Abstract
Purpose of Review
Addressing cardiometabolic risk factors in persons with serious mental illness requires early screening and proactive medical management in both medical and mental health settings.
Recent Findings
Cardiovascular disease remains the leading cause of death for persons with serious mental illness (SMI), such as schizophrenia or bipolar disorder, much of which is driven by a high prevalence of metabolic syndrome, diabetes, and tobacco use. We summarize barriers and recent approaches to screening and treatment for metabolic cardiovascular risk factors within physical health and specialty mental health settings.
Summary
Incorporating system-based and provider-level support within physical health and psychiatric clinical settings should contribute to improvement for screening, diagnosis, and treatment for cardiometabolic conditions for patients with SMI. Targeted education for clinicians and leveraging multi-disciplinary teams are important first steps to recognize and treat populations with SMI at risk of CVD.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is the leading cause of death for persons with serious mental illness (SMI), such as schizophrenia, schizoaffective disorder, or bipolar disorder [1]. It directly contributes to premature mortality by 10–20 years compared with populations without mental illness—unfortunately, this gap has not narrowed in the past few decades [1,2,3].
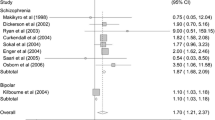
Much of this mortality disparity is driven by the high prevalence of cardiometabolic risk factors, tobacco use and low rates of physical activity in populations with SMI [4,5,6,7]. Cardiometabolic risk factors (diabetes mellitus, dyslipidemia, hypertension, and overweight/obesity) are a set of risk factors that contribute to the development of CVD [8]. Estimates suggest that people with serious mental illness may have nearly a twofold risk of developing diabetes compared with those without serious mental illness [4]. Estimates of the prevalence of diabetes range from 13 to 18% and 10 to 61% for hypertension in populations with SMI [9, 10]. The use of antipsychotic medication may further elevate their risk of metabolic syndrome through weight gain and altered glucose metabolism [11, 12]. In addition, approximately half of individuals with SMI smoke tobacco, with higher rates observed in individuals with a schizophrenia diagnosis [7, 13]. The goal of this paper is to summarize the known barriers and current strategies to address these barriers in the following domains: screening, diagnosis, treatment, and control of cardiometabolic risk factors. We also include approaches for engaging patients with SMI in disease management who have a diagnosis with a CVD risk factor.
Continuum of Care for Cardiometabolic Conditions
We focus on cardiometabolic risk factors as all are targeted through early identification and interventions, including overlapping strategies for lifestyle modification [14]. In addition, screening for most of these conditions has long been a recommended priority within psychiatry and general medical care [15]. Management of these cardiometabolic risk factor conditions operates as a continuum of care: screening, diagnosis, treatment, and control (Fig. 1).
Screening and Diagnosis
The goal of screening is to identify potential diseases, particularly in asymptomatic patients, in order to initiate treatment at an early disease stage and reduce the progression of disease [16]. Evidence shows control of cardiometabolic conditions significantly reduces the risk of mortality [14]. Populations who are at elevated risk of developing disease, such as by demographics (age, race/ethnicity), family history, other comorbid conditions (e.g., chronic kidney disease), or iatrogenic causes (e.g., psychotropic medication), should be screened at earlier and more frequent intervals [14, 17]. Studies indicate that people with schizophrenia are less likely to receive recommended screenings for diabetes, hyperlipidemia, and obesity than those without mental illness [18,19,20,21].
Treatment and Control
Treatment of cardiometabolic conditions focuses on achieving recommended targets for the given risk factor: glycemic control for diabetes, blood pressure control for hypertension, reduction in blood cholesterol for dyslipidemia, and weight reduction for obesity [14]. In many studies, patients with SMI are less likely to receive guideline-concordant care for these cardiometabolic conditions than those without SMI [6, 21]. In one study of 1433 participants with schizophrenia, 70% of individuals with diabetes received hypoglycemic agent, but only 38% of individuals with hypertension received pharmacologic treatment and 12% of individuals with dyslipidemia received pharmacologic treatment, such as with a statin [22]. In another study, individuals with schizophrenia and diabetes were less likely to receive recommended lipid testing, eye exams, monitoring of hemoglobin A1c values compared with individuals without schizophrenia [21]. Yet in other studies, no differences in rates of guideline-concordant care were observed. However, many of these studies noted overall low rates of guideline-concordant care, which suggests that there is need for improvement in quality metrics. Rates also appear lower in Medicaid populations and higher in Veteran’s Administration populations, suggesting additional variation across health insurer and healthcare delivery system [6].
