Abstract
Purpose of Review
Pre-exposure prophylaxis (PrEP) represents one of the most effective methods of prevention for HIV, but remains inequitable, leaving many transgender and nonbinary (trans) individuals unable to benefit from this resource. Deploying community-engaged PrEP implementation strategies for trans populations will be crucial for ending the HIV epidemic.
Recent Findings
While most PrEP studies have progressed in addressing pertinent research questions about gender-affirming care and PrEP at the biomedical and clinical levels, research on how to best implement gender-affirming PrEP systems at the social, community, and structural levels remains outstanding.
Summary
The science of community-engaged implementation to build gender-affirming PrEP systems must be more fully developed. Most published PrEP studies with trans people report on outcomes rather than processes, leaving out important lessons learned about how to design, integrate, and implement PrEP in tandem with gender-affirming care. The expertise of trans scientists, stakeholders, and trans-led community organizations is essential to building gender-affirming PrEP systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Designing gender-affirming PrEP systems goes beyond simply integrating gender-affirming care and PrEP services – it starts with partnerships with transgender scientists, stakeholders, trans-led community organizations, and community members at large.
Introduction
A decade after Truvada as oral HIV pre-exposure prophylaxis (PrEP, tenofovir disoproxil/emtricitabine) was approved in 2012 by the U.S. Food and Drug Administration (FDA) for public use [1], multiple interventions and programs have demonstrated PrEP’s effectiveness to curb HIV incidence. Since then, three new major advancements were made in PrEP formulation and delivery. In particular, the Descovy formulation of PrEP (emtricitabine/tenofovir alafenamide) was evaluated for safety and efficacy in 2019. It received FDA approval and provided a second oral PrEP option for some adults and adolescents, but importantly, people assigned female at birth were excluded from the clinical research on Descovy, resulting in the FDA’s limited approval of Descovy for people assigned male at birth only [2]. More recently approved in 2021, Apretude (cabotegravir extended-release injectable suspension) became the first long-acting injectable (LAI) option that makes it possible to take PrEP every 2 months instead of in a daily pill form, but again, this option has transgender-specific limitations, as transmasculine people were not included in the clinical trials [3]. Lastly, as an alternative to daily oral PrEP, “on-demand” or 2–1-1 PrEP, which follows an arranged schedule of taking two Truvada pills 2 to 24 ho before sex, one pill 24 h after the first dose, and another pill 24 h after the second dose, is currently endorsed by the Centers for Disease Control and Prevention (CDC) to be taken only when “at-risk” for HIV [4], and with studies demonstrating its efficacy and effectiveness, yet largely conducted in cisgender populations [5,6,7]. These are monumental and promising advances in the HIV prevention landscape and the broader mission to improve the health of communities and end HIV/AIDS around the world. However, their reach is limited among communities of transgender and nonbinary (trans) people, due to the ongoing underrepresentation of these communities in PrEP research and implementation globally.
Trans populations are diverse and include communities of transfeminine, transmasculine, and nonbinary individuals [8, 9••].Footnote 1 Trans communities face ubiquitous stigma, cissexism, and discrimination across all socio-ecological domains, including persistent structural efforts to delegitimize their gender identities and rights to access care, in addition to a dearth of comprehensive gender-affirming providers and services [10, 11]. These social and structural vulnerabilities place transgender and nonbinary communities at elevated risk for adverse behavioral and health outcomes, which further perpetuate to HIV inequities in this population [9••]. One recent study reported that transfeminine individuals, particularly those in the USA, have an estimated HIV prevalence of 14.1% [12••]. While existing data are scarce as a result of gender-blind surveillance systems [13], the limited data on transmasculine and nonbinary individuals who have sex with men show alarmingly high HIV incidence and prevalence as well [12••, 14]. Notably, the inequity in HIV prevalence is even more pronounced among minoritized ethnoracial groups [12••], within the trans community with estimates for HIV prevalence among Black, Indigenous, and Latine transgender women being substantially high [12••]. And community-led advocacy, research, and structural interventions that aim to promote HIV prevention interventions, including PrEP use, adherence, and persistence, must recognize the pressing need for equitable and transformative HIV prevention strategies that are rooted in and led by transgender and nonbinary communities [15,16,17,18].
