Abstract
Purpose of Review
In this narrative review, we discuss key questions about the antifungal treatment of complicated intrabdominal infections (cIAI).
Recent Findings
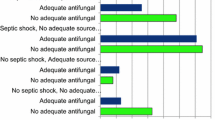
Although less common than bacteria, Candida spp. are not an infrequent cause of cIAI. Considering that invasive abdominal candidiasis (IAC) may be accompanied by septic shock in up to 40% of cases, empirical antifungal treatment should be considered while waiting for rapid tests and cultures results, and it should be guided by the presence of risk factors for invasive candidiasis in patients with consistent signs and symptoms. Early antifungal therapy before availability of culture results can be partly based on the results of rapid diagnostic tests such as antigen/antibody assays or other rapid methods, although it should be noted that most data pertaining to the use of rapid tests refer to candidemia or invasive candidiasis in general, and not specifically to IAC, thus clinical judgment still remains crucial. Although cultures are hampered by a slow turnaround time, they remain of paramount importance, by allowing identification at species level and antifungal susceptibility testing.
Summary
Together with source control, adequate antifungal therapy is an essential component of the correct approach to IAC. Future research should focus on enriching our knowledge on the diagnostic performance of rapid tests in cIAI, and on providing a standardized definition for IAC. Advancements in these fields are crucial for improving the correct use of antifungals at the bedside of cIAI patients and also for reducing unnecessary antifungal use in line with antifungal stewardship principles.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Bassetti M, Eckmann C, Giacobbe DR, Sartelli M, Montravers P. Post-operative abdominal infections: epidemiology, operational definitions, and outcomes. Intensive Care Med. 2019;46(2):163–72. https://doi.org/10.1007/s00134-019-05841-5A recent review regarding current major clinical and research questions in the field of cIAI.
Bassetti M, Righi E, Ansaldi F, Merelli M, Scarparo C, Antonelli M, et al. A multicenter multinational study of abdominal candidiasis: epidemiology, outcomes and predictors of mortality. Intensive Care Med. 2015;41:1601–10.
De Waele J, Lipman J, Sakr Y, Marshall JC, Vanhems P, Barrera Groba C, et al. Abdominal infections in the intensive care unit: characteristics, treatment and determinants of outcome. BMC Infect Dis. 2014;14:420.
Sartelli M, Catena F, Ansaloni L, Coccolini F, Corbella D, Moore EE, et al. Complicated intra-abdominal infections worldwide: the definitive data of the ciaow study. World J Emerg Surg. 2014;9:37.
Sartelli M, Weber DG, Ruppe E, Bassetti M, Wright BJ, Ansaloni L, et al. Antimicrobials: a global alliance for optimizing their rational use in intra-abdominal infections (agora). World J Emerg Surg. 2016;11:33.
• Montravers P, Blot S, Dimopoulos G, Eckmann C, Eggimann P, Guirao X, et al. Therapeutic management of peritonitis: a comprehensive guide for intensivists. Intensive Care Med. 2016;42:1234–47 Discussion of the approach to peritonitis from the intensivist’s perspective.
Bassetti M, Marchetti M, Chakrabarti A, Colizza S, Garnacho-Montero J, Kett DH, et al. A research agenda on the management of intra-abdominal candidiasis: results from a consensus of multinational experts. Intensive Care Med. 2013;39:2092–106.
Dupont H, Paugam-Burtz C, Muller-Serieys C, Fierobe L, Chosidow D, Marmuse JP, et al. Predictive factors of mortality due to polymicrobial peritonitis with candida isolation in peritoneal fluid in critically ill patients. Arch Surg. 2002;137:1341–6 discussion 47.
Montravers P, Dupont H, Gauzit R, Veber B, Auboyer C, Blin P, et al. Candida as a risk factor for mortality in peritonitis. Crit Care Med. 2006;34:646–52.
Sandven P, Qvist H, Skovlund E, Giercksky KE, N. Group, G. the Norwegian Yeast Study. Significance of candida recovered from intraoperative specimens in patients with intra-abdominal perforations. Crit Care Med. 2002;30:541–7.
Pappas PG, Lionakis MS, Arendrup MC, Ostrosky-Zeichner L, Kullberg BJ. Invasive candidiasis. Nat Rev Dis Primers. 2018;4:18026.
Bassetti M, Giacobbe DR, Vena A, Trucchi C, Ansaldi F, Antonelli M, et al. Incidence and outcome of invasive candidiasis in intensive care units (icus) in europe: results of the eucandicu project. Crit Care. 2019;23:219.