Barriers to Care
Patient-Level Barriers
Patients with SMI are likely to experience disadvantages of low socioeconomic status, low educational attainment, unemployment, social isolation, homelessness, criminal justice involvement, and substance use disorder, all of which are associated with an increased risk of developing cardiometabolic conditions [23,24,25,26]. They may also be more likely to live in congregate settings, with limited control of menu planning and choice of healthy foods.
Patients with schizophrenia may have cognitive dysfunction or experience disorganized thought processes as part of a psychotic disorder and are among the fastest growing subgroup of beneficiaries of disability [25, 27]. Such cognitive difficulties may only add to patient challenges in navigating a complex healthcare system [28]. Furthermore, patients with SMI, as with those without SMI, require knowledge of how to self-manage their underlying cardiometabolic conditions. They may benefit from additional educational sessions with information broken into small components [29, 30]. Cognitive challenges could influence a patient’s ability to schedule recommended testing and follow-up. As much of chronic disease care relies on regular follow-up (e.g., monitoring of blood pressure, hemoglobin A1c), delays in care may result. Studies report an association between delays in seeking medical care and SMI status [31, 32].
Provider-Level Barriers
Challenges in who provides physical healthcare and how it is implemented are observed from both primary care and psychiatry perspectives. Primary care physicians and psychiatrists envision a shared responsibility for the care of patients with SMI and want a shared consultative model to implement such care in both primary care and mental health settings [33–36]. However, in many settings, there remains a lack of a clarity as to how such responsibility is divided and the specific roles of each provider [33, 36].
Physical healthcare providers report a lack of time to address screenings and treatment plans and feel less prepared to engage in shared decision-making with patients with SMI who may also experience communication challenges [37,38,39]. Specifically, some have noted that they feel concerned about their ability to assess a patient’s capacity to make decisions or how to discuss follow-up plans for future health scenarios [40]. Primary care physicians report challenges with communicating if patients with SMI have significant psychiatric symptoms that they feel are not well controlled [40, 41].
Importantly, many patients with SMI may see their psychiatrists or other mental health clinicians more frequently than a primary care physician [42]. Persons with SMI are less likely to be seen in primary care clinics than those without SMI [43, 44]. Yet, many psychiatrists report a lack of a systematic approach for screening for cardiometabolic conditions and insufficient time to incorporate screenings into their practice, particularly when patients have psychiatric illness needs [34, 35]. Others express concern that they lack sufficient training and it is out of their scope of practice. Psychiatrists also report challenges in arranging medical follow-up [35].
Persons with SMI also report experiencing stigma from healthcare providers, which may act as an additional deterrent to engaging with healthcare providers, attending visits, and adhering to recommended treatment plans [39, 41, 45]. The stigma that they may experience may reflect implicit biases around mental illness [46, 47]. Implicit bias is an automatic, unintentional process, where stereotypes are activated and influence judgments and behaviors [46]. In other marginalized populations, implicit bias has been associated with differences in acute pain management, treatment of myocardial infarction, and asthma exacerbations [46, 48]. In a study of 166 healthcare providers, participants who endorsed stigmatizing characteristics of a patient with schizophrenia were less likely to refer to specialist care, refill non-steroidal pain medication, and to endorse that patient would not be adherent to treatment for low back pain [37]. However, few further studies on implicit bias and clinical decision-making have been conducted with an SMI population.
