcome: in nonanxious participants, results paralleled ITT findings. For those with anxiety disorders, however, Beh yielded significantly better outcomes than CC regarding ADHDrelated and internalizing symptoms. In families receiving public assistance, MedMgmt yielded decreased closeness in parent-child interactions, and Comb yielded relatively greater benefits for teacherreported social skills. In families with high treatment acceptance/ attendance, ITT results were upheld, but this effect was only seen with medication treatments.
Satterfield JH, Cantwell DP, Satterfield BT: Multimodality treatment: A one-year follow-up of 84 hyperactive boys. Arch Gen Psychiatry 1979, 36:965–974.
Satterfield JH, Satterfield BT, Cantwell DP: Three-year multimodality treatment study of 100 hyperactive boys. J Pediatrics 1981, 98:650–655.
Satterfield JH, Satterfield BT, Schell AM: Therapeutic interventions to prevent delinquency in hyperactive boys. J Am Acad Child Adolesc Psychiatry 1987, 26:56–64.
Jacobvitz D, Sroufe LA, Stewart M, Leffert N: Treatment of attentional and hyperactivity problems in children with sympathomimetic drugs: a comprehensive review. J Am Acad Child Adolesc Psychiatry 1990, 29:677–688.
Spencer T, Biederman J, Wilens T, et al.: Pharmacotherapy of attention-deficit hyperactivity disorder across the life cycle. J Am Acad Child Adolesc Psychiatry 1996, 35:409–432.
Swanson J: Effect of stimulant medication on hyperactive children: a review of reviews. Exceptional Child 1993, 60:154–162.
Gillberg C, Melander H, von Knorring AL, et al.: Long-term stimulant treatment of children with attention-deficit hyperactivity disorder symptoms. A randomized, double-blind, placebo-controlled trial. Arch Gen Psychiatry 1997, 54:857–864.
Hechtman L, Abikoff H: Multimodal treatment plus stimulants vs. stimulant treatment in ADHD children: results from a two year comparative treatment study. Proceedings of the Annual Meeting of the American Academy of Child and Adolescent Psychiatry, New Orleans, LA, October 17–22, 1995.
Pelham WE, Hoza B: Comprehensive treatment for ADHD: a proposal for intensive summer treatment programs and outpatient follow-up. In Psychosocial Treatment Research of Child and Adolescent Disorders. Edited by Hibbs E, Jensen P. New York: APA Press; 1996:311–340.
Abikoff H, Gittelman R: Does behavior therapy normalize the classroom behavior of hyperactive children? Arch Gen Psychiatry 1984, 41:449–454.
Pelham WE, Hinshaw SP: Behavioral intervention for ADHD. In Handbook of clinical behavior therapy, edn 2. Edited by Turner SM, Calhoun KS, Adams HE.). New York, Wiley; 1992:259–283.
Hinshaw SP, Henker B, Whalen CK: Self-control in hyperactive boys in anger-inducing situations: effects of cognitive-behavioral training and of methylphenidate. J Abnorm Child Psychol 1984, 12:55–77.
Abikoff H: An evaluation of cognitive behavior therapy for hyperactive children. In Advances in Clinical Child Psychology, vol. 10. Edited by Lahey BB, Kazdin AE. New York: Plenum Press; 1987:171–216.
Hinshaw SP, Klein RG, Abikoff H: Childhood attention-deficit hyperactivity disorder: nonpharmacologic and combination treatments. In A Guide to Treatments that Work. Edited by Nathan PE, Gorman JM. New York: Oxford University Press; 1998:26–41.
Pelham WE, Wheeler T, Chronis A: Empirically supported psychosocial treatments for attention deficit hyperactivity disorder. J Clin Child Psychol 1998, 27:190–205.
Wells K, Pelham WA, Kotkin RA, et al.: Psychosocial treatment strategies in the MTA study: rationale, methods, and critical issues in design and implementation. J Abn Child Psychol 2000, in press.
Barkley RA, Shelton TL, Crosswait C, et al.: An early multi-method intervention program for preschool children with aggressive and hyperactive-impulsive behavior. Attention-Deficit/Hyperactivity Disorder: Results of recent treatment studies. Paper presented at the Annual Meeting of the American Academy of Child and Adolescent Psychiatry, Toronto, Canada, October 1997.
