Abstract
Purpose of Review
Bioengineering of functional cardiac tissue composed of primary cardiomyocytes has great potential for myocardial regeneration and in vitro tissue modeling. 3D bioprinting was developed to create cardiac tissue in hydrogels that can mimic the structural, physiological, and functional features of native myocardium. Through a detailed review of the 3D printing technologies and bioink materials used in the creation of a heart tissue, this article discusses the potential of engineered heart tissues in biomedical applications.
Recent Findings
In this review, we discussed the recent progress in 3D bioprinting strategies for cardiac tissue engineering, including bioink and 3D bioprinting methods as well as examples of engineered cardiac tissue such as in vitro cardiac models and vascular channels.
Summary
3D printing is a powerful tool for creating in vitro cardiac tissues that are structurally and functionally similar to real tissues. The use of human-induced pluripotent stem cell-derived cardiomyocytes (iPSC-CM) enables the generation of patient-specific tissues. These tissues have the potential to be used for regenerative therapies, disease modeling, and drug testing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
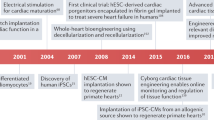
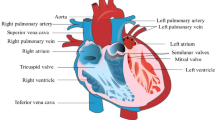
Cardiovascular disease (CVD) is still one of the leading causes of death worldwide due to its high mortality and morbidity [1]. Currently, heart transplantation is the best option at the end-stage of CVD [2]. However, since the shortage of heart donors, new sources of cardiac regenerative medicine are greatly needed to regenerate an infarcted heart [3]. Recently, engineered cardiac tissues provided an alternative approach for addressing the growing demand for heart transplantation due to its potential to repair a cardiac tissue by integrating cardiac cells with biomaterials [4–6].
Cardiac tissue engineering aims to repair, regenerate, and replace the damaged heart tissue, which develops technologies to form cardiac constructs by using a combination of cells, biomaterials, and signaling molecules [7–9]. In addition to restoring the function of an infarcted tissue, a cardiac tissue that is derived from autologous cells is less likely to trigger an immune response [10, 11]. Given these possible benefits, cardiac tissue engineering has the potential to develop cardiac tissue constructs for the treatment of CVD [12]. To manufacture tissue-engineered scaffolds, 3D bioprinting emerged as a powerful tool that can accurately deposit biomaterials and cardiac cells in accordance with a certain spatial pattern [13–15]. In addition, it can produce a highly continuous and stable biological pattern, which can achieve a high resolution simulating the key state of the heart and paving the way for myocardial tissue repair and regeneration [16–18]. To mimic the complex architectural features of native tissue and create patient-specific 3D models, a wide variety of imaging technologies such as 3D scanners, computed tomography (CT), magnetic resonance imaging (MRI) systems, and computer-aided design (CAD) software have been used [19, 20].
Additionally, various biomaterials have been utilized as bioinks for 3D bioprinting cardiac constructs, including alginate, gelatin, collagen, and decellularized extracellular matrix (ECM). These biomaterials are used in conjunction with various bioprinting methods such as extrusion, inkjet, laser-assisted, and light-based techniques [21, 22]. Depending on the type of engineered cardiac tissues (e.g., myocardium, vascularization) being created, specific combinations of biomaterials and bioprinters are selected [23–26]. In this review, we present the state-of-the-art of 3D bioprinting techniques and biomaterials (bioinks) for 3D bioprinting of cardiac constructs. We also emphasize the recent advancements in using 3D bioprinting and bioinks to develop relevant tissue models for cardiovascular tissue engineering.
Printing Techniques for 3D Tissue Fabrication
3D printing technology has the potential to automate the creation of artificial cardiac tissues by recreating key characteristics such as position, size, shape, number and type of cells, and physiological complexity [22, 27, 28]. Customized structures can be realized through an additive manufacturing process using computer-aided design (CAD) models [29]. By controlling the spatial positions of cells and providing topological, chemical, and complex cues, 3D printing can promote the morphogenesis of cardiac tissue and the development of neovascularization and maturation in engineered cardiovascular tissues [30]. To ensure the structural and functional operation of cardiac tissues, several aspects must be considered, including bioprinting methods and the use of printable biomaterials [30].
Bioinks
Bioinks are used to construct a temporary ECM in a tissue-engineered scaffold in order to provide a tissue-specific microenvironment to guide cellular behaviors and promote cell recruitment, migration, adhesion, proliferation, differentiation, and maturation. [31, 32] Additionally, this transient ECM ought to give cells the necessary mechanical support. When developing bioinks for 3D bioprinting, certain properties should be taken into consideration. A variety of materials have so far been explored for the development of bioinks. The two most popular natural biomaterials that have been thoroughly explored for cardiac tissue regeneration using 3D printing are gelatin and alginate [33]. Gelatin is a biodegradable polymer with unique properties such as amino acid composition, gel strength, isomeric point, and charge [34]. One of the best-known derivatives of gelatin is its methacrylated gelatin (GelMA). GelMA exhibits promising qualities as a bioink due to its strong biocompatibility, ability for photocrosslinking, and programmable physicochemical features [35]. An anionic polysaccharide, alginate is a natural biopolymer that is non-toxic, non-immunogenic, biocompatible, and inexpensive [36]. Alginate can be ionically crosslinked with Ca2 + , making it a suitable material for bioprinting [37]. Alginate’s ability to support cell encapsulation and cell growth throughout the bioprinting process is an additional benefit when employing it as a cell-laden material for 3D bioprinting [38]. Additionally, other natural polymers like collagen, silk, chitosan, and hyaluronic acid are also extensively applied [21, 39–41].
