Abstract
Purpose of Review
The purpose of this study was to conduct a scoping review to map intervention, sample, and physiologic measurement characteristics of lifestyle interventions for gestational diabetes mellitus (GDM) prevention.
Recent Findings
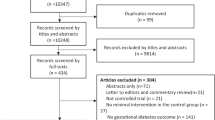
A total of 19 studies met selection criteria from 405 articles screened (PubMed, Web of Science). No studies were US-based (47% multi-site), and all were delivered in clinical settings. The most targeted nutrition components were low carbohydrate intake (sugar rich foods/added sugars, low glycemic index), low fat intake (mainly low-fat meat, dairy, and saturated fat), and increased fruits and vegetables. Many studies promoted 150 min/week moderate-intensity physical activity. Only two studies provided supervised physical activity sessions. Dietitians and nurses were the most common implementers. Samples were characterized as adults with obesity (mean age 31 yr, BMI 31 kg/m2). Asian populations were predominantly studied. Four studies used theoretical frameworks (75% of which used Social Cognitive Theory). GDM diagnostic criteria set forth by the American Diabetes Association were the most widely used. Insulin sensitivity was commonly assessed via fasting indices.
Summary
There was a lack of multi-disciplinary, multi-level, and theory-based lifestyle interventions for reducing GDM risk. Addressing these gaps and prioritizing high-risk populations in the US with measurement of traditional and novel biomarkers will advance the field.

Similar content being viewed by others
Data Availability
Spreadsheets with data used in this study are publicly available at https://osf.io/gjw2n/.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Shah NS, et al. Trends in gestational diabetes at first live birth by race and ethnicity in the US, 2011–2019. JAMA. 2021;326(7):660–9. This study demonstrates the increasing trends in gestational diabetes mellitus in the United States and by racial/ethnic sub-groups.
Noctor E, Dunne FP. Type 2 diabetes after gestational diabetes: the influence of changing diagnostic criteria. World J Diabetes. 2015;6(2):234–44.
Li S, et al. Offspring risk of obesity in childhood, adolescence and adulthood in relation to gestational diabetes mellitus: a sex-specific association. Int J Epidemiol. 2017;46(5):1533–41.
Tam WH, et al. In utero exposure to maternal hyperglycemia increases childhood cardiometabolic risk in offspring. Diabetes Care. 2017;40(5):679–86.
Li W, et al. Maternal prepregnancy BMI and glucose level at 24–28 gestational weeks on offspring’s overweight status within 3 years of age. Biomed Res Int. 2017;2017:7607210.
American College of O, B-O. Gynecologists' Committee on Practice. Obesity in pregnancy: ACOG Practice Bulletin, Number 230. Obstet Gynecol. 2021;137(6):e128-e144.
•• Cantor AG, et al. Counseling and behavioral interventions for healthy weight and weight gain in pregnancy: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2021;325(20):2094–109. This study by the US Preventive Services Task Force reviewed 68 intervention studies and found a significant reduction in gestational diabetes mellitus from lifestyle interventions.
Guo XY, et al. Improving the effectiveness of lifestyle interventions for gestational diabetes prevention: a meta-analysis and meta-regression. BJOG. 2019;126(3):311–20.
Bennett CJ, et al. Interventions designed to reduce excessive gestational weight gain can reduce the incidence of gestational diabetes mellitus: a systematic review and meta-analysis of randomised controlled trials. Diabetes Res Clin Pract. 2018;141:69–79.
Rogozinska E, et al. Nutritional manipulation for the primary prevention of gestational diabetes mellitus: a meta-analysis of randomised studies. PLoS ONE. 2015;10(2):e0115526.
Madhuvrata P, et al. Prevention of gestational diabetes in pregnant women with risk factors for gestational diabetes: a systematic review and meta-analysis of randomised trials. Obstet Med. 2015;8(2):68–85.
•• Griffith RJ, et al. Interventions to prevent women from developing gestational diabetes mellitus: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2020;6(6):CD012394. This study of 11 Cochrane Reviews that included 71 total trials found no clear benefit or harm of gestational diabetes prevention interventions, including exercise and diet.
Group D.P.P.D.R. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care 2002;25(12):2165–71
Knowler WC, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403.