Inequities in Designing PrEP Studies with Trans Populations
Despite a wide diversity of gender identities and expression, PrEP research has largely focused on transfeminine adults. While this focus on transfeminine adults is likely due to the epidemiological evidence of high HIV burden among transfeminine individuals, it also reflects a paradigm in clinical research in which trans communities are perceived as ancillary to other key communities placed at risk [13, 19]. A 2021 scoping review focusing specifically on trans populations examined 667 HIV prevention articles that sampled at least one trans participant based on assigned sex at birth found that “38.5% subsumed transgender participants into cisgender populations (most frequently combining trans women with cisgender men who have sex with men), 20.4% compared transgender and cisgender participants, and 41.1% focused exclusively on transgender women” [20••]. While this review is aimed at comprehensively providing an overview for all trans groups, data extracted were only able to delineate the inclusion of transfeminine adults in HIV studies and were unable to distinguish transmasculine and nonbinary people. To date, few reviews have been conducted to delineate the participation of either transmasculine or nonbinary individuals in HIV or PrEP studies [21], reflective of the erasure and lack of gender-inclusive approaches in PrEP studies and in the broader HIV landscape.
While there have been improvements in including transfeminine adults in PrEP and HIV research and programming, glaring intersecting gender and racial inequities remain. The inclusion of transgender and nonbinary individuals in implementation research, clinical trials, and community engagement has remained at best, scant, despite the growing number of transgender and nonbinary communities in the USA [12••]. Globally, particularly in the global south where community engagement and leadership with trans advocates have gained more prominence, PrEP programming and HIV surveillance systems are only now beginning to implement changes and correct systematic practices that subsumed trans populations into other key populations [22, 23]. And while PrEP studies and HIV surveillances have relied on sex assigned at birth as part of eligibility criteria as well as to identify trans individuals in primary data collection and in existing databases, such an approach not only disregards the diversity in trans identities but also complicates and furthers data misrepresentation rendering some to the point of invisibility, where the true burden of need remains unknown. This further limits any understanding of ethno-racial differences within subgroups of trans communities, where health inequities [24••], including HIV has been documented [25]. Trans and HIV scholars have recommended designing studies with self-reported demographic data on gender identity or trans status to be the preferred method for measuring and identifying trans populations in studies and surveillance systems, and for conducting research with trans communities [9••, 26••].
Persistence for Gender-Affirmative PrEP Systems and Trans Engagement
Advancements in PrEP have scarcely included, prioritized, or positioned trans people as stakeholders, as scientists, as partners with trans-led community-based organizations, and as we noted above, not even as research participants. This exclusion is due to the pervasiveness of cissexism and cisnormativity that leads to erasure in research and public health programming at-large that researchers—both cis and trans—reinforce and uphold [18, 27••]. Many have begun working to heal relationships between trans communities, HIV research, and scientific communities through community-engaged research and programmatic interventions [28,29,30,31,32,33,34], but much more work is needed [35]. Several trans and nonbinary scientists and community scholars working within spaces of HIV prevention have recurrently advocated for HIV prevention research and programming to be conducted with them across all stages of research development, implementation, and dissemination [17, 32].
Specifically, there has been a persistent demand by trans people for PrEP programmers to design and implement gender-affirmative PrEP systems [16]. Gender-affirmative PrEP systems necessitate for trans people to receive the necessary PrEP care continuum services [36] while also highly valuing and ensuring that trans people’s gender identity and treatment goals are medically, socially, and structurally recognized and supported—to maximize the benefits of PrEP within trans communities directly [15, 37]. In the context of HIV care, this includes the critical and comprehensive integration of HIV care with gender-affirming health services, which has been shown to improve engagement and retention for achieving viral suppression [38,39,40]. There have been some efforts to implement and evaluate gender-affirmative PrEP programs in existing healthcare settings [29, 41]; however, additional efforts are warranted to address PrEP barriers across the personal/biological, social, structural socio-ecological levels. Specifically, the transformation of health care settings towards gender-affirming warrants the implementation of policies in different geographic locales that eliminate HIV criminalization as well as bans or restrictions to legal affirmation, such as name and gender marker changes both in government-issued identification documents and electronic medical records [42]. For example, the Trans Renaming Project in Detroit, Michigan, a community-led initiative, is aimed at improving access to legal affirmation and address social and legal barriers that contribute to HIV inequities and inaccessibility to PrEP and HIV prevention services for trans communities locally [34, 43].