Synthetic polymers, on the other hand, offer a mechanically robust structure with better control of chemical and mechanical properties, but the absence of active binding sites, which can activate the biological signaling pathway, hinders cell adherence, and may even cause cell death [42]. Therefore, a limited number of synthetic polymers with adjustable mechanical strength and degradation capability, such as poly(ethylene glycol) diacrylate (PEGDA), are utilized to directly encapsulate cells for printing operations [43]. Comprehensive descriptions are available in a number of pertinent publications [43, 44].
Bioprinting Method
For creating 3D cell-laden constructions for tissue engineering purposes, 3D bioprinting is the most up-to-date technique currently available to scientists. The in situ cell encapsulation empowered by 3D bioprinting facilitates the reorganization of the fabricated model into functional tissue constructs [45]. High accuracy and flexibility are two other key advantages of 3D bioprinting. The two primary categories of 3D bioprinting techniques are light-based (such as digital light processing (DLP), two-photon polymerization (TPP), and laser-assisted bioprinting) and nozzle-based (such as inkjet and extrusion bioprinting) [46, 47].
DLP Bioprinting
In DLP bioprinting, photon energy (e.g., LED light) is used to induce photopolymerization of a bioink to form 3D structures in a projection and layer-by-layer fashion. DLP bioprinting controls tissue architectures in all three dimensions with high resolution and precision [48]. Photocrosslinking of the bioink with cells minimizes the shear force and heat impact on the cells and provides better spatial and temporal control during the polymerization process [49]. In particular, microscale continuous optical printing (μCOP) has emerged as an advancement of DLP printing. This method involves converting a 2D image into a volume of prepolymer solution while combining continuous stage movement with adjustments to digital masks. This results in higher spatial resolution and can create millimeter- or centimeter-scale structures in seconds to minutes [50]. In aμCOP printer, a digital micromirror device (DMD) chip composed of an array of millions of micromirrors is employed to project user-defined patterns by turning on or off each micromirror [51]. The projection optics direct the light that is reflected by the “on” mirrors onto the prepolymer solution, where it immediately starts to polymerize layer by layer. The printer is designed to allow continuous movement in the Z-stage, therefore creating a 3D structure that replicates the desired pattern in a continuous fashion with much improved structural integrity. Cells can be directly patterned into a 3D hydrogel using appropriate bioinks, allowing control over cell alignment and concentration in the printed tissue construct [52]. Higher cell viabilities can be achieved using DLP bioprinting approaches without the high sheer pressures that occur in nozzle-based bioprinting, even for sensitive cell types such as stem cells [46].
Extrusion-Based Bioprinting
Extrusion-based bioprinting is a well-developed 3D bioprinting technique used in tissue engineering [15]. In this method, the bioink is typically placed in a syringe-like tool that uses a controlled force—pneumatic pressure or mechanical force generated by a piston or screw—to propel the bioink through a nozzle [53]. The size and structure of the nozzles placed at the end of the syringe are selected according to the specification of the structural design [54]. This bioprinting technique can deposit highly viscous bioinks with high cell concentrations at a large deposition rate [55]. Moreover, multi-nozzle extrusion bioprinters facilitate simultaneous deposition of heterogeneous constructs [56], enabling direct bioprinting of different cardiovascular cell types, i.e., fibroblasts, endothelium, smooth muscle cell (SMC), and stroma into a single tissue abridge by co-printing [57]. Extrusion-based bioprinting represents a convenient, intensively explored rapid prototyping platform with reasonable resolutions and costs. In extrusion bioprinting, however, the main factor affecting cell viability is the shear stress acting on the bioink, which depends on the viscosity of the bioink, nozzle dimension, and printing pressure [58]. Although printing resolution can be improved by smaller nozzles, a decrease in nozzle diameter results in higher shear stress (i.e., lower cell viability) and nozzle clogging. Therefore, the resolution of this method is usually limited. The minimum feature size is generally 150 μm, which is much worse than other bioprinting techniques [59, 60].
Inkjet Bioprinting
Inkjet bioprinting has been largely adapted from commercial inkjet printers, making it available at low costs [61]. Because it is based on the mechanical pulse of the printing head to generate and precisely position small droplets (1–100 picoliters), inkjet printing has a high-resolution characteristic [62]. The bioink is poured into a chamber with an inkjet head, and thermal or acoustic pressure is then applied to cause small, controllable droplets of bioink to be released onto a collection plate. Thermal and piezoelectric methods are commonly used to deposit bioink from the head, and the motion stage allows for the generation of specific 2D patterns or 3D structures [32]. A thermal inkjet printer, in particular, produces bioink drops via a heating pulse from a microheater. A piezoelectric inkjet printer generates a direct mechanical pulse, which causes a force to expel bioink droplets from the printing head [63]. This technique’s main advantages are its high resolution and ability to form thin layers and patterned constructs. Inkjet printers can produce a high-resolution structure (around 20–100 μm) at a high printing speed of 1–1000 drops/s. [64] However, one limitation of inkjet bioprinting is that high-viscosity bioinks are difficult to be bioprinted properly due to clogging at the outlet nozzle. Consequently, using low-viscosity bioinks with lower cell content results in fewer cells delivered per unit time. Furthermore, because inkjet bioprinters can only use low-viscosity bioinks (3–12 mPa/s), a crosslinking step is almost always required after bioprinting to achieve a stable structure [39, 65].