In practice, healthcare providers, whether through implicit biases or being unaware of additional risk factors, may be underestimating the risk of CVD in populations with SMI and therefore under-treat this population [22]. In one US-based health system, the mean 10-year risk of developing ASCVD was significantly higher in populations aged 40–75 years with SMI compared with those without SMI [9]. Moreover, this risk of developing cardiovascular disease is not isolated to older adults. When a 30-year risk of developing CVD was calculated using the Framingham risk score in adults ages 18–59 years, as many as 25% of adults with SMI were observed to be in the highest risk category compared with 11% of adults without SMI [9]. In addition, the use of antipsychotic medication may be an additional risk enhancer for CVD independent of traditional of other cardiometabolic risk factors; it is captured in CVD risk calculation scores in the UK but not in the USA [11, 12, 14, 49].
System-Level Barriers
System-level and structural barriers disproportionately affect populations with SMI, which likely strongly influence both the prevalence and management of cardiometabolic risk factors [23, 28]. First, the physical and mental healthcare systems have traditionally been siloed apart from one another, contributing to fragmentation of care [50]. Physical healthcare providers and mental healthcare providers may not share electronic health records, much less co-located, physical space-key attributes that promote coordination of care across providers [51]. Second, many persons with SMI face structural barriers, such as lack of transportation to medical appointments and limited financial resources for medication and appointment copayments [28]. Approximately 20–25% of the population who experience homelessness also have a diagnosis of SMI [52]. There also remains limited support for individuals with disabilities through employment opportunities, social programs, and community resources [53].
A majority of people with SMI have insurance, with most being publicly insured [54]. However, younger individuals with schizophrenia may have more frequent and longer gaps in insurance coverage (“churn”) and primary care access than those without schizophrenia [55, 56]. Within 1 year, 54% of individuals aged 18–34 years with schizophrenia were noted to have a disruption in insurance compared with 37% of similarly aged individuals without schizophrenia [55]. As a consequence of gaps in insurance, there may be delays in seeing medical providers or attaining recommended screening tests. In addition, access to mental healthcare remains a barrier, with community mental health clinics being underfunded and only a limited number of psychiatrists available within a given insurance network [57].
Strategies to Address Barriers
Given the multi-level barriers present to care for individuals with SMI with cardiometabolic conditions, current strategies have focused on how healthcare is organized and delivered, with an emphasis on early identification of cardiometabolic conditions through place-based and population health-based strategies.
Organization of Healthcare Delivery
Bring Physical Health Services to Mental Health Programs
As populations with SMI are frequently seen at mental health clinics, delivery models (e.g., reverse-integration programs, health homes) have sought to bring physical health services to specialty mental health programs [20, 58,59,60,61]. Over the past decade, these models have increasingly been implemented in the USA through Substance Abuse and Mental Health Services Administration’s (SAMHSA), a branch of the US Department of Health and Human Services Primary Behavioral Health Care Integration (PBHCI) program and the Affordable Care Act Medicaid health home waiver [20, 60]. The Medicaid health home waiver allows specialty mental health programs to bill for care management and care coordination services, which traditionally has not been reimbursable; to date, 17 US States and the District of Columbia have implemented this waiver program for health homes [62]. Models have been implemented in three ways: (1) co-located primary care providers embedded within mental health clinic or team; (2) psychiatrists initiate management of common chronic conditions using algorithms with a primary care physician acting as consultant, or (3) [nurse] care manager tasked with coordinating physical healthcare but embedded within mental health setting [20, 34, 59, 63, 64].
In the first model, primary care physicians and psychiatrists are co-located onsite within a community mental health center [65]. This model allows primary care physicians and psychiatrists to deliver their usual practice and to collaborate when needed for mutual patients [65, 66]. However, this model is uncommon, with less than a quarter of community mental health sites offering integrated primary care [66]. Facilities likely need a high level of resources to implement and support delivery of primary care (e.g., quality, accreditation, availability of wellness services), which itself may be a high barrier for sites serving smaller number of patients [20, 66].