•• Bassetti M, Scudeller L, Giacobbe DR, Lamoth F, Righi E, Zuccaro V, et al. Developing definitions for invasive fungal diseases in critically ill adult patients in intensive care units. Protocol of the fungal infections definitions in icu patients (fundicu) project. Mycoses. 2019;62:310–9 Protocol of the FUNDICU project aimed at developing standard definitions for invasive fungal diseases in critically ill patients.
de Ruiter J, Weel J, Manusama E, Kingma WP, van der Voort PH. The epidemiology of intra-abdominal flora in critically ill patients with secondary and tertiary abdominal sepsis. Infection. 2009;37:522–7.
Dupont H, Bourichon A, Paugam-Burtz C, Mantz J, Desmonts JM. Can yeast isolation in peritoneal fluid be predicted in intensive care unit patients with peritonitis? Crit Care Med. 2003;31:752–7.
Lee SC, Fung CP, Chen HY, Li CT, Jwo SC, Hung YB, et al. Candida peritonitis due to peptic ulcer perforation: incidence rate, risk factors, prognosis and susceptibility to fluconazole and amphotericin b. Diagn Microbiol Infect Dis. 2002;44:23–7.
Leon C, Ruiz-Santana S, Saavedra P, Almirante B, Nolla-Salas J, Alvarez-Lerma F, et al. A bedside scoring system (“candida score”) for early antifungal treatment in nonneutropenic critically ill patients with candida colonization. Crit Care Med. 2006;34:730–7.
Leon C, Ruiz-Santana S, Saavedra P, Galvan B, Blanco A, Castro C, et al. Usefulness of the “candida score” for discriminating between candida colonization and invasive candidiasis in non-neutropenic critically ill patients: a prospective multicenter study. Crit Care Med. 2009;37:1624–33.
Ostrosky-Zeichner L. New approaches to the risk of candida in the intensive care unit. Curr Opin Infect Dis. 2003;16:533–7.
Pittet D, Monod M, Suter PM, Frenk E, Auckenthaler R. Candida colonization and subsequent infections in critically ill surgical patients. Ann Surg. 1994;220:751–8.
Eggimann P, Pittet D. Candida colonization index and subsequent infection in critically ill surgical patients: 20 years later. Intensive Care Med. 2014;40:1429–48.
Martin-Loeches I, Antonelli M, Cuenca-Estrella M, Dimopoulos G, Einav S, De Waele JJ, et al. Esicm/escmid task force on practical management of invasive candidiasis in critically ill patients. Intensive Care Med. 2019;45:789–805. https://doi.org/10.1007/s00134-019-05599-w.
Perlin DS. Echinocandin resistance in candida. Clin Infect Dis. 2015;61(Suppl 6):S612–7.
Grau S, Luque S, Campillo N, Samso E, Rodriguez U, Garcia-Bernedo CA, et al. Plasma and peritoneal fluid population pharmacokinetics of micafungin in post-surgical patients with severe peritonitis. J Antimicrob Chemother. 2015;70:2854–61.
Lempers VJ, Schouten JA, Hunfeld NG, Colbers A, van Leeuwen HJ, Burger DM, et al. Altered micafungin pharmacokinetics in intensive care unit patients. Antimicrob Agents Chemother. 2015;59:4403–9.
Muilwijk EW, Schouten JA, van Leeuwen HJ, van Zanten AR, de Lange DW, Colbers A, et al. Pharmacokinetics of caspofungin in icu patients. J Antimicrob Chemother. 2014;69:3294–9.
Sinnollareddy MG, Roberts JA, Lipman J, Akova M, Bassetti M, De Waele JJ, et al. Pharmacokinetic variability and exposures of fluconazole, anidulafungin, and caspofungin in intensive care unit patients: data from multinational defining antibiotic levels in intensive care unit (dali) patients study. Crit Care. 2015;19:33.
Dupont H, Massias L, Jung B, Ammenouche N, Montravers P. Pharmacokinetic study of anidulafungin in icu patients with intra-abdominal candidiasis. J Antimicrob Chemother. 2017;72:1429–32.
Dagens A, Mughal N, Sisson A, Moore LSP. Experience of using beta-d-glucan assays in the intensive care unit. Crit Care. 2018;22:125.
Donato L, Gonzalez T, Canales M, Legarraga P, Garcia P, Rabagliati R. the 1,3-beta-d-glucan in critical adult patients as diagnostic tool for invasive Candida spp. Infection, performance evaluation. Rev Chil Infectol. 2017;34:340–6 Evaluación del rendimiento de 1,3-β-d-glucano como apoyo diagnóstico de infecciones invasoras por Candida spp. en pacientes críticos adultos.