Laser-Assisted Bioprinting
The essential parts of a laser-based bioprinter include a continuous or pulsed laser source, a laser-transparent printing ribbon covered with a layer of cell-filled bioink, and a substrate slide mounted on a moveable plate [64]. Laser-based methods are classified according to the type of these components: (1) laser-induced cell transfer technologies and (2) laser stereolithography. Light-induced forward transfer (LIFT) and direct write processes are examples of cell transfer technologies. LIFT consists of a laser, a donor substrate layered with liquid enclosing biological elements (bioink), and a receiver substrate that receives the printed liquid [66, 67]. By pulsing onto a layer of bioink that contains cells (referred to as ribbon) that is positioned beneath a layer that absorbs laser energy, the LIFT technique creates a droplet that contains cells [68]. The main advantages of laser-based bioprinters are high resolution (the ability to bioprint a single cell per droplet), no clogging, the ability to bioprint low-viscosity bioinks (1–300 mPa s), and the ability to fabricate cellularized constructs with a high cell density (up to 108 cells per mL) [69–71]. The main drawbacks of laser-based bioprinting, on the other hand, include the possibility of cell damage caused by laser radiation, the complexity of controlling laser pulses, the challenge of manufacturing the cell-embedded ribbons before printing, difficulty and low throughput for 3D tissue formation, and the high cost of the laser system [72, 73].
In laser stereolithography, tissue formation via laser-induced photopolymerization is possible in the presence of photosensitive bioinks and cells [67]. A 3D scaffold is formed by laser scanning of the bioink in a dot-by-dot or line-by-line fashion. To improve printing resolution, two‐photon polymerization (TPP) is employed by using a ultrafast laser [74]. By exposing photosensitive materials to focused low-energy femtosecond (fs) laser pulses (near-infrared (NIR) light) with the ability to direct laser focal point in the desired spot, biocompatible, high-resolution, and selective consolidation of photosensitive materials is made possible [75]. The method has been utilized to fabricate scaffolds in biocompatible hydrogels with focus spots as small as sub-micron utilizing a femtosecond laser (100 fs pulse, 800 nm wavelength, at 80 MHz, 0.1–10 nJ per pulse) [76, 77]. Sub-micrometer scale features can be obtained since the diffraction limit of the light source is not a constraint on TPP’s resolution. However, the printing speed is typically slower than DLP due to the point-by-point or line-by-line polymerization process [78].
3D Printing Scaffolds for Vascularized Organoids
Cells are highly dependent on the blood supply for oxygen and nutrients to maintain their proper function, proliferation, and viability [79]. Several studies have found that oxygen and nutrient diffusivity is only adequate over short distances (200 m) [80, 81]. As a result, the vascular network is a critical component in tissue engineering. Liu et al. investigated early vascular cells (EVCs) derived from human embryonic stem cells (hESCs) as seeding cells for vascular engineering in cardiac tissues (Fig. 1A) [82••]. The authors demonstrated that 3D bioprinting of cardiomyocytes (CMs) and EVC spheroids mediated vascular differentiation and self-assembling, leading to the fabrication of functional cardiac microtissues with well-organized microvasculature. Based on these vascularized cardiac organoids, it was discovered that the presence of EVCs carrying CD34+ progenitor cells during the vascular induction stage is necessary for the effective differentiation of microvascular cells. The ability of EVCs to form 3D networks in engineered matrices demonstrated that hydrogel plays an essential role in the formation of self-organized vascular networks. The authors applied an anchorage-dependent cardiac tissue 3D bioprinting strategy in order to construct EVC spheroid-laden cardiac patches. This strategy induced in situ differentiation and microvasculature self-assembly in the contractile cardiac tissue with the cellular organization. Also, EVC spheroids showed better 3D vascular network formation than EVC single cells in 3D bioprinted myocardial tissues. Finally, they developed centimeter-scale cardiac tissues with well-organized and dense microvasculature using 3D printing with self-assembly EVC spheroid, which has great potential for cell-based therapy of in vivo myocardial infarction (MI) test.
A Representative and schematic images of BIO-X 3D bioprinter for bioprinting cardiac tissue. Typical three components of the bioprinter were marked as a, b, and c. Thereinto, “a” represents thermoplastic printhead, “b” represents conventional pneumatic printhead, and “c” represents temperature-controlled printhead (reprinted from: Liu Y et al. [82]; Creative Commons user license https://creativecommons.org/licenses/by/4.0/) B Fabrication of the cardiac micro-tissue and Schematic of DLP-based bioprinter consisting of a (1) UV light source, (2) DMD, (3) focusing optics, (4) prepolymer solution, (5) 3D sample stage, and (6) fully printed scaffold (reprinted from: Miller KL et al. [90], with permission from Elsevier). C Schematic illustration of fabrication of biomimetic cardiac tissue using scaffold-free de novo 3Dprinting technique, which is applied for in situ detection of drug-induced sodium ion channel responses (reprinted from: Samson AAS [91], with permission from Elsevier). D Schematic illustration of aOBB orientation within the compacted bioink, which depicts their initial random orientation in the syringe reservoir followed by their shear-induced alignment during ink extrusion from nozzle and multiscale alignment generated via bioprinting cardiac inks composed of aOBBs (reprinted from: Ahrens JH [92], with permission from John Wiley and Sons)
3D Printing Vascular Channels
Blood vessels are the conduits through which blood is distributed to body tissues. They are responsible for transporting oxygen, nutrients, and blood cells to the tissue as well as for removing carbon dioxide and other waste products [83]. Recently, synthetic grafts made from poly(ethylene terephthalate) and expanded polytetrafluoroethylene have been widely used [84, 85]. However, these grafts for the heart have significant downsides, such as low patency rates and graft failure due to hyperplasia and atherosclerosis [86, 87]. To overcome the limitations of conventional artificial vascular grafts, Wang et al. developed a tough double-network hydrogel bioink to fabricated mono- and dual-layered hollow conduits to mimic the real vein and artery tissues, respectively [88••]. The bioink comprised of sodium alginate and gelatin (or GelMA) forms a double-network hydrogel with energy-dissipative ionically crosslinked alginate and enzyme–crosslinked gelatin. Microfluidic coaxial extrusion bioprinting with two or three channels was utilized to fabricate monolayered or dual-layered vascular conduits, respectively, with this bioink. Coaxial extrusion bioprinting offers a number of significant benefits for creating vascular conduits. First, conduits made using the approach would have structurally appropriate tubes with tunable wall thicknesses. Additionally, this method allowed for the high-throughput production of lengthy, continuous tubes. Finally, coaxial bioprinting allowed for successful conduit manufacture with minimal bioink waste, making it ideal for the economic and mass production of conduits. With the recapitulation of important characteristics of natural blood vessel, the in vitro test demonstrated that these vascular conduits can be used as a reliable preclinical model to investigate the vascular responses to SARS-CoV-2 infections. Ex vivo and in vivo tests demonstrated that the bioprinted conduit could be glued to an ex vivo explanted mouse aorta and vena cava without causing visible leakage. This set of findings demonstrated that bioprinted conduits have a high potential for future translational applications of in vivo vascular reconstruction.