In the second model, psychiatrists are tasked with screening for common cardiometabolic conditions, counseling patients to reduce risk of cardiometabolic conditions, limiting side effects from psychotropic medications, and to initiate treatment for common cardiometabolic conditions (e.g., metformin for diabetes) until patients can be connected to general medical services [34, 36]. These programs have the advantage to reach populations with SMI who are actively engaged with their mental healthcare providers and reduce the burden of patients needing to go elsewhere to receive their physical healthcare [20, 58, 59, 61]. However, some psychiatrists express discomfort that treatment of cardiometabolic conditions is out of their skillset [35, 67]. More training and support is needed for psychiatry trainees and practicing psychiatrists, including cross-training opportunities for psychiatrists to work collaboratively with general medical and social services [34, 36]. In addition, this model depends on referral for physical health services after screening/diagnosis and does not address long-term treatment and control of cardiometabolic conditions for patients with SMI [34].
In the third model, a care manager, often a nurse, is embedded within a community mental health clinic [63]. The care manager acts to coordinate across physical health (often primary care) and behavioral health services and deliver care management services [68]. Notably, primary care is not co-located in this model and often is in a separate health system. One clinical trial intervention successfully leveraged a nurse care manager and health coaches, who were embedded within community mental health clinics, to reduce overall CVD risk for adults with SMI and at least one CVD risk factor [69••]. Here, the nurse developed an individual care plan, worked with participants around their individual health goal, and coordinated care. The health coaches delivered education around health behaviors related to CVD risk with material edited for improved readability given that many participants experienced cognitive dysfunction and low health literacy [25]. Continual communication, regular check-ins and follow-up, accountability, and support of patient goals were identified as key components [70]. However, in non-clinical trial settings, results have been more limited, particularly those funded through the public insurance-based, Medicaid waiver health home program [20]. Programs report improvement in screening rates of cardiometabolic conditions but no improvement in treatment of cardiometabolic conditions, such as glycemic control or blood pressure control [20]. Programs face barriers around communication when the care manager is not able to see existing electronic health records and must rely on phone calls or faxes to obtain updated medical records [63]. Such barriers may further contribute to miscommunication or delays in care. Some programs also report a lack of capacity for population health management, a staple nowadays in chronic disease care and monitoring [20, 71]. Greater investment in information technology, workforce development, and financing is required [72].
Support Physical Healthcare Clinics with Mental Health Professionals
Persons with SMI also report wanting to be seen in primary care [41]. The Collaborative Care Model (CCM) incorporates a psychiatrist and other mental health professionals into a primary care practice, with early studies focusing on providing mental health treatment [73,74,75]. However, later studies have examined whether CCM could improve delivery of physical healthcare for patients with SMI [76, 77]. In one small study, patients with psychosis and poorly controlled diabetes were assigned care to a team featuring a nurse care manager, psychiatrist, primary care provider, and endocrinology consultant. Diabetes education was delivered using motivational interviewing and behavioral activation strategies and material was adapted to address specific needs of patients with psychosis. After 3 months, mean hemoglobin A1c declined significantly for intervention-arm participants (9.4% to 8.0%) but did not significantly change for control arm participants (8.3 to 8.0%) [77]. No differences were observed for blood pressure control. In this model, participants also received mental healthcare at the CCM.
Facilitators of this model include the presence of a team member with a specialist mental health background (e.g., care manager, care provider) who communicates effectively with primary care providers and receives support from healthcare clinic/system and patients with SMI who are open to working with the care manager [78]. Care providers could enhance a primary care physician’s understanding of a patient with SMI’s concerns, while a primary care physician could increase the care manager’s understanding of why a specific chronic condition should be prioritized. In turn, the care provider could then help to introduce these topics to the patient. Mean healthcare costs are higher for patients with SMI compared with SMI, particularly if they have a common chronic condition, such as diabetes or chronic kidney disease [79]. Given that primary care practices may have a small proportion of patients with SMI and limited resources, practices may wish to direct CCM resources towards patients with SMI who also have a major chronic condition.