Aziz Z, et al. A systematic review of real-world diabetes prevention programs: learnings from the last 15 years. Implement Sci. 2015;10:172.
Ackermann RT, O’Brien MJ. Evidence and challenges for translation and population impact of the diabetes prevention program. Curr Diab Rep. 2020;20(3):9.
Peters MDJ, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Implement. 2021;19(1):3–10.
Peters MDJ, et al. Scoping reviews: reinforcing and advancing the methodology and application. Syst Rev. 2021;10(1):263.
Tricco AC, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Peña A, Miller A. Mapping the characteristics of gestational diabetes prevention lifestyle interventions: a scoping review. 2022. https://doi.org/10.17605/OSF.IO/RW2UH.
Koivusalo SB, et al. Gestational diabetes mellitus can be prevented by lifestyle intervention: the Finnish Gestational Diabetes Prevention Study (RADIEL): a randomized controlled trial. Diabetes Care. 2016;39(1):24–30.
Luoto R, et al. Primary prevention of gestational diabetes mellitus and large-for-gestational-age newborns by lifestyle counseling: a cluster-randomized controlled trial. PLoS Med. 2011;8(5):e1001036.
Sagedal LR, et al. The effect of a prenatal lifestyle intervention on glucose metabolism: results of the Norwegian Fit for Delivery randomized controlled trial. BMC Pregnancy Childbirth. 2017;17(1):167.
Korpi-Hyovalti EA, et al. Feasibility of a lifestyle intervention in early pregnancy to prevent deterioration of glucose tolerance. BMC Public Health. 2011;11:179.
Rono K, et al. Prevention of gestational diabetes with a prepregnancy lifestyle intervention - findings from a randomized controlled trial. Int J Womens Health. 2018;10:493–501.
Lin X, et al. Lifestyle intervention to prevent gestational diabetes mellitus and adverse maternal outcomes among pregnant women at high risk for gestational diabetes mellitus. J Int Med Res. 2020;48(12):300060520979130.
Ding B, et al. WeChat-assisted dietary and exercise intervention for prevention of gestational diabetes mellitus in overweight/obese pregnant women: a two-arm randomized clinical trial. Arch Gynecol Obstet. 2021;304(3):609–18.
Deng Y, et al. Effects of diet and exercise interventions to prevent gestational diabetes mellitus in pregnant women with high-risk factors in China: a randomized controlled study. Clin Nurs Res. 2022;31(5):836–47.
Chan RS, et al. Randomized trial examining effectiveness of lifestyle intervention in reducing gestational diabetes in high risk Chinese pregnant women in Hong Kong. Sci Rep. 2018;8(1):13849.
Poston L, et al. Effect of a behavioural intervention in obese pregnant women (the UPBEAT study): a multicentre, randomised controlled trial. Lancet Diabetes Endocrinol. 2015;3(10):767–77.
Simmons D, et al. Effect of physical activity and/or healthy eating on GDM risk: the DALI Lifestyle Study. J Clin Endocrinol Metab. 2017;102(3):903–13.
Petrella E, et al. Gestational weight gain in overweight and obese women enrolled in a healthy lifestyle and eating habits program. J Matern Fetal Neonatal Med. 2014;27(13):1348–52.
Bruno R, Petrella E, Bertarini V, Pedrielli G, Neri I, Facchinetti F. Adherence to a lifestyle programme in overweight/obese pregnant women and effect on gestational diabetes mellitus: a randomized controlled trial. Matern Child Nutr. 2017;13(3). https://doi.org/10.1111/mcn.12333.
Motahari-Tabari NS, et al. The effectiveness of information-motivation-behavioral skills model on self-care practices in early pregnancy to prevent gestational diabetes mellitus in iranian overweight and obese women: a randomized controlled trial. Community Health Equity Res Policy. 2023;43(3):257–64.
Eslami E, et al. The effect of a lifestyle-based training package on weight gain and frequency of gestational diabetes in obese and overweight pregnant females. Iran Red Crescent Med J. 2018;20(S1):e62576.
Sadiya A, et al. Lifestyle intervention in early pregnancy can prevent gestational diabetes in high-risk pregnant women in the UAE: a randomized controlled trial. BMC Pregnancy Childbirth. 2022;22(1):668.
