Abstract
Purpose of Review
Ileal pouch-anal anastomosis (IPAA) is the standard restorative procedure after proctocolectomy in patients with inflammatory bowel disease who require colectomy. The ileal pouch is susceptible to a variety of adverse outcomes including mechanical insult, ischemia, and infectious agents. There is also a risk for developing low-grade dysplasia (LGD), high-grade dysplasia (HGD), or even adenocarcinoma in the pouch. The purpose of this review is to highlight risk factors, clinical presentation, surveillance, and treatment of pouch neoplasia.
Recent Findings
Patients with pre-colectomy colitis-associated neoplasia are at high risk for developing pouch neoplasia. Other purported risk factors include the presence of family history of colorectal cancer, the presence of concurrent primary sclerosing cholangitis, chronic pouchitis, cuffitis, or Crohn’s disease of the pouch. Pouch adenocarcinoma tends to have a poor prognosis.
Summary
It is recommended to have a combined clinical, endoscopic, and histologic approach in diagnosis and management. Surveillance and management algorithms of pouch neoplasia are proposed, based on the risk stratification.






Similar content being viewed by others
Abbreviations
- ATZ:
-
Anal transitional zone
- CAN:
-
Colitis-associated neoplasia
- CD:
-
Crohn’s disease
- CRC:
-
Colorectal cancer
- EMR:
-
Endoscopic mucosal resection
- ESD:
-
Endoscopic submucosal dissection
- FAP:
-
Familial adenomatous polyposis
- HGD:
-
High-grade dysplasia
- IBD:
-
Inflammatory bowel disease
- IND:
-
Indefinite for dysplasia
- IPAA:
-
Ileal pouch-anal anastomosis
- LGD:
-
Low-grade dysplasia
- PSC:
-
Primary sclerosing cholangitis
- UC:
-
Ulcerative colitis
References
Papers of particular interest, published recently, have been highlighted as:•• Of major importance
Delaney CP, Fazio VW, Remzi FH, Hammel J, Church JM, Hull TL, et al. Prospective, age-related analysis of surgical results, functional outcome, and quality of life after ileal pouch-anal anastomosis. Ann Surg. 2003;238:221–8.
Fazio VW, Kiran RP, Remzi FH, Coffey JC, Heneghan HM, Kirat HT, et al. Ileal pouch anal anastomosis: analysis of outcome and quality of life in 3707 patients. Ann Surg. 2013;257:679–85.
Delaney CP, Remzi FH, Gramlich T, Dadvand B, Fazio VW. Equivalent function, quality of life and pouch survival rates after ileal pouch-anal anastomosis for indeterminate and ulcerative colitis. Ann Surg. 2002;236:43–8.
•• Derikx LA, Kievit W, Drenth JP, et al. Prior colorectal neoplasia is associated with increased risk of ileoanal pouch neoplasia in patients with inflammatory bowel disease. Gastroenterologia. 2014;146:119–28. This registry-based study provides helpful information on association between prior dysplasia or colon cancer and risk of developing pouch neoplasia.
•• Kariv R, Remzi FH, Lian L, Bennett AE, Kiran RP, Kariv Y, et al. Preoperative colorectal neoplasia increases risk for pouch neoplasia in patients with restorative proctocolectomy. Gastroenterologia. 2010;139:806–12. This is the first controlled study in pouch neoplasia based on a large institutional database.
Althumairi AA, Lazarev MG, Gearhart SL. Inflammatory bowel disease associated neoplasia: a surgeon’s perspective. World J Gastroenterol. 2016;22:961–73.
Remzi FH, Fazio VW, Delaney CP, Preen M, Ormsby A, Bast J, et al. Dysplasia of the anal transitional zone after ileal pouch-anal anastomosis: results of prospective evaluation after a minimum of ten years. Dis Colon Rectum. 2003;46:6–13.
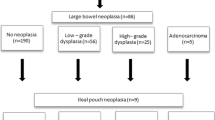
Wu XR, Remzi FH, Liu XL, Lian L, Stocchi L, Ashburn J, et al. Disease course and management strategy of pouch neoplasia in patients with underlying inflammatory bowel diseases. Inflamm Bowel Dis. 2014;20:2073–82.