In another study, Skylar-Scott et al. manufactured the organ-specific tissues with a high cellular density and embedded vascular channels [89]. They reported a biomanufacturing method by using sacrificial writing into functional tissue (SWIFT) with living organ building blocks (OBB) matrix. First, a cold OBB-ECM slurry was centrifuged to produce a living tissue matrix containing approximately 200 million cells/ml. The tissue construct was warmed to 37 °C after SWIFT. The sacrificial gelatin ink melted and was removed from the tissue build, leaving behind a network of tubular channels imbedded within the tissue construct. To sustain cell viability, the resultant tissue was immediately linked to an external pump and perfused in oxygenated medium. As a result, SWIFT was able to integrate vascular channels into living matrices made up of a diverse set of OBBs. Next, they introduced HUVECs to manufacture a perfusable endothelial-lined channels by SWIFT. Endothelial cells were seeded specifically by first passing a suspension of HUVECs through an embedded, bifurcating vascular network within a SWIFT construct. It was allowed for the cells to attach to the luminal surface. Finally, using cardiac structural data from the National Institutes of Health 3D Print Exchange, they printed a 3D CAD model of a typical human heart, comprising a portion of the left anterior descending (LAD) artery and a diagonal branch within a cardiac OBB matrix. In conclusion, they presented SWIFT, a new biomanufacturing technology that employs OBB tissue matrices with a cell density, microarchitecture, and function similar to that of real tissues. SWIFT can be used with a variety of OBBs, such as embryoid bodies (EBs), differentiated organoids, and multi-cellular spheroids.
3D Printing of Cardiac Model
Accurate and high-throughput drug testing is critical since cardiac disease is a reigning problem in the world. With the 2D culture of cells on flat surfaces, it is difficult to understand their original functions inherited from their 3D existence. To address the limitation of current models, 3D-printed cardiac tissue is a promising approach that reproduces the cell–cell, cell–matrix interaction, and tissue architecture to imitate the structural and functional complexity of heart tissues [26]. Miller et al. reported a novel method for cardiomyocyte encapsulation in 3D GelMA scaffolds with micropatterns using an in-house designed microcontinuous optical printing system (Fig. 1B) [90]. They designed an asymmetric, cantilever-based tissue scaffold and customizable force-measuring system that directly measures the deformation produced by the beating microtissue. The microtissue displayed a high degree of sarcomere organization and produced a tissue that contracted synchronously. The force output was determined by the deflection of an integrated, 3D-printed force gauge. They showed that the 3D microtissues could be sustained over an extended period, generate significant forces, and be validated against drugs at different doses, demonstrating corresponding and measurably different changes in beating frequency and displacement force. This highly customizable 3D cardiac tissue fits in multi-well plates and could be used for high-throughput disease modeling and drug discovery in the future.
In another study, Samson et al. fabricated a scaffold-free 3D printing model (SFP) for the simultaneous extrusion of bioink [91]. The SFP method, which uses precise printed patterns, can be used to systematically study the formation of native cardiac tissue patterns in order to generate consistent tissue structures. The cells are trapped within the 3D-printed cell-laden pattern when printing. The hydrogel composition keeps the original printed shape since it is stiff. The 3D-printed structure provides the necessary space for printed cells to grow and proliferate. This printing method can print cell-laden 3D structures as well as structures with mechanical support that can generate tissue structures with desired patterns. They assessed the maturity of the constructs through the modulation that occurred in Na+ channels, and they used Na+ indicators to monitor the effect of drugs on intracellular Na+ levels, which evaluated the functionality of the SFP-engineered cardiac constructs. This study demonstrated that drug response in 3D-printed cardiac tissue can be accurately assessed by measuring the fluorescent signal and can be assessed both qualitatively and quantitatively from 3D-reconstructed images.
Most recently, the Lewis group has developed engineered cardiac tissue with programmable alignment via bioprinting of anisotropic organ building blocks (aOBBs) [92••]. Gelatin and fibrinogen are employed as the bioinks. The initial stage in developing their heart bioink is to use stereolithography to create scalable micropillar arrays (SLA). Tens of thousands of aOBBs with controlled aspect ratio and cellular composition are produced using these micropillar arrays. These aOBBs are elongated microtissues made up of cellularly aligned hiPSC-CMs that may be constructed modularly into a printed bioink. Individual aOBBs in this bioink align along the print path due to shear and extensional forces similar to those that orient acellular fibers when extruded via a tapered nozzle. They created cardiac tissues with a high cell density and controlled alignment at various length scales, from aOBBs in isolation to the sarcomeric machinery that controls the contractile function of the tissues. Cardiovascular macrofilaments made of aOBBs showed a preferred cellular alignment along the printing direction that was higher than the spheroid-based controls after bioprinting. The functional characterization of aligned cardiac macrofilaments showed that the conduction velocity (CV) was gradually increased and Connexin-43-positive gap junctions and N-Cadherin-positive adherens junctions, which are signs of tissue fusion, were also observed between cardiomyocytes. Finally, they emphasized the capacity to alter the amplitude and direction of contractile force in printed cardiac tissue sheets with a varying aOBB orientation.