Barriers occur when care managers lack the support of supervisors or primary care physicians, lack the knowledge or skills required to deliver chronic disease education, or struggle with use of information technology, which is often a primary means of communication [78]. More work is needed to understand the training, education, and infrastructure needed to support healthcare professionals who may not be used to working with patients with SMI.
Strategies to Support Healthcare Providers
Use of Clinical Decision Support Tools
Clinical decision support systems leverage informatics systems (e.g., electronic health records) to assist clinicians with delivering evidence-based care by taking existing information on a specific patient to recommend specific screening tests, medications, and treatment goals [80]. In a recent trial of adult patients with SMI (defined as schizophrenia, schizoaffective disorder, or bipolar disorder), 76 primary care clinics were randomized across three health systems for primary care physicians and psychiatrists to receive best practice advisory prompts based on a patient’s modifiable CVD risk profile [81••]. Across the 12-month intervention, the intervention was associated with a net 4% decrease in total modifiable CVD risk. Investigators calculated this intervention could prevent 3 events per 1000 patients. Patients who were younger (aged 18–29 years) or middle-aged (aged 50–59 years), Black or White were more likely to benefit from the intervention; however, no significant treatment effects were observed for individual CVD risk factors [81••].
One benefit of these decision support systems is that they can be implemented within any specialty (e.g., internal medicine, psychiatry), modified according to relevant populations, and used in combination with other interventions, such as team-based care models [80]. Best practice alerts in other settings have been shown to improve laboratory-based metabolic monitoring while a patient is prescribed antipsychotic medication [82, 83]. However, studies note that clinicians may override alerts due to fatigue from overuse of alerts or having alerts that are not well targeted to specific patients [84]. Future work is needed to understand how clinical decision supports may be used with populations with SMI, who may be at risk of under-diagnosis of ASCVD [9].
Leverage Multi-disciplinary Teams
As described earlier, use of multi-disciplinary teams where the healthcare is delivered (primary care clinic vs mental health clinic location) is increasingly being leveraged to care for populations with SMI around CVD risk factors. Programs using individual and group weight management sessions have been shown to be effective in populations with SMI [85]. Yet work is needed around how to adapt existing evidence-based programs (e.g., diabetes prevention program, weight management) in real-world settings [86].
Employing educators who are not physicians to deliver critical health education also may address known time shortages within traditional clinic visits. One common theme is to leverage healthcare team members who have experience working with persons with SMI and who can help to educate other healthcare team members around specific care needs that populations with SMI may require [59, 63, 77, 78]. Health coaches can help individuals with SMI learn how to identify their health goals and to self-manage cardiometabolic conditions [69••]. One ongoing intervention is training direct care staff at specialty mental health clinics to conduct evidence-based CVD care coordination through a team-based implementation strategy [87]. All may use motivational interviewing to deliver this educational material [88].
Another resource are peers with lived experience with SMI. In one study, they have been shown to promote self-management and self-efficacy around diabetes management [89]. In another study of 400 patients across 6 months, peers helped to positively engage participants around self-management of chronic conditions and improved quality of life [90]. Peers may be powerful role models for patients through relating to their challenges and offering advice and promoting engagement in self-management programs [91]. Self-management programs around diabetes are feasible and acceptable to patients with SMI; however, little is known about their effectiveness as many trials exclude participants with SMI or have limited data available [92, 93].
Addressing Unconscious Bias
While stigma and implicit bias are known barriers, there is limited data as to how to address stigma and implicit bias among medical professionals [39, 41]. Contact-based interventions between groups with and without lived experience with SMI has been one strategy; in these interventions, a meeting (“contact”) is set up between an individual from the stigmatized group (here, individual with SMI) and individual from general population (here, medical professional) [94]. It often includes an educational component and occurs in an artificial setting [94]. However, available studies may lack the rigor of a control arm, are of limited duration, or have not been linked to behavioral changes [94, 95]. Studies have used anti-stigma educational training programs, increased contact with individuals with SMI (in-person, video), technology (e.g., virtual reality), and public activism approaches [95,96,97,98,99]. More rigorous studies targeting behavioral change are needed to elucidate mechanisms that both mediate stigma and promote change around caring for persons with SMI. In addition, more education is needed, including in medical school and residency for all specialities given that patients with SMI are at elevated risk for experiencing an adverse events during a medical-surgical hospitalization [100]. However, given the outsize proportion of premature mortality attributed to cardiometabolic conditions, such training is critical for psychiatry and general medical trainees who are more likely to care for this population.