Liu ZX, Kiran RP, Bennett AE, Ni RZ, Shen B. Diagnosis and management of dysplasia and cancer of the ileal pouch in patients with underlying inflammatory bowel disease. Cancer. 2011;117:3081–92.
Schaus BJ, Fazio VW, Remzi FH, Bennett AE, Lashner BA, Shen B. Clinical features of ileal pouch polyps in patients with underlying ulcerative colitis. Dis Colon Rectum. 2007;50:832–8.
Gonzalo DH, Collinsworth AL, Liu X. Common inflammatory disorders and neoplasia of the ileal pouch: a review of histopathology. Gastroenterology Res. 2016;9:29–38.
Ziv Y, Fazio VW, Sirimarco MT, Lavery IC, Goldblum JR, Petras RE. Incidence, risk factors, and treatment of dysplasia in the anal transitional zone after ileal pouch-anal anastomosis. Dis Colon Rectum. 1994;37:1281–5.
Liu ZX, Liu XL, Patil DT, Lian L, Kiran RP, Remzi FH, et al. Clinical significance of indefinite for dysplasia on pouch biopsy in patients with underlying inflammatory bowel disease. J Gastrointest Surg. 2012;16:562–71.
Van Schaik FD, Ten Kate FJ, Offerhaus GJ, et al. Misclassification of dysplasia in patients with inflammatory bowel disease: consequences for progression rates to advanced neoplasia. Inflamm Bowel Dis. 2011;17:1108–16.
Eaden JA, Mayberry JF. British Society for Gastroenterology, Association of Coloproctology for Great Britain and Ireland. Guidelines for screening and surveillance of asymptomatic colorectal cancer in patients with inflammatory bowel disease. Gut. 2002;5:10.
•• Gu J, Remzi FH, Lian L, et al. Practice pattern of ileal pouch surveillance in academic medical centers in the United States. Gastroenterol Rep. 2016;4:119–24. Authors provided information on performing pouchoscopy and biopsy for surveillance of ileal pouch neoplasia from fifty-two eligible participants from 32 tertiary institutions.
Gadacz TR, McFadden DW, Gabrielson EW, Ullah A, Berman JJ. Adenocarcinoma of the ileostomy: the latent risk of cancer after colectomy for ulcerative colitis and familial polyposis. Surgery. 1990;107:698–703.
Smart PJ, Sastry S, Wells S. Primary mucinous adenocarcinoma developing in an ileostomy stoma. Gut. 1988;29:1607–12.
Elkowitz D, Daum F, Markowitz J, Proccaccino J, Boas E, Cuomo J, et al. Risk factors for carcinoma of the pelvic ileal pouch/anal canal in ulcerative colitis. Ann Clin Lab Sci. 2004;34:143–9.
Coull DB, Lee FD, Henderson AP, Anderson JH, McKee RF, Finlay IG. Risk of dysplasia in the columnar cuff after stapled restorative proctocolectomy. Br J Surg. 2003;90:72–5.
Heuschen UA, Heuschen G, Autschbach F, Allemeyer EH, Herfarth C. Adenocarcinoma in the ileal pouch: late risk of cancer after restorative proctocolectomy. Int J Color Dis. 2001;16:126–30.
Zmora O, Spector D, Dotan I, Klausner JM, Rabau M, Tulchinsky H. Is stapled ileal pouch anal anastomosis a safe option in ulcerative colitis patients with dysplasia or cancer? Int J Color Dis. 2009;24:1181–6.
•• Ishii H, Hata K, Kishikawa J, et al. Incidence of neoplasias and effectiveness of postoperative surveillance endoscopy for patients with ulcerative colitis: comparison of ileorectal anastomosis and ileal pouch-anal anastomosis. World J Surg Oncol. 2016;14:75. The study compared the incidence of pouch neoplasia after stapled IPAA versus hand- sewn IPAA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Large Intestine
Rights and permissions
About this article
Cite this article
Khan, F., Shen, B. Inflammation and Neoplasia of the Pouch in Inflammatory Bowel Disease. Curr Gastroenterol Rep 21, 10 (2019). https://doi.org/10.1007/s11894-019-0679-4
Published:
DOI: https://doi.org/10.1007/s11894-019-0679-4