Conclusion
Recent advancements in 3D bioprinting technology have demonstrated its potential as a powerful tool for the field of cardiac tissue engineering. 3D bioprinting provides a platform for exploring new avenues in development, regenerative medicine, and drug responsiveness by enabling the construction of complex, organ-mimicking cellular structures on scaffolds with precision and flexibility in design. In addition, the use of 3D printing to fabricate scaffolds for vasculature is becoming an increasingly viable approach in biofabrication, offering the potential for creating physiologically informed blood vessel networks in tissue engineering. Furthermore, the convergence of 3D bioprinting with stem cell engineering allows for the creation of 3D tissue models that accurately reflect individual characteristics in vivo, leading to a greater impact in treatment outcomes. However, there are still areas where further research is required to fully realize the potential of 3D bioprinting in the field of cardiac tissue engineering. One such area is the coordination between bioink material and bioprinting parameters, which greatly influence the mechanical properties of scaffolds, biocompatibility, printing resolution, and flexibility. This underscores the importance of selecting appropriate bioink materials and 3D printing parameters for optimal tissue generation. The use of iPSC-derived cardiomyocytes in 3D-printed tissues will enable patient-specific treatment and drug testing. However, maturing the iPSC-CMs needs further research. Furthermore, incorporating multiple cell types according to in vivo architecture in 3D bioprinting still remains a challenge. In conclusion, continued investigations are necessary to better understand the intricacies of cardiac biology and fully realize the potential of 3D bioprinting for the field of cardiovascular disease modeling and treatment.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25.
Benatti RD, Oliveira GH, Bacal F. Heart transplantation for Chagas cardiomyopathy. J Heart Lung Transplant. 2017;36(6):597–603.
Liu N, Ye X, Yao B, Zhao M, Wu P, Liu G, et al. Advances in 3D bioprinting technology for cardiac tissue engineering and regeneration. Bioactive Materials. 2021;6(5):1388–401.
Qasim M, Haq F, Kang M-H, Kim J-H. 3D printing approaches for cardiac tissue engineering and role of immune modulation in tissue regeneration. Int J Nanomed. 2019;14:1311.
Thomas D, Choi S, Alamana C, Parker KK, Wu JC. Cellular and engineered organoids for cardiovascular models. Circ Res. 2022;130(12):1780–802.
Zhao Y, Rafatian N, Feric NT, Cox BJ, Aschar-Sobbi R, Wang EY, et al. A platform for generation of chamber-specific cardiac tissues and disease modeling. Cell. 2019;176(4):913–27. e18.
Lee SJ, Yoo JJ, Atala A. Biomaterials and tissue engineering. Clin Regen Med Urol. 2018;17–51.
Chandika P, Heo S-Y, Kim T-H, Oh G-W, Kim G-H, Kim M-S, et al. Recent advances in biological macromolecule based tissue-engineered composite scaffolds for cardiac tissue regeneration applications. Int J Biol Macromol. 2020;164:2329–57.
Sheehy SP, Grosberg A, Qin P, Behm DJ, Ferrier JP, Eagleson MA, et al. Toward improved myocardial maturity in an organ-on-chip platform with immature cardiac myocytes. Exp Biol Med. 2017;242(17):1643–56.
Saludas L, Pascual-Gil S, Prósper F, Garbayo E, Blanco-Prieto M. Hydrogel based approaches for cardiac tissue engineering. Int J Pharm. 2017;523(2):454–75.
Fujita B, Zimmermann W-H. Myocardial tissue engineering for regenerative applications. Curr Cardiol Rep. 2017;19(9):1–10.
Zhang J, Zhu W, Radisic M, Vunjak-Novakovic G. Can we engineer a human cardiac patch for therapy? Circ Res. 2018;123(2):244–65.
Yan Q, Dong H, Su J, Han J, Song B, Wei Q, et al. A review of 3D printing technology for medical applications. Engineering. 2018;4(5):729–42.
Xiang Y, Miller K, Guan J, Kiratitanaporn W, Tang M, Chen S. 3D bioprinting of complex tissues in vitro: state-of-the-art and future perspectives. Arch Toxicol. 2022;1–20.
Askari M, Naniz MA, Kouhi M, Saberi A, Zolfagharian A, Bodaghi M. Recent progress in extrusion 3D bioprinting of hydrogel biomaterials for tissue regeneration: a comprehensive review with focus on advanced fabrication techniques. Biomaterials science. 2021;9(3):535–73.
Moroni L, Burdick JA, Highley C, Lee SJ, Morimoto Y, Takeuchi S, et al. Biofabrication strategies for 3D in vitro models and regenerative medicine. Nat Rev Mater. 2018;3(5):21–37.
Jang J, Park H-J, Kim S-W, Kim H, Park JY, Na SJ, et al. 3D printed complex tissue construct using stem cell-laden decellularized extracellular matrix bioinks for cardiac repair. Biomaterials. 2017;112:264–74.
Izadifar M, Chapman D, Babyn P, Chen X, Kelly ME. UV-assisted 3D bioprinting of nanoreinforced hybrid cardiac patch for myocardial tissue engineering. Tissue Eng Part C Methods. 2018;24(2):74–88.