At the biomedical level, formative research has been conducted with transfeminine adults to examine PrEP efficacy along with gender-affirming hormones. Specifically, concerns for lowered efficacy and drug-drug interactions between PrEP and gender-affirming hormones have been documented, both from the perspectives of providers and trans community members [44, 45]. To address this concern, several pharmacological studies have examined the impact of PrEP on hormones and vice versa [45,46,47]. One pharmacological clinical trial with Thai transfeminine adults offers clarity showing that estrogen hormones do not lower PrEP efficacy in a clinically significant way and that estrogen levels were not affected by PrEP [48]. In a recent double-blind noninferiority trial with transfeminine adults, findings demonstrated that blood-level concentration of two types of PrEP formulation (emtricitabine and tenofovir alafenamide (F/TAF) versus emtricitabine and tenofovir disoproxil fumarate (F/TDF)) remained efficacious and were not negatively impacted by gender-affirming hormones [49]. However, studies on the efficacies and effectiveness of taking both gender-affirming hormones with other important PrEP modalities such as long-acting injectable PrEP and 2–1-1 are underexamined. Despite this limitation, some expert opinions convey that there are no expected drug-to-drug interactions between gender-affirming hormones and PrEP, and though more studies are needed, authors recommended to continue offering PrEP for trans communities given studies showing the reach of protective concentrations [45]. Scholars have also noted the need to train PrEP providers to utilize gender-affirming rhetoric and adopt a personalized medicine approach when prescribing gender-affirming care with PrEP [50]. This approach not only allows for providers to monitor and ensure that PrEP and hormone blood levels remain safe but also to align and meet patients’ PrEP and other HIV services needs with their gender affirmation goals [50].
At the clinic-level, a select few US- and international-based demonstration projects have shown some promising successes in implementing the integration of gender-affirming care with PrEP services, with the majority primarily designed to increase PrEP uptake among transfeminine adults in community-based health clinic settings. For example, researchers at Callen Lorde Community Health Center in New York City, an LGBTQ-focused health center that specializes in the integration of PrEP, gender-affirming care, as well as insurance and payment services, recently published a longitudinal study that showed PrEP adherence was high (greater than 90%) at 3 and 6 months after initiation both in self-report and urine assay data collection among 80% of the 100 enrolled transfeminine patients [51]. In Atlanta, a patient-centered PrEP program designed with a co-located gender clinic offering affordable comprehensive primary care, gender-affirming hormone, and mental health services showed high rates of linkage to PrEP care, prescription, and initiation among transfeminine participants. In Thailand, key population-led health service programming that offers same-day PrEP and is delivered by trained key population community health workers, including transgender lay providers, contributed to 82% current Thai PrEP users and highlighted adherence and retention as high-priority research areas for scale-up of the program [29, 52]. In addition, the Tangerine Clinic in Thailand introduced the “Integrated Trans Model,” which was disseminated to three other Asian countries using implementation strategies informed by community leaders and resulted in PrEP linkages ranged from 20 to 27% [53]. In the Philippines, community-based organizations and trans community leaders are building out grassroots community outreach, infrastructure, and organizational capacity for ongoing gender affirming care, PrEP and HIV research clinics, including offering in-person and telehealth services, training health care workforce, organizing community events, and building formal coalitions such as the Philippine Professional Association for Transgender Health to improve gender-affirming care as well as combat recent surges in HIV incidence [54]. Similarly in South Africa, scaling up of PrEP clinics are underway with aims to provide comprehensive care in addition to PrEP for transgender women, with results under review at the time of this review [55]. To our team’s knowledge, only one study in California has been inclusive of transmasculine and nonbinary communities and demonstrated high levels of PrEP initiation across gender identities; however, gender differences were found in adherence to daily oral PrEP such that transfeminine adults were more likely to have protective drug levels compared to transmasculine and nonbinary adults [41]. As such, future research is warranted to develop and implement gender-affirming PrEP programs that addresses barriers across the PrEP cascade.
Recommendations for Community-Engaged Gender-Affirming PrEP Systems
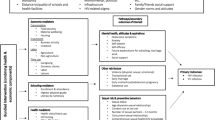
Envisioning what gender-affirming PrEP systems look like across other socio-ecological levels remains underdeveloped. Published PrEP studies typically report on outcomes rather than processes. As a step to fill this gap, we turn to documented strategies drawn from the literature, and when possible, leaned on our expertise as trans stakeholders, leaders of trans-led community organizations, and as communities of trans and cis scholars in the fields of trans health and HIV prevention to map (in Fig. 1) and synthesize the following recommendations (in Table 1).