Kennelly MA, et al. Pregnancy exercise and nutrition with smartphone application support: a randomized controlled trial. Obstet Gynecol. 2018;131(5):818–26.
Harrison CL, et al. Optimizing healthy gestational weight gain in women at high risk of gestational diabetes: a randomized controlled trial. Obesity (Silver Spring). 2013;21(5):904–9.
Kunath J, et al. Effects of a lifestyle intervention during pregnancy to prevent excessive gestational weight gain in routine care - the cluster-randomised GeliS trial. BMC Med. 2019;17(1):5.
International Association of D, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33(3):676–82.
Organization W. H. Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy. 2013: Geneva.
Matthews DR, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH. The pathophysiology of gestational diabetes mellitus. Int J Mol Sci. 2018;19(11). https://doi.org/10.3390/ijms19113342.
Ruiz JR, et al. Supervised exercise-based intervention to prevent excessive gestational weight gain: a randomized controlled trial. Mayo Clin Proc. 2013;88(12):1388–97.
Onaade O, et al. Physical activity for blood glucose control in gestational diabetes mellitus: rationale and recommendations for translational behavioral interventions. Clin Diabetes Endocrinol. 2021;7(1):7.
ACOG Committee Opinion No. 804: Physical activity and exercise during pregnancy and the postpartum period: correction. Obstet Gynecol. 2021;138(4):683.
Marshall NE, et al. The importance of nutrition in pregnancy and lactation: lifelong consequences. Am J Obstet Gynecol. 2022;226(5):607–32.
Rhodes EC, et al. Promoting equity in breastfeeding through peer counseling: the US Breastfeeding Heritage and Pride program. Int J Equity Health. 2021;20(1):128.
Chang YS, et al. Views and experiences of women, peer supporters and healthcare professionals on breastfeeding peer support: a systematic review of qualitative studies. Midwifery. 2022;108:103299.
Disparities, N.I.o.M.H.a.H. National institute of minority health and health disparities. (2017) NIMHD research framework. 2017 [cited 2023 May 1]. https://nimhd.nih.gov/researchFramework. Accessed 8 Aug 2023.
Hill-Briggs F, Adler NE, Berkowitz SA, et al. Social determinants of health and diabetes: a scientific review. Diabetes care. 2020. https://doi.org/10.2337/dci20-0053.
Clark ML, Utz SW. Social determinants of type 2 diabetes and health in the United States. World J Diabetes. 2014;5(3):296–304.
Phonyiam R. Barriers and facilitators to diabetes self-management in pregnant women with pre-existing type 2 diabetes mellitus: a scoping review. Curr diabetes rev. 2022. https://doi.org/10.2174/1573399819666220627111430.
Phonyiam R, Berry DC. Racial and ethnic disparities in health care and health outcomes for pregnant women with diabetes. Nurs Womens Health. 2021;25(6):437–49.
Thornton PL, et al. New research directions on disparities in obesity and type 2 diabetes. Ann N Y Acad Sci. 2020;1461(1):5–24.
Roman CG, et al. The relation of the perceived environment to fear, physical activity, and health in public housing developments: evidence from Chicago. J Public Health Policy. 2009;30(Suppl 1):S286-308.
Roman CG, Chalfin A. Fear of walking outdoors. A multilevel ecologic analysis of crime and disorder. Am J Prev Med. 2008;34(4):306–12.
Geneshka M, Coventry P, Cruz J, Gilbody S. Relationship between green and blue spaces with mental and physical health: a systematic review of longitudinal observational studies. Int J Environ Res Public Health. 2021;18(17). https://doi.org/10.3390/ijerph18179010.
Bancroft C, et al. Association of proximity and density of parks and objectively measured physical activity in the United States: a systematic review. Soc Sci Med. 2015;138:22–30.
Lee JLC, Lo TLT, Ho RTH. Understanding outdoor gyms in public open spaces: a systematic review and integrative synthesis of qualitative and quantitative evidence. Int J Environ Res Public Health. 2018;15(4). https://doi.org/10.3390/ijerph15040590.
Stalsberg R, Pedersen AV. Are differences in physical activity across socioeconomic groups associated with choice of physical activity variables to report? Int J Environ Res Public Health. 2018;15(5). https://doi.org/10.3390/ijerph15050922.