Van Eijnatten M, van Dijk R, Dobbe J, Streekstra G, Koivisto J, Wolff J. CT image segmentation methods for bone used in medical additive manufacturing. Med Eng Phys. 2018;51:6–16.
Ripley B, Levin D, Kelil T, Hermsen JL, Kim S, Maki JH, et al. 3D printing from MRI data: harnessing strengths and minimizing weaknesses. J Magn Reson Imaging. 2017;45(3):635–45.
Jafari A, Ajji Z, Mousavi A, Naghieh S, Bencherif SA, Savoji H. Latest advances in 3D bioprinting of cardiac tissues. Adv Mater Technol. 2022;2101636.
Jang J. 3D bioprinting and in vitro cardiovascular tissue modeling. Bioengineering. 2017;4(3):71.
Liu J, Miller K, Ma X, Dewan S, Lawrence N, Whang G, et al. Direct 3D bioprinting of cardiac micro-tissues mimicking native myocardium. Biomaterials. 2020;256: 120204.
Lee S, Sani ES, Spencer AR, Guan Y, Weiss AS, Annabi N. Human-recombinant-elastin-based bioinks for 3D bioprinting of vascularized soft tissues. Adv Mater. 2020;32(45):2003915.
Papaioannou TG, Manolesou D, Dimakakos E, Tsoucalas G, Vavuranakis M, Tousoulis D. 3D bioprinting methods and techniques: applications on artificial blood vessel fabrication. Acta Cardiologica Sinica. 2019;35(3):284.
Cho S, Discher DE, Leong KW, Vunjak-Novakovic G, Wu JC. Challenges and opportunities for the next generation of cardiovascular tissue engineering. Nat Methods. 2022;19(9):1064–71.
Puluca N, Lee S, Doppler S, Münsterer A, Dreßen M, Krane M, et al. Bioprinting approaches to engineering vascularized 3D cardiac tissues. Curr Cardiol Rep. 2019;21(9):1–11.
Hu JB, Tomov ML, Buikema JW, Chen C, Mahmoudi M, Wu SM, et al. Cardiovascular tissue bioprinting: physical and chemical processes. Appl Phys Rev. 2018;5(4): 041106.
Ligon SC, Liska R, Stampfl J, Gurr M, Mülhaupt R. Polymers for 3D printing and customized additive manufacturing. Chem Rev. 2017;117(15):10212–90.
Huang G, Li F, Zhao X, Ma Y, Li Y, Lin M, et al. Functional and biomimetic materials for engineering of the three-dimensional cell microenvironment. Chem Rev. 2017;117(20):12764–850.
Nikolova MP, Chavali MS. Recent advances in biomaterials for 3D scaffolds: a review. Bioactive materials. 2019;4:271–92.
Cui H, Nowicki M, Fisher JP, Zhang LG. 3D bioprinting for organ regeneration. Adv Healthcare Mater. 2017;6(1):1601118.
Catoira MC, Fusaro L, Di Francesco D, Ramella M, Boccafoschi F. Overview of natural hydrogels for regenerative medicine applications. J Mater Sci - Mater Med. 2019;30(10):1–10.
Wang X, Ao Q, Tian X, Fan J, Tong H, Hou W, et al. Gelatin-based hydrogels for organ 3D bioprinting. Polymers. 2017;9(9):401.
Ying G, Jiang N, Yu C, Zhang YS. Three-dimensional bioprinting of gelatin methacryloyl (GelMA). Bio-Design and Manufacturing. 2018;1(4):215–24.
Rastogi P, Kandasubramanian B. Review of alginate-based hydrogel bioprinting for application in tissue engineering. Biofabrication. 2019;11(4): 042001.
Jeon O, Lee YB, Hinton TJ, Feinberg AW, Alsberg E. Cryopreserved cell-laden alginate microgel bioink for 3D bioprinting of living tissues. Materials Today Chemistry. 2019;12:61–70.
Hull SM, Brunel LG, Heilshorn SC. 3D bioprinting of cell-laden hydrogels for improved biological functionality. Adv Mater. 2022;34(2):2103691.
Bhattacharyya A, Janarthanan G, Noh I. Nano-biomaterials for designing functional bioinks towards complex tissue and organ regeneration in 3D bioprinting. Addit Manuf. 2021;37: 101639.
Liu J, He J, Liu J, Ma X, Chen Q, Lawrence N, et al. Rapid 3D bioprinting of in vitro cardiac tissue models using human embryonic stem cell-derived cardiomyocytes. Bioprinting. 2019;13: e00040.
Mehrotra S, de Melo BA, Hirano M, Keung W, Li RA, Mandal BB, et al. Nonmulberry silk based ink for fabricating mechanically robust cardiac patches and endothelialized myocardium-on-a-chip application. Adv Func Mater. 2020;30(12):1907436.
Wang X. Advanced polymers for three-dimensional (3D) organ bioprinting. Micromachines. 2019;10(12):814.
Shin YJ, Shafranek RT, Tsui JH, Walcott J, Nelson A, Kim D-H. 3D bioprinting of mechanically tuned bioinks derived from cardiac decellularized extracellular matrix. Acta Biomater. 2021;119:75–88.
Cui H, Liu C, Esworthy T, Huang Y, Yu Z-x, Zhou X, et al. 4D physiologically adaptable cardiac patch: a 4-month in vivo study for the treatment of myocardial infarction. Sci Adv. 2020;6(26):eabb5067.
de Melo BA, Jodat YA, Cruz EM, Benincasa JC, Shin SR, Porcionatto MA. Strategies to use fibrinogen as bioink for 3D bioprinting fibrin-based soft and hard tissues. Acta Biomater. 2020;117:60–76.