Conclusion
Despite the development of multiple PrEP formulations now available for delivery, trans people experience suboptimal benefits due to low community engagement resulting in inequitable access and uptake of this medication. The expertise of trans people has not been adequately incorporated into the design of PrEP education and promotion campaigns. The complex health needs of trans communities have not been sufficiently consulted in the implementation of PrEP delivery systems. Consequently, trans communities continue to suffer disproportionately from the unnecessary and preventable burden of new HIV infections. This inequity must be remedied.
Meaningful and sustained investments in partnerships with trans community members are essential to mitigating widening inequities of HIV burden that disproportionately affect trans people worldwide. Specific actions are as follows: (i) recognize transmasculine and nonbinary individuals (i.e., not just transfeminine individuals) as priorities for PrEP programming; (ii) bring visibility to similarities and differences in gender-affirmation needs across the spectrum of gender minority groups by distinguishing gender-inclusive and gender-specific approaches in designing PrEP delivery systems (19); (iii) address social determinants of HIV within trans populations including—but not limited to—the role of employment, insurance, housing, legal factors that shape the ability for trans people to achieve optimal health; (iv) include trans scholars and scientists in positions of leadership in future PrEP research and programming efforts.
Notes
Transfeminine is a gender identity that describes people who were assigned male sex at birth and now with a gender identity within the transfeminine spectrum (e.g., trans women, women), and transmasculine is a gender identity that describes people who were assigned female sex at birth and now with gender identity within the transmasculine spectrum (e.g., trans men, men). And nonbinary describes people whose gender identities do not conform with the gender binary.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Centers for Disease Control Prevention. Interim guidance for clinicians considering the use of preexposure prophylaxis for the prevention of HIV infection in heterosexually active adults. MMWR Morb Mortal Wkly Rep. 2012;61(31):586–9.
US Food and Drug Administration. FDA approves second drug to prevent HIV infection as part of ongoing efforts to end the HIV epidemic. FDA News Release. Available at: https://www.fda.gov/news-events/press-announcements/fda-approves-second-drug-prevent-hiv-infection-part-ongoing-efforts-end-hiv-epidemic . Accessed date: January 14, 20232019.
US Food and Drug Administration. FDA approves first injectable treatment for HIV pre-exposure prevention. 2019. FDA News Release. Available at: https://www.fda.gov/news-events/press-announcements/fda-approves-first-injectable-treatment-hiv-pre-exposure-prevention . Accessed Date: January 14, 2023.2019.
Centers for Disease Control Prevention. Pre-exposure prophylaxis for the prevention of HIV infection in the United States - 2021 update. Available at: https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf . Accessed Date: January 14, 20232021.
Molina J, Ghosn J, Béniguel L, Rojas-Castro D, Algarte-Genin M, Pialoux G. Incidence of HIV-infection in the ANRS Prevenir study in Paris region with daily or on-demand PrEP with TDF/FTC. Age (years). 2018;36:30–44.
Molina J-M, Charreau I, Spire B, Cotte L, Chas J, Capitant C, et al. Efficacy, safety, and effect on sexual behaviour of on-demand pre-exposure prophylaxis for HIV in men who have sex with men: an observational cohort study. The lancet HIV. 2017;4(9):e402–10.
Zhang J, Xu JJ, Wang HY, Huang XJ, Chen YK, Wang H, et al. Preference for daily versus on-demand pre-exposure prophylaxis for HIV and correlates among men who have sex with men: the China Real-world Oral PrEP Demonstration study. J Int AIDS Soc. 2021;24(2):e25667.
James S, Herman J, Rankin S, Keisling M, Mottet L, Anafi Ma. The report of the 2015 US transgender survey. 2016.
Scheim AI, Baker KE, Restar AJ, Sell RL. Health and health care among transgender adults in the United States. Annual Review of Public Health. 2022;43:503–23. This article summarizes the multiple healthcare disparities and inequities documented among trans populations in the US.
Goldenberg T. Health care use among transgender and other gender diverse people in the United States: influences of stigma and resilience 2019.
Hughto JMW, Reisner SL, Pachankis JE. Transgender stigma and health: a critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med. 2015;147:222–31.