Mikulska M, Giacobbe DR, Furfaro E, Mesini A, Marchese A, Del Bono V, et al. Lower sensitivity of serum (1,3)-beta-d-glucan for the diagnosis of candidaemia due to Candida parapsilosisClin Microbiol Infect. 2016;22:646.e5–8.
Nucci M, Nouer SA, Esteves P, Guimaraes T, Breda G, de Miranda BG, et al. Discontinuation of empirical antifungal therapy in icu patients using 1,3-beta-d-glucan. J Antimicrob Chemother. 2016;71:2628–33.
Ostrosky-Zeichner L, Alexander BD, Kett DH, Vazquez J, Pappas PG, Saeki F, et al. Multicenter clinical evaluation of the (1-->3) beta-d-glucan assay as an aid to diagnosis of fungal infections in humans. Clin Infect Dis. 2005;41:654–9.
Posteraro B, Tumbarello M, De Pascale G, Liberto E, Vallecoccia MS, De Carolis E, et al. (1,3)-beta-d-glucan-based antifungal treatment in critically ill adults at high risk of candidaemia: An observational study. J Antimicrob Chemother. 2016;71:2262–9.
Talento AF, Dunne K, Joyce EA, Palmer M, Johnson E, White PL, et al. A prospective study of fungal biomarkers to improve management of invasive fungal diseases in a mixed specialty critical care unit. J Crit Care. 2017;40:119–27.
Tissot F, Lamoth F, Hauser PM, Orasch C, Fluckiger U, Siegemund M, et al. Beta-glucan antigenemia anticipates diagnosis of blood culture-negative intraabdominal candidiasis. Am J Respir Crit Care Med. 2013;188:1100–9.
Duettmann W, Koidl C, Krause R, Lackner G, Woelfler A, Hoenigl M. Specificity of mannan antigen and anti-mannan antibody screening in patients with haematological malignancies at risk for fungal infection. Mycoses. 2016;59:374–8.
Mikulska M, Calandra T, Sanguinetti M, Poulain D, Viscoli C, Third European G. Conference on infections in leukemia. The use of mannan antigen and anti-mannan antibodies in the diagnosis of invasive candidiasis: recommendations from the third european conference on infections in leukemia. Crit Care. 2010;14:R222.
Prella M, Bille J, Pugnale M, Duvoisin B, Cavassini M, Calandra T, et al. Early diagnosis of invasive candidiasis with mannan antigenemia and antimannan antibodies. Diagn Microbiol Infect Dis. 2005;51:95–101.
Sendid B, Poirot JL, Tabouret M, Bonnin A, Caillot D, Camus D, et al. Combined detection of mannanaemia and antimannan antibodies as a strategy for the diagnosis of systemic infection caused by pathogenic candida species. J Med Microbiol. 2002;51:433–42.
Verduyn Lunel FM, Donnelly JP, van der Lee HA, Blijlevens NM, Verweij PE. Circulating candida-specific anti-mannan antibodies precede invasive candidiasis in patients undergoing myelo-ablative chemotherapy. Clin Microbiol Infect. 2009;15:380–6.
Leon C, Ruiz-Santana S, Saavedra P, Castro C, Loza A, Zakariya I, et al. Contribution of candida biomarkers and DNA detection for the diagnosis of invasive candidiasis in icu patients with severe abdominal conditions. Crit Care. 2016;20:149.
Clancy CJ, Nguyen MH. Non-culture diagnostics for invasive candidiasis: Promise and unintended consequences. J Fungi (Basel). 2018;4:7.
Martinez-Jimenez MC, Munoz P, Guinea J, Valerio M, Alonso R, Escribano P, et al. Potential role of candida albicans germ tube antibody in the diagnosis of deep-seated candidemia. Med Mycol. 2014;52:270–5.
Martinez-Jimenez MC, Munoz P, Valerio M, Vena A, Guinea J, Bouza E. Combination of candida biomarkers in patients receiving empirical antifungal therapy in a spanish tertiary hospital: a potential role in reducing the duration of treatment. J Antimicrob Chemother. 2016;71:2679.
Parra-Sanchez M, Zakariya-Yousef Breval I, Castro Mendez C, Garcia-Rey S, Loza Vazquez A, Ubeda Iglesias A, et al. Candida albicans germ-tube antibody: evaluation of a new automatic assay for diagnosing invasive candidiasis in icu patients. Mycopathologia. 2017;182:645–52.