Tang M, Rich JN, Chen S. Biomaterials and 3D bioprinting strategies to model glioblastoma and the blood–brain barrier. Adv Mater. 2021;33(5):2004776.
Roy A, Saxena V, Pandey LM. 3D printing for cardiovascular tissue engineering: a review. Mater Technol. 2018;33(6):433–42.
You S, Wang P, Schimelman J, Hwang HH, Chen S. High-fidelity 3D printing using flashing photopolymerization. Addit Manuf. 2019;30: 100834.
Xie H, Yang K-K, Wang Y-Z. Photo-cross-linking: a powerful and versatile strategy to develop shape-memory polymers. Prog Polym Sci. 2019;95:32–64.
Yu C, Ma X, Zhu W, Wang P, Miller KL, Stupin J, et al. Scanningless and continuous 3D bioprinting of human tissues with decellularized extracellular matrix. Biomaterials. 2019;194:1–13.
Yu C, You S, Zhu W, Sun B, Chen S. DMD-based rapid 3D bioprinting for precision tissue engineering and regenerative medicine. Emerging Digital Micromirror Device Based Systems and Applications XII: SPIE; 2020. p. 15–26.
Zhu W, Qu X, Zhu J, Ma X, Patel S, Liu J, et al. Direct 3D bioprinting of prevascularized tissue constructs with complex microarchitecture. Biomaterials. 2017;124:106–15.
Liu W, Heinrich MA, Zhou Y, Akpek A, Hu N, Liu X, et al. Extrusion bioprinting of shear-thinning gelatin methacryloyl bioinks. Adv Healthcare Mater. 2017;6(12):1601451.
Alruwaili M, Lopez JA, McCarthy K, Reynaud EG, Rodriguez BJ. Liquid-phase 3D bioprinting of gelatin alginate hydrogels: influence of printing parameters on hydrogel line width and layer height. Bio-Design and Manufacturing. 2019;2(3):172–80.
Paxton N, Smolan W, Böck T, Melchels F, Groll J, Jungst T. Proposal to assess printability of bioinks for extrusion-based bioprinting and evaluation of rheological properties governing bioprintability. Biofabrication. 2017;9(4): 044107.
Skylar-Scott MA, Mueller J, Visser CW, Lewis JA. Voxelated soft matter via multimaterial multinozzle 3D printing. Nature. 2019;575(7782):330–5.
Davoodi E, Sarikhani E, Montazerian H, Ahadian S, Costantini M, Swieszkowski W, et al. Extrusion and microfluidic-based bioprinting to fabricate biomimetic tissues and organs. Advanced materials technologies. 2020;5(8):1901044.
Boularaoui S, Al Hussein G, Khan KA, Christoforou N, Stefanini C. An overview of extrusion-based bioprinting with a focus on induced shear stress and its effect on cell viability. Bioprinting. 2020;20: e00093.
Ramesh S, Harrysson OL, Rao PK, Tamayol A, Cormier DR, Zhang Y, et al. Extrusion bioprinting: Recent progress, challenges, and future opportunities. Bioprinting. 2021;21: e00116.
Gillispie G, Prim P, Copus J, Fisher J, Mikos AG, Yoo JJ, et al. Assessment methodologies for extrusion-based bioink printability. Biofabrication. 2020;12(2): 022003.
Li X, Liu B, Pei B, Chen J, Zhou D, Peng J, et al. Inkjet bioprinting of biomaterials. Chem Rev. 2020;120(19):10793–833.
Matai I, Kaur G, Seyedsalehi A, McClinton A, Laurencin CT. Progress in 3D bioprinting technology for tissue/organ regenerative engineering. Biomaterials. 2020;226: 119536.
Jang J, Park JY, Gao G, Cho D-W. Biomaterials-based 3D cell printing for next-generation therapeutics and diagnostics. Biomaterials. 2018;156:88–106.
Vikram Singh A, Hasan Dad Ansari M, Wang S, Laux P, Luch A, Kumar A, et al. The adoption of three-dimensional additive manufacturing from biomedical material design to 3D organ printing. Appl Sci. 2019;9(4):811.
Rahmani Dabbagh S, Rezapour Sarabi M, Birtek MT, Mustafaoglu N, Zhang YS, Tasoglu S. 3D bioprinted organ‐on‐chips. Aggregate. 2022;e197.
Wang Z, Kapadia W, Li C, Lin F, Pereira RF, Granja PL, et al. Tissue-specific engineering: 3D bioprinting in regenerative medicine. J Control Release. 2021;329:237–56.
Alonzo M, AnilKumar S, Roman B, Tasnim N, Joddar B. 3D Bioprinting of cardiac tissue and cardiac stem cell therapy. Transl Res. 2019;211:64–83.
Hong N, Yang GH, Lee J, Kim G. 3D bioprinting and its in vivo applications. J Biomed Mater Res B Appl Biomater. 2018;106(1):444–59.
Harley WS, Li CC, Toombs J, O’Connell CD, Taylor HK, Heath DE, et al. Advances in biofabrication techniques towards functional bioprinted heterogeneous engineered tissues: a comprehensive review. Bioprinting. 2021;23: e00147.
Koch L, Deiwick A, Franke A, Schwanke K, Haverich A, Zweigerdt R, et al. Laser bioprinting of human induced pluripotent stem cells—the effect of printing and biomaterials on cell survival, pluripotency, and differentiation. Biofabrication. 2018;10(3): 035005.
Wang Z, Jin X, Tian Z, Menard F, Holzman JF, Kim K. A Novel, Well-resolved direct laser bioprinting system for rapid cell encapsulation and microwell fabrication. Adv Healthcare Mater. 2018;7(9):1701249.