Becasen JS, Denard CL, Mullins MM, Higa DH, Sipe TA. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and meta-analysis, 2006–2017. American journal of public health. 2019;109(1):e1-e8. This article is a meta-analysis of lab-confirmed HIV results among trans populations in the city, stratified by race/ethnicity.
Tordoff DM, Minalga B, Gross BB, Martin A, Caracciolo B, Barbee LA, et al. Erasure and health equity implications of using binary male/female categories in sexual health research and human immunodeficiency virus/sexually transmitted infection surveillance: recommendations for transgender-inclusive data collection and reporting. Sex Transm Dis. 2022;49(2):e45–9.
McNulty A, Bourne C. Transgender HIV and sexually transmissible infections. Sexual Health. 2017;14(5):451–5.
Minalga B, Chung C, Davids J, Martin A, Perry NL, Shook A. Research on transgender people must benefit transgender people. The Lancet. 2022;399(10325):628.
Operario D, Restar A. Gender-affirmative systems needed for PrEP implementation. The Lancet HIV. 2020;7(12):e799–800.
Scheim AI, Appenroth MN, Beckham SW, Goldstein Z, Grinspan MC, Keatley JG, et al. Transgender HIV research: nothing about us without us. The Lancet HIV. 2019;6(9):e566–7.
Adimora AA, Auerbach JD. Structural interventions for HIV prevention in the United States. J Acquir Immune Defic Syndr. 2010;55(0 2):S132.
Restar A, Jin H, Operario D. Gender-inclusive and gender-specific approaches in trans health research. Transgender Health. 2021;6(5):235–9.
Grant RM, Sevelius JM, Guanira JV, Aguilar JV, Chariyalertsak S, Deutsch MB. Transgender women in clinical trials of pre-exposure prophylaxis. Journal of acquired immune deficiency syndromes (1999). 2016;72(Suppl 3):S226. This is a sub-analysis of trans women’s involvement in one of the first PrEP clinical trials.
Dang M, Scheim AI, Teti M, Quinn KG, Zarwell M, Petroll AE, et al. Barriers and facilitators to HIV pre-exposure prophylaxis uptake, adherence, and persistence among transgender populations in the United States: a systematic review. AIDS Patient Care STDS. 2022;36(6):236–48.
Cloete A, Skinner D, van der Merwe L, Lynch I. Community-derived interventions can improve responsiveness to the HIV prevention needs of transgender women in South Africa. (Paper presented at the Satellite HIVR4P: Getting to the Heart of Stigma: Removing Stigma as Barrier and Enhancing HIV Prevention Efforts). 2021.
Van Der Merwe L, Mavhandu-Mudzusi A. S06. 1 The healthcare experiences of transgender women living with HIV in the Buffalo City Metro Municipality. BMJ Publishing Group Ltd; 2021.
Lett E, Abrams MP, Gold A, Fullerton F-A, Everhart A. Ethnoracial inequities in access to gender-affirming mental health care and psychological distress among transgender adults. Soc Psychiatry Psychiatr Epidemiol. 2022;57(5):963–71. This article applies an intersectionality framework to both premise and methodology to delineate the racial/ethnic differences of gender-affirming care and mental health outcomes among trans people.
Lett E, Asabor EN, Tran N, Dowshen N, Aysola J, Gordon AR, et al. Sexual behaviors associated with HIV transmission among transgender and gender diverse young adults: the intersectional role of racism and transphobia. AIDS Behav. 2022;1–13.
Restar A, Dusic E, Garrison-Desany H, Lett E, Everhart A, Baker KE, et al. Gender affirming hormone therapy dosing behaviors among transgender and nonbinary adults. Humanit Soc Sci Commun. 2022;9(1):1–11. This article documents the different dosing behaviors of gender affirming hormones among trans people, showing that not all trans people take or view hormones as part of their gender affirmation.
Bowleg L. “The master’s tools will never dismantle the master’s house”: ten critical lessons for Black and other health equity researchers of color. Health Educ Behav. 2021;48(3):237–49. This article discusses the key contexts on how to address pervasive oppressive systems of power perpetuate harms like cissexim and cisnormativity in the context of health equity research.
Wongkanya R, Pankam T, Wolf S, Pattanachaiwit S, Jantarapakde J, Pengnongyang S, et al. HIV rapid diagnostic testing by lay providers in a key population-led health service programme in Thailand. J Virus Erad. 2018;4(1):12–5.