Arnold L, Abikoff H, Cantwell D, et al.: NIMH Collaborative Multimodal Treatment Study of Children With ADHD (MTA): Design Challenges and Choices. Arch Gen Psychiatry 1997, 54:865–870.
Pelham WE, Murphy HA: Behavioral and pharmacological treatment of hyperactivity and attention-deficit disorders. In Pharmacological and Behavioral Treatment: an Integrative Approach. Edited by Herson M, Breuning SE. New York: Wiley; 1986:108–147.
McMaster University Evidence-based Practice Center: The treatment of attention-deficit/hyperactivity disorder: an evidence report. Contract No. 290-97-0017. Agency for Health Care Policy and Research, 1998.
Ialongo NS, Horn WF, Pascoe JM, et al.: The effects of a multimodal intervention with attention-deficit hyperactivity disorder children: a 9-month follow-up. J Am Acad Child Adolesc Psychiatry 1993, 32:182–189.
Klein RG, Abikoff H: Behavior therapy and methylphenidate in the treatment of children with ADHD. J Attention Disord 1997, 2:89–114.
Horn WF, Ialongo NS, Pascoe JM, et al.: Additive effects of psychostimulants, parent training, and self-control therapy with ADHD children. J Am Acad Child Adolesc Psychiatry 1991, 30:233–240.
Carlson CL, Pelham WE, Milich R, Dixon J: Single and combined effects of methylphenidate and behavior therapy on the classroom performance of children with ADHD. J Abnorm Child Psychol 1992, 20:213–231.
Pelham WE, Carlson CL, Sams SE, Vallano G: Separate and combined effects of methylphenidate and behavior modification on boys with attention-deficit hyperactivity disorder in the classroom. J Cons Clin Psychology 1993, 61:506–515.
Greenhill L, Abikoff H, Arnold L, et al.: Medication treatment strategies in the MTA study: relevance to clinicians and researchers. J Am Acad Child Adolesc Psychiatry 1996, 35:1304–1313.
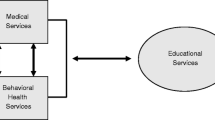
Sloan M, Jensen P, Kettle L: Assessing services for children with ADHD: gaps and opportunities. J Attention Disord 1999 3:13–29.
Firestone P, Crowe D, Goodman JT, McGrath P: Vicissitudes of follow-up studies: differential effects of parent training and stimulant medication with hyperactives. Am J Orthopsychiatry 1986, 56:184–194.
Abikoff H, Gittelman-Klein R: The normalizing effects of methylphenidate on the classroom behavior of hyperactive children. J Abn Child Psychology 1985, 13:33–44.
Brown RT, Wynne ME, Medenis R: Methylphenidate and cognitive therapy: a comparison of treatment approaches with hyperactive boys. J Abnorm Child Psychol 1985, 13:69–87.
Brown RT, Borden KA, Wynne ME, et al.: Methylphenidate and cognitive therapy with ADD children: a methodologic reconsideration. J Abnorm Child Psychol 1986, 14:481–497.
Gittelman-Klein R, Klein DF, Abikoff H, et al.: Relative efficacy of methylphenidate and behavior modification in hyperkinetic children: an interim report. J Abnorm Child Psychol 1976, 4:361–379.
Long N, Rickert VI, Ashcraft EW: Bibliotherapy as an adjunct to stimulant medication in the treatment of attention-deficit hyperactivity disorder. J Ped Health Care 1993, 7:82–88.
Solanto MV, Wender EH, Bartell SS: Effects of methylphenidate and behavioral contingencies on sustained attention in attention-deficit hyperactivity disorder: a test of the reward dysfunction hypothesis. J Child Adolesc Psychopharmacol 1997, 7:123–136.
Thurston LP: Comparison of the effects of parent training and of Ritalin in treating hyperactive children. Int J Mental Health 1979, 8:121–128.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Jensen, P.S. Current concepts and controversies in the diagnosis and treatment of attention deficit hyperactivity disorder. Curr Psychiatry Rep 2, 102–109 (2000). https://doi.org/10.1007/s11920-000-0053-z
Issue Date:
DOI: https://doi.org/10.1007/s11920-000-0053-z