Wei S, Wu T, Wu Y, Ming D, Zhu X. Diagnostic accuracy of candida albicans germ tube antibody for invasive candidiasis: systematic review and meta-analysis. Diagn Microbiol Infect Dis. 2019;93:339–45.
Giacobbe DR, Mikulska M, Tumbarello M, Furfaro E, Spadaro M, Losito AR, et al. Combined use of serum (1,3)-beta-d-glucan and procalcitonin for the early differential diagnosis between candidaemia and bacteraemia in intensive care units. Crit Care. 2017;21:176.
Martinez-Jimenez MC, Munoz P, Valerio M, Alonso R, Martos C, Guinea J, et al. Candida biomarkers in patients with candidaemia and bacteraemia. J Antimicrob Chemother. 2015;70:2354–61.
Avni T, Leibovici L, Paul M. Pcr diagnosis of invasive candidiasis: systematic review and meta-analysis. J Clin Microbiol. 2011;49:665–70.
Chang SS, Hsieh WH, Liu TS, Lee SH, Wang CH, Chou HC, et al. Multiplex pcr system for rapid detection of pathogens in patients with presumed sepsis—a systemic review and meta-analysis. PLoS One. 2013;8:e62323.
Desmet S, Maertens J, Bueselinck K, Lagrou K. Broad-range pcr coupled with electrospray ionization time of flight mass spectrometry for detection of bacteremia and fungemia in patients with neutropenic fever. J Clin Microbiol. 2016;54:2513–20.
White PL, Hibbitts SJ, Perry MD, Green J, Stirling E, Woodford L, et al. Evaluation of a commercially developed semiautomated pcr-surface-enhanced raman scattering assay for diagnosis of invasive fungal disease. J Clin Microbiol. 2014;52:3536–43.
Bassetti M, Righi E, Montravers P, Cornely OA. What has changed in the treatment of invasive candidiasis? A look at the past 10 years and ahead. J Antimicrob Chemother. 2018;73:i14–25.
Arendrup MC, Andersen JS, Holten MK, Krarup KB, Reiter N, Schierbeck J, et al. Diagnostic performance of T2Candida among ICU patients with risk factors for invasive candidiasis. Open Forum Infect Dis. 2019;6:ofz136.
Bouza E, Vena A, Munoz P, T. M. s. group. T2Candida MR as a predictor of outcome in patients with suspected invasive candidiasis starting empirical antifungal treatment: a prospective pilot study–authors' response. J Antimicrob Chemother. 2019;74:533–4.
Giannella M, Paolucci M, Roncarati G, Vandi G, Pascale R, Trapani F, et al. Potential role of t2candida in the management of empirical antifungal treatment in patients at high risk of candidaemia: a pilot single-Centre study. J Antimicrob Chemother. 2018;73:2856–9.
Munoz P, Vena A, Machado M, Gioia F, Martinez-Jimenez MC, Gomez E, et al. T2Candida MR as a predictor of outcome in patients with suspected invasive candidiasis starting empirical antifungal treatment: a prospective pilot study. J Antimicrob Chemother. 2018;73:iv6–iv12.
Clancy CJ, Nguyen MH. T2 magnetic resonance for the diagnosis of bloodstream infections: charting a path forward. J Antimicrob Chemother. 2018;73:iv2–5.
Mylonakis E, Clancy CJ, Ostrosky-Zeichner L, Garey KW, Alangaden GJ, Vazquez JA, et al. T2 magnetic resonance assay for the rapid diagnosis of candidemia in whole blood: a clinical trial. Clin Infect Dis. 2015;60:892–9.
Cuenca-Estrella M, Verweij PE, Arendrup MC, Arikan-Akdagli S, Bille J, Donnelly JP, et al. Escmid* guideline for the diagnosis and management of candida diseases 2012: diagnostic procedures. Clin Microbiol Infect. 2012;18(Suppl 7):9–18.
Bailly S, Leroy O, Montravers P, Constantin JM, Dupont H, Guillemot D, et al. Antifungal de-escalation was not associated with adverse outcome in critically ill patients treated for invasive candidiasis: post hoc analyses of the AmarCAND2 study data. Intensive Care Med. 2015;41:1931–40.
Vazquez J, Reboli AC, Pappas PG, Patterson TF, Reinhardt J, Chin-Hong P, et al. Evaluation of an early step-down strategy from intravenous anidulafungin to oral azole therapy for the treatment of candidemia and other forms of invasive candidiasis: results from an open-label trial. BMC Infect Dis. 2014;14:97.