Phanuphak N, Sungsing T, Jantarapakde J, Pengnonyang S, Trachunthong D, Mingkwanrungruang P, et al. Princess PrEP program: the first key population-led model to deliver pre-exposure prophylaxis to key populations by key populations in Thailand. Sexual health. 2018;15(6):542–55.
van Griensven F, Janamnuaysook R, Nampaisan O, Peelay J, Samitpol K, Mills S, et al. Uptake of primary care services and HIV and syphilis infection among transgender women attending the Tangerine Community Health Clinic, Bangkok, Thailand, 2016–2019. J Int AIDS Soc. 2021;24(6):e25683.
Gamarel KE, Rebchook G, McCree BM, Jadwin-Cakmak L, Connolly M, Reyes LA, et al. The ethical imperative to reduce HIV stigma through community-engaged, status-neutral interventions designed with and for transgender women of colour in the United States. J Int AIDS Soc. 2022;25:e25907.
Vannakit R, Janyam S, Linjongrat D, Chanlearn P, Sittikarn S, Pengnonyang S, et al. Give the community the tools and they will help finish the job: key population-led health services for ending AIDS in Thailand. J Int AIDS Soc. 2020;23(6).
Yang F, Janamnuaysook R, Boyd MA, Phanuphak N, Tucker JD. Key populations and power: people-centred social innovation in Asian HIV services. The Lancet HIV. 2020;7(1):e69–74.
Janamnuaysook R, Green KE, Seekaew P, Vu BN, Van Ngo H, Doan HA, et al. Demedicalisation of HIV interventions to end HIV in the Asia-Pacific. Sexual Health. 2021;18(1):13–20.
Cargill VA. Valuing the vulnerable–the important role of transgender communities in biomedical research. Ethn Dis. 2020;30(2):247.
Nunn AS, Brinkley-Rubinstein L, Oldenburg CE, Mayer KH, Mimiaga M, Patel R, et al. Defining the HIV pre-exposure prophylaxis care continuum. AIDS (London, England). 2017;31(5):731.
Sevelius JM, Deutsch MB, Grant R. The future of PrEP among transgender women: the critical role of gender affirmation in research and clinical practices. J Int AIDS Soc. 2016;19:21105.
Sevelius JM, Dilworth SE, Reback CJ, Chakravarty D, Castro D, Johnson MO, et al. Randomized controlled trial of healthy divas: a gender-affirming, peer-delivered intervention to improve hIV care engagement among transgender women living with HIV. J Acquir Immune Defic Syndr (1999). 2022.
Sevelius J, Chakravarty D, Neilands TB, Keatley J, Shade SB, Johnson MO, et al. Evidence for the model of gender affirmation: the role of gender affirmation and healthcare empowerment in viral suppression among transgender women of color living with HIV. AIDS Behav. 2021;25(1):64–71.
Bothma R, O’Connor C, Nkusi J, Shiba V, Segale J, Matsebula L, et al. Differentiated HIV services for transgender people in four South African districts: population characteristics and HIV care cascade. J Int AIDS Soc. 2022;25:e25987.
Sevelius JM, Glidden DV, Deutsch M, Welborn L, Contreras A, Salinas A, et al. Uptake, retention, and adherence to pre-exposure prophylaxis (PrEP) in TRIUMPH: a peer-led PrEP demonstration project for transgender communities in Oakland and sacramento, California. J Acquir Immune Defic Syndr. 2021;88(1):S27.
Harsono D, Galletly CL, O’Keefe E, Lazzarini Z. Criminalization of HIV exposure: a review of empirical studies in the United States. AIDS Behav. 2017;21(1):27–50.
Gamarel KE, Jadwin-Cakmak L, King WM, Hughes L, Abad J, Trammell R, et al. Improving access to legal gender affirmation for transgender women involved in the criminal–legal system. J Correct Health Care. 2022.
Anderson PL, Reirden D, Castillo-Mancilla J. Pharmacologic considerations for preexposure prophylaxis in transgender women. J Acquir Immune Defic Syndr. 2016;72(Suppl 3):S230.
Yager JL, Anderson PL. Pharmacology and drug interactions with HIV PrEP in transgender persons receiving gender affirming hormone therapy. Expert Opin Drug Metab Toxicol. 2020;16(6):463–74.
Mehrotra ML, Westreich D, McMahan VM, Glymour MM, Geng E, Grant RM, et al. Baseline characteristics explain differences in effectiveness of randomization to daily oral TDF/FTC PrEP between transgender women and cisgender men who have sex with men in the iPrEx trial. J Acquir Immune Defic Syndr. 2019;81(3):e94.