Gross RS, Mendelsohn AL, Arana MM, Messito MJ. Food insecurity during pregnancy and breastfeeding by low-income hispanic mothers. Pediatrics. 2019;143(6). https://doi.org/10.1542/peds.2018-4113.
Di Renzo GC, Tosto V. Food insecurity, food deserts, reproduction and pregnancy: we should alert from now. J Matern Fetal Neonatal Med. 2022;35(25):9119–21.
National Academies of Sciences Engineering and Medicine (U.S.). Committee on Integrating Social Needs Care into the Delivery of Health Care to Improve the Nation's Health. Integrating social care into the delivery of health care : moving upstream to improve the nation's health. A consensus study report of the National Academies of Sciences, Engineering, Medicine. 2019, Washington, DC: the National Academies Press. xv, 177 pages.
Reinoso D, et al. Addressing food insecurity: lessons learned from co-locating a food pantry with a federally qualified health center. Int J Integr Care. 2022;22(3):24.
Lim S, Takele WW, Vesco KK, Redman L, group APGpw, Josefson J. A systematic review and meta-analysis of participant characteristics in the prevention of gestational diabetes: a summary of evidence for precision medicine. medRxiv. 2023. https://doi.org/10.1101/2023.04.16.23288650.
Sparks JR, et al. Lifestyle interventions in pregnancy targeting GDM prevention: looking ahead to precision medicine. Diabetologia. 2022;65(11):1814–24.
de Mendonca E, Fragoso MBT, de Oliveira JM, Xavier JA, Goulart MOF, de Oliveira ACM. Gestational diabetes mellitus: The crosslink among inflammation, nitroxidative stress, intestinal microbiota and alternative therapies. Antioxidants (Basel). 2022;11(1). https://doi.org/10.3390/antiox11010129.
Pantham P, Aye IL, Powell TL. Inflammation in maternal obesity and gestational diabetes mellitus. Placenta. 2015;36(7):709–15.
Lekva T, et al. Impact of systemic inflammation on the progression of gestational diabetes mellitus. Curr Diab Rep. 2016;16(4):26.
Jadhav A, Khaire A, Joshi S. Exploring the role of oxidative stress, fatty acids and neurotrophins in gestational diabetes mellitus. Growth Factors. 2020;38(3–4):226–34.
Zhu W, et al. Epigenetic alternations of microRNAs and DNA methylation contribute to gestational diabetes mellitus. J Cell Mol Med. 2020;24(23):13899–912.
Dluski DF, Wolinska E, Skrzypczak M. Epigenetic changes in gestational diabetes mellitus. Int J Mol Sci. 2021;22(14). https://doi.org/10.3390/ijms22147649.
Wang QY, et al. Current progress in metabolomics of gestational diabetes mellitus. World J Diabetes. 2021;12(8):1164–86.
Kemp L. Adaptation and fidelity: a recipe analogy for achieving both in population scale implementation. Prev Sci. 2016;17(4):429–38.
Acknowledgements
We are grateful to all researchers who conducted the studies that were available for review and the research participants that participated in them.
Funding
This work was funded, in part, by the Health Equity Advancing through Learning health system Research (HEAL-R) Collaborative, a partnership between IU Health’s Office of Health Equity Research and Engagement (HERE) and the Indiana University School of Medicine, generously funded by a Cook Group Incorporated Advances in Medicine (AIM) award.
Author information
Authors and Affiliations
Contributions
AP conceived of the study. AP and AMM served as primary reviewers and AGC as third reviewer. AP conducted the analysis and wrote the first draft of the manuscript with revisions from AMM, AGC, CMS, and RJH.
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
No studies reported in this article included animal subjects. All reported studies/experiments with human subjects performed by the authors were performed in accordance with all applicable ethical standards including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines.
Competing Interests
The authors declare no competing interests.
Disclaimer
The funder/sponsor did not participate in the work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Peña, A., Miller, A.M., Campbell, A.G. et al. Mapping Lifestyle Interventions for Gestational Diabetes Prevention: A Scoping Review. Curr Diab Rep 24, 74–83 (2024). https://doi.org/10.1007/s11892-024-01535-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11892-024-01535-5