Future Directions
While CVD remains a leading cause of mortality for persons with SMI, delivery models are increasingly focused on how to systematically screen populations and connect them to treatment for cardiometabolic conditions. Caring for populations with SMI at high risk for developing CVD is challenging with barriers at the system, provider, and patient level. Consequently, multi-level strategies will be required to address how healthcare is delivered to populations with SMI and how to engage them in evidence-based, patient-centered self-management of these chronic conditions.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006;3(2):A42.
Brown S. Excess mortality of schizophrenia. A meta-analysis. Br J Psychiatry : J Mental Sci. 1997;171:502–8.
Iturralde E, Slama N, Kline-Simon AH, Young-Wolff KC, Mordecai D, Sterling SA. Premature mortality associated with severe mental illness or substance use disorder in an integrated health care system. Gen Hosp Psychiatry. 2021;68:1–6. https://doi.org/10.1016/j.genhosppsych.2020.11.002.
Osborn DP, Wright CA, Levy G, King MB, Deo R, Nazareth I. Relative risk of diabetes, dyslipidaemia, hypertension and the metabolic syndrome in people with severe mental illnesses: systematic review and metaanalysis. BMC Psychiatry. 2008;8:84. https://doi.org/10.1186/1471-244x-8-84.
Dixon L, Weiden P, Delahanty J, et al. Prevalence and correlates of diabetes in national schizophrenia samples. Schizophr Bull. 2000;26(4):903–12. https://doi.org/10.1093/oxfordjournals.schbul.a033504.
McGinty EE, Baller J, Azrin ST, Juliano-Bult D, Daumit GL. Quality of medical care for persons with serious mental illness: a comprehensive review. Schizophr Res. 2015;165(2–3):227–35. https://doi.org/10.1016/j.schres.2015.04.010.
Cather C, Pachas GN, Cieslak KM, Evins AE. Achieving smoking cessation in individuals with schizophrenia: special considerations. CNS Drugs. 2017;31(6):471–81. https://doi.org/10.1007/s40263-017-0438-8.
Eckel RH, Kahn R, Robertson RM, Rizza RA. Preventing cardiovascular disease and diabetes. Circulation. 2006;113(25):2943–6. https://doi.org/10.1161/CIRCULATIONAHA.106.176583.
Rossom RC, Hooker SA, O’Connor PJ, Crain AL, Sperl-Hillen JM. Cardiovascular risk for patients with and without schizophrenia, schizoaffective disorder, or bipolar disorder. J Am Heart Assoc. 2022;11(6):e021444. https://doi.org/10.1161/jaha.121.021444.
Pérez-Piñar M, Mathur R, Foguet Q, Ayis S, Robson J, Ayerbe L. Cardiovascular risk factors among patients with schizophrenia, bipolar, depressive, anxiety, and personality disorders. Eur Psychiatry. 2016;35:8–15. https://doi.org/10.1016/j.eurpsy.2016.02.004.
De Hert M, Detraux J, Van Winkel R, Yu W, Correll CU. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol. 2011;8(2):114–26. https://doi.org/10.1038/nrendo.2011.156.
Tschoner A, Engl J, Laimer M, et al. Metabolic side effects of antipsychotic medication. Int J Clin Pract. 2007;61(8):1356–70. https://doi.org/10.1111/j.1742-1241.2007.01416.x.
Dickerson F, Schroeder J, Katsafanas E, et al. Cigarette smoking by patients with serious mental illness, 1999–2016: an increasing disparity. Psychiatr Serv. 2018;69(2):147–53. https://doi.org/10.1176/appi.ps.201700118.