Grant RM, Pellegrini M, Defechereux PA, Anderson PL, Yu M, Glidden DV, et al. Sex hormone therapy and tenofovir diphosphate concentration in dried blood spots: primary results of the interactions between antiretrovirals and transgender hormones study. Clin Infect Dis. 2021;73(7):e2117–23.
Hiransuthikul A, Himmad L, Kerr SJ, Janamnuaysook R, Dalodom T, Phanjaroen K, et al. Drug-drug interactions among Thai transgender women living with human immunodeficiency undergoing feminizing hormone therapy and antiretroviral therapy: the iFACT Study. Clin Infect Dis. 2021;72(3):396–402.
Cespedes MS, Das M, Yager J, Prins M, Krznaric I, de Jong J, et al. Gender affirming hormones do not affect the exposure and efficacy of F/TDF or F/TAF for HIV preexposure prophylaxis: a subgroup analysis from the DISCOVER trial. Transgender Health. 2022.
Restar AJ, Santamaria EK, Adia A, Nazareno J, Chan R, Lurie M, et al. Gender affirmative HIV care framework: decisions on feminizing hormone therapy (FHT) and antiretroviral therapy (ART) among transgender women. PLoS One. 2019;14(10):e0224133.
Starbuck L, Golub SA, Klein A, Harris AB, Guerra A, Rincon C, et al. Brief report: transgender women and preexposure prophylaxis care: high preexposure prophylaxis adherence in a real-world health care setting in New York City. JAIDS J Acquir Immune Defic Syndr. 2022;90(1):15–9.
Lertpiriyasuwat C, Jiamsiri S, Tiramwichanon R, Langkafah F, Prommali P, Srikhamjean Y, et al. Thailand national PrEP program: moving towards sustainability. The 24th International AIDS Conference: AIDS 2022; Montreal, Canda2022.
Janamnuaysook R, Samitpol K, Getwongsa P, Srimanus P, Aung M, Oo H, et al. Integrating gender-affirming care into HIV services for transgender women in three Asian countries: an implementation opportunity using Rogers’ diffusion of innovation theory. The 24th International AIDS Conference: AIDS 2022; Montreal, Canda2022.
Quilantang M, Irene N, Bermudez ANC, Operario D. Reimagining the future of HIV service implementation in the Philippines based on lessons from COVID-19. AIDS Behav. 2020;24(11):3003–5.
Poteat T, Malik M, van der Merwe LLA, Cloete A, Adams D, Nonyane BA, et al. PrEP awareness and engagement among transgender women in South Africa: a cross-sectional, mixed methods study. The Lancet HIV. 2020;7(12):e825–34.
Baum F, MacDougall C, Smith D. Participatory action research. J Epidemiol Community Health. 2006;60(10):854.
De Lew N, Sommers BD, editors. Addressing social determinants of health in federal programs. JAMA Health Forum; 2022: Am Med Assoc.
Regenstein M, Trott J, Williamson A, Theiss J. Addressing social determinants of health through medical-legal partnerships. Health Aff. 2018;37(3):378–85.
Yamanis TJ, Zea MC, RaméMontiel AK, Barker SL, Díaz-Ramirez MJ, Page KR, et al. Immigration legal services as a structural HIV intervention for Latinx sexual and gender minorities. J Immigr Minor Health. 2019;21(6):1365–72.
Wesp LM, Malcoe LH, Elliott A, Poteat T. Intersectionality research for transgender health justice: a theory-driven conceptual framework for structural analysis of transgender health inequities. Transgender health. 2019;4(1):287–96.
Lacombe-Duncan A, Jadwin-Cakmak L, Trammell R, Burks C, Rivera B, Reyes L, et al. “… Everybody else is more privileged. Then it’s us…”: a qualitative study exploring community responses to social determinants of health inequities and intersectional exclusion among trans women of color in Detroit, Michigan. Sexuality Research and Social Policy. 2021:1–21.
Reback CJ, Kisler KA, Fletcher JB. A novel adaptation of peer health navigation and contingency management for advancement along the HIV care continuum among transgender women of color. AIDS Behav. 2021;25(1):40–51.