Kačarević ŽP, Rider PM, Alkildani S, Retnasingh S, Smeets R, Jung O, et al. An introduction to 3D bioprinting: possibilities, challenges and future aspects. Materials. 2018;11(11):2199.
Dobos A, Van Hoorick J, Steiger W, Gruber P, Markovic M, Andriotis OG, et al. Thiol–gelatin–norbornene bioink for laser-based high-definition bioprinting. Adv Healthcare Mater. 2020;9(15):1900752.
Song J, Michas C, Chen CS, White AE, Grinstaff MW. From simple to architecturally complex hydrogel scaffolds for cell and tissue engineering applications: opportunities presented by two-photon polymerization. Adv Healthcare Mater. 2020;9(1):1901217.
Mao M, He J, Li X, Zhang B, Lei Q, Liu Y, et al. The emerging frontiers and applications of high-resolution 3D printing. Micromachines. 2017;8(4):113.
Jonušauskas L, Juodkazis S, Malinauskas M. Optical 3D printing: bridging the gaps in the mesoscale. J Opt. 2018;20(5): 053001.
Bouzin M, Zeynali A, Marini M, Sironi L, Scodellaro R, D’Alfonso L, et al. Multiphoton laser fabrication of hybrid photo-activable biomaterials. Sensors. 2021;21(17):5891.
Dabbagh SR, Sarabi MR, Birtek MT, Seyfi S, Sitti M, Tasoglu S. 3D-printed microrobots from design to translation. Nat Commun. 2022;13(1):1–24.
Ayuso JM, Virumbrales-Munoz M, McMinn PH, Rehman S, Gomez I, Karim MR, et al. Tumor-on-a-chip: a microfluidic model to study cell response to environmental gradients. Lab Chip. 2019;19(20):3461–71.
Velasco-Mallorquí F, Rodríguez-Comas J, Ramón-Azcón J. Cellulose-based scaffolds enhance pseudoislets formation and functionality. Biofabrication. 2021;13(3): 035044.
Soliman BG, Major GS, Atienza-Roca P, Murphy CA, Longoni A, Alcala-Orozco CR, et al. Development and characterization of gelatin-norbornene bioink to understand the interplay between physical architecture and micro-capillary formation in biofabricated vascularized constructs. Adv Healthcare Mater. 2022;11(2):2101873.
•• Liu Y, Zhang Y, Mei T, Cao H, Hu Y, Jia W, et al. hESCs-derived early vascular cell spheroids for cardiac tissue vascular engineering and myocardial infarction treatment. Advanced Science. 2022;9(9):2104299. Findings from the research uncover hESCs-derived EVC spheroids rather than single cells are more accessible for complex vasculature engineering, which is of great potential for cardiac tissue vascular engineering and MI treatment by cell therapy.
Peate I. The circulatory system. British Journal of Healthcare Assistants. 2020;14(11):548–53.
Lee SE, Park YS. The role of bacterial cellulose in artificial blood vessels. Mol Cell Toxicol. 2017;13(3):257–61.
Wang L, Xin X, Li P, Dou J, Han X, Shen J, et al. Stepwise immobilization of keratin-dopamine conjugates and gold nanoparticles on PET sheets for potential vascular graft with the catalytic generation of nitric oxide. Colloids Surf, B. 2021;205: 111855.
Chang WG, Niklason LE. A short discourse on vascular tissue engineering. NPJ Regenerative medicine. 2017;2(1):1–8.
Wadey K, Lopes J, Bendeck M, George S. Role of smooth muscle cells in coronary artery bypass grafting failure. Cardiovasc Res. 2018;114(4):601–10.
•• Wang D, Maharjan S, Kuang X, Wang Z, Mille LS, Tao M, et al. Microfluidic bioprinting of tough hydrogel-based vascular conduits for functional blood vessels. Sci Adv. 2022;8(43):eabq6900. This study presents biofabrication of mechanically and functionally relevant vascular conduits, showcasing their potentials as vascular models for disease studies in vitro and as grafts for vascular surgeries in vivo, possibly serving broad biomedical applications in the future.
Skylar-Scott MA, Uzel SG, Nam LL, Ahrens JH, Truby RL, Damaraju S, et al. Biomanufacturing of organ-specific tissues with high cellular density and embedded vascular channels. Sci Adv. 2019;5(9):eaaw2459.
Miller KL, Xiang Y, Yu C, Pustelnik J, Wu J, Ma X, et al. Rapid 3D bioprinting of a human iPSC-derived cardiac micro-tissue for high-throughput drug testing. Organs-on-a-Chip. 2021;3: 100007.
Samson AAS, Song JM. Scaffold-free 3D printing for fabrication of biomimetic branched multinucleated cardiac tissue construct: a promising ex vivo model for in situ detection of drug-induced sodium ion channel responses. Appl Mater Today. 2022;27: 101416.
•• Ahrens JH, Uzel SG, Skylar‐Scott M, Mata MM, Lu A, Kroll KT, et al. Programming cellular alignment in engineered cardiac tissue via bioprinting anisotropic organ building blocks. Adv Mater. 2022:2200217. Findings from this research showed that a bioink composed of contractile cardiac aOBBs is first generated and aligned cardiac tissue sheets with linear, spiral, and chevron features are printed. Finally, the ability to spatially control the magnitude and direction of contractile force by printing cardiac sheets with different aOBB alignment is highlighted.
Funding
This project is supported in part by grants from the US National Science Foundation (2135720) and National Institutes of Health (R21ES034455).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lu, TY., Xiang, Y., Tang, M. et al. 3D Printing Approaches to Engineer Cardiac Tissue. Curr Cardiol Rep 25, 505–514 (2023). https://doi.org/10.1007/s11886-023-01881-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-023-01881-y