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary. Circulation. 2019:Cir0000000000000677. https://doi.org/10.1161/cir.0000000000000677.
Marder SR, Cannon TD. Schizophrenia. N Engl J Med. 2019;381(18):1753–61. https://doi.org/10.1056/NEJMra1808803.
Classification and Diagnosis of Diabetes. Standards of medical care in diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S13-s27. https://doi.org/10.2337/dc18-S002.
American Diabetes Association; American Psychiatric Association; American Association of Clinical Endocrinologists; North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. J Clin Psychiatry. 2004;65(2):267–72. https://doi.org/10.4088/jcp.v65n0219.
Banta JE, Morrato EH, Lee SW, Haviland MG. Retrospective analysis of diabetes care in California Medicaid patients with mental illness. J Gen Intern Med. 2009;24(7):802–8. https://doi.org/10.1007/s11606-009-0994-9.
Mangurian C, Newcomer JW, Modlin C, Schillinger D. Diabetes and cardiovascular care among people with severe mental illness: a literature review. J Gen Intern Med. 2016;31(9):1083–91. https://doi.org/10.1007/s11606-016-3712-4.
Murphy KA, Daumit GL, Stone E, McGinty EE. Physical health outcomes and implementation of behavioural health homes: a comprehensive review. Int Rev Psychiatry (Abingdon, England). 2019:1–18. https://doi.org/10.1080/09540261.2018.1555153.
Kurdyak P, Vigod S, Duchen R, Jacob B, Stukel T, Kiran T. Diabetes quality of care and outcomes: comparison of individuals with and without schizophrenia. Gen Hosp Psychiatry. 2017;46:7–13. https://doi.org/10.1016/j.genhosppsych.2017.02.001.
Nasrallah HA, Meyer JM, Goff DC, et al. Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: data from the CATIE schizophrenia trial sample at baseline. Schizophr Res. 2006;86(1–3):15–22. https://doi.org/10.1016/j.schres.2006.06.026.
Diez Roux AV, Mujahid MS, Hirsch JA, Moore K, Moore LV. The impact of neighborhoods on CV risk. Glob Heart. 2016;11(3):353–63. https://doi.org/10.1016/j.gheart.2016.08.002.
Draine J, Salzer MS, Culhane DP, Hadley TR. Role of social disadvantage in crime, joblessness, and homelessness among persons with serious mental illness. Psychiatr Serv. 2002;53(5):565–73. https://doi.org/10.1176/appi.ps.53.5.565.
Mueser KT, McGurk SR. Schizophrenia Lancet. 2004;363(9426):2063–72. https://doi.org/10.1016/s0140-6736(04)16458-1.
Lin D, Kim H, Wada K, et al. Unemployment, homelessness, and other societal outcomes in patients with schizophrenia: a real-world retrospective cohort study of the United States Veterans Health Administration database: Societal burden of schizophrenia among US veterans. BMC Psychiatry. 2022;22(1):458. https://doi.org/10.1186/s12888-022-04022-x.
Drake RE, Frey W, Bond GR, et al. Assisting social security disability insurance beneficiaries with schizophrenia, bipolar disorder, or major depression in returning to work. Am J Psychiatry. 2013;170(12):1433–41. https://doi.org/10.1176/appi.ajp.2013.13020214.
Firth J, Siddiqi N, Koyanagi A, et al. The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. 2019. https://doi.org/10.1016/S2215-0366(19)30132-4.
Bartels SJ, Aschbrenner KA, Rolin SA, Hendrick DC, Naslund JA, Faber MJ. Activating older adults with serious mental illness for collaborative primary care visits. Psychiatr Rehabil J. 2013;36(4):278–288. Illness/Wellness Management for Individuals With Serious Mental Illnesses. https://doi.org/10.1037/prj0000024.
Dalcin AT, Jerome GJ, Appel LJ, et al. Need for cardiovascular risk reduction in persons with serious mental illness: design of