Seekaew P, Phanuphak N, Teeratakulpisarn N, Amatavete S, Lujintanon S, Teeratakulpisarn S, et al. Same-day antiretroviral therapy initiation hub model at the Thai Red Cross Anonymous Clinic in Bangkok, Thailand: an observational cohort study. J Int AIDS Soc. 2021;24(12):e25869.
Hiransuthikul A, Janamnuaysook R, Himma L, Taya C, Amatsombat T, Chumnanwet P, et al. Acceptability and satisfaction towards self-collection for chlamydia and gonorrhoea testing among transgender women in Tangerine Clinic, Thailand: shifting towards the new normal. J Int AIDS Soc. 2021;24(9):e25801.
Berg RC, Page S, Øgård-Repål A. The effectiveness of peer-support for people living with HIV: a systematic review and meta-analysis. PLoS One. 2021;16(6):e0252623.
Everhart AR, Ferguson L, Wilson JP. Construction and validation of a spatial database of providers of transgender hormone therapy in the US. Soc Sci Med. 2022;115014.
Everhart AR, Boska H, Sinai-Glazer H, Wilson-Yang JQ, Burke NB, LeBlanc G, et al. ‘I’m not interested in research; I’m interested in services’: how to better health and social services for transgender women living with and affected by HIV. Soc Sci Med. 2022;292:114610.
Sharpe D. PrEP, Prevention, and place: examining the effect of geographic accessibility on the use of HIV pre-exposure prophylaxis 2022.
Amatavete S, Lujintanon S, Teeratakulpisarn N, Thitipatarakorn S, Seekaew P, Hanaree C, et al. Evaluation of the integration of telehealth into the same-day antiretroviral therapy initiation service in Bangkok, Thailand in response to COVID-19: a mixed-method analysis of real-world data. J Int AIDS Soc. 2021;24:e25816.
Srimanus P, Janamnuaysook R, Samitpol K, Chancham A, Kongkapan J, Amatsombat T, et al. Changes in sexual behaviors and testing for HIV and sexually transmitted infections among transgender women at Tangerine Clinic during COVID-19 lockdown. The 24th International AIDS Conference: AIDS 2022; Montreal, Canda2022.
Connolly MD, Dankerlui DN, Eljallad T, Dodard-Friedman I, Tang A, Joseph CL. Outcomes of a PrEP demonstration project with LGBTQ youth in a community-based clinic setting with integrated gender-affirming care. Transgender Health. 2020;5(2):75–9.
Beckwith N, Reisner SL, Zaslow S, Mayer KH, Keuroghlian AS. Factors associated with gender-affirming surgery and age of hormone therapy initiation among transgender adults. Transgender health. 2017;2(1):156–64.
Ashley F. Gatekeeping hormone replacement therapy for transgender patients is dehumanising. J Med Ethics. 2019;45(7):480–2.
Acknowledgements
We would like to thank Wesley King, PhDc, MPH, for their time and assistance in generating the graphic visualization for this manuscript.
Funding
Dr. Restar is supported by the Research Education Institute for Diverse Scholars (REIDS) Program at Yale University School of Public Health, funded by the National Institute of Mental Health (R25MH087217). Additional support was provided by R01MH115765 (Drs. Kristi Gamarel and Don Operario) from the National Institute of Mental Health (NIMH) and R21TW012010 (Dr. Don Operario) from the Fogarty International Center (FIC). This article does not represent the official views of the sponsors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Rena Janamnuaysook has received research funding from Gilead Sciences, and speaker fees from ViiV Healthcare. Dr. Stephaun Wallace reports research funding from NIH/NIAID, Johnson and Johnson/Janssen, and Gilead. Dr. Leigh-Ann van der Merwe reports involvement as global community advisory group for Gilead’s Lenacapavir trial for transgender women. Arjee Restar, Brian J. Minalga, Ma Irene Quilantang, Tyler Adamson, Emerson Dusic, Greg Millet, Danvic Rosadiño, Tanya Laguing, Elle Lett, Avery Everhart, Gregory Phillips II, Pich Seekaew, Kellan Baker, Florence Ashley, Jeffrey Wickersham, Don Operario, and Kristi E. Gamarel, PhD, declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Restar, A., Minalga, B.J., Quilantang, M.I. et al. Mapping Community-Engaged Implementation Strategies with Transgender Scientists, Stakeholders, and Trans-Led Community Organizations. Curr HIV/AIDS Rep 20, 160–169 (2023). https://doi.org/10.1007/s11904-023-00656-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-023-00656-y