Koperna T, Schulz F. Relaparotomy in peritonitis: prognosis and treatment of patients with persisting intraabdominal infection. World J Surg. 2000;24:32–7.
Seiler CA, Brugger L, Forssmann U, Baer HU, Buchler MW. Conservative surgical treatment of diffuse peritonitis. Surgery. 2000;127:178–84.
Azuhata T, Kinoshita K, Kawano D, Komatsu T, Sakurai A, Chiba Y, et al. Time from admission to initiation of surgery for source control is a critical determinant of survival in patients with gastrointestinal perforation with associated septic shock. Crit Care. 2014;18:R87.
Bloos F, Ruddel H, Thomas-Ruddel D, Schwarzkopf D, Pausch C, Harbarth S, et al. Effect of a multifaceted educational intervention for anti-infectious measures on sepsis mortality: a cluster randomized trial. Intensive Care Med. 2017;43:1602–12.
Martin-Loeches I, Timsit JF, Leone M, de Waele J, Sartelli M, Kerrigan S, et al. Clinical controversies in abdominal sepsis. Insights for critical care settings. J Crit Care. 2019;53:53–8.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43:304–77.
Eggimann P, Francioli P, Bille J, Schneider R, Wu MM, Chapuis G, et al. Fluconazole prophylaxis prevents intra-abdominal candidiasis in high-risk surgical patients. Crit Care Med. 1999;27:1066–72.
Khoury W, Szold O, Soffer D, Kariv Y, Wasserlauf R, Klausner JM, et al. Prophylactic fluconazole does not improve outcome in patients with purulent and fecal peritonitis due to lower gastrointestinal perforation. Am Surg. 2010;76:197–202.
Senn L, Eggimann P, Ksontini R, Pascual A, Demartines N, Bille J, et al. Caspofungin for prevention of intra-abdominal candidiasis in high-risk surgical patients. Intensive Care Med. 2009;35:903–8.
•• Cortegiani A, Russotto V, Maggiore A, Attanasio M, Naro AR, Raineri SM, et al. Antifungal agents for preventing fungal infections in non-neutropenic critically ill patients. Cochrane Database Syst Rev. 2016;2016(1):CD004920. https://doi.org/10.1002/14651858.CD004920Comprehensive systematic review about the role of antifungal prophylaxis in non-neutropenic critically ill patients.
Cruciani M, de Lalla F, Mengoli C. Prophylaxis of candida infections in adult trauma and surgical intensive care patients: a systematic review and meta-analysis. Intensive Care Med. 2005;31:1479–87.
Playford EG, Webster AC, Sorrell TC, Craig JC. Antifungal agents for preventing fungal infections in non-neutropenic critically ill and surgical patients: systematic review and meta-analysis of randomized clinical trials. J Antimicrob Chemother. 2006;57:628–38.
Shorr AF, Chung K, Jackson WL, Waterman PE, Kollef MH. Fluconazole prophylaxis in critically ill surgical patients: a meta-analysis. Crit Care Med. 2005;33:1928–35 quiz 36.
Vardakas KZ, Samonis G, Michalopoulos A, Soteriades ES, Falagas ME. Antifungal prophylaxis with azoles in high-risk, surgical intensive care unit patients: a meta-analysis of randomized, placebo-controlled trials. Crit Care Med. 2006;34:1216–24.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Outside the submitted work, MB has participated in advisory boards and/or received speaker honoraria from Achaogen, Angelini, Astellas, Bayer, Basilea, BioMérieux, Cidara, Gilead, Menarini, MSD, Nabriva, Paratek, Pfizer, Roche, Melinta, Shionogi, Tetraphase, VenatoRx, and Vifor and has received study grants from Angelini, Basilea, Astellas, Shionogi, Cidara, Melinta, Gilead, Pfizer, and MSD. Outside the submitted work, DRG reports honoraria from Stepstone Pharma GmbH and an unconditional grant from MSD Italia. The other authors have no conflicts of interest to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by either of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Intra-Abdominal Infections, Hepatitis and Gastroenteritis
Rights and permissions
About this article
Cite this article
Bassetti, M., Vena, A., Pincino, R. et al. Role of Antifungal Therapy in Complicated Intra-abdominal Infections. Curr Infect Dis Rep 22, 21 (2020). https://doi.org/10.1007/s11908-020-00731-0
Published:
DOI: https://doi.org/10.1007/s11908-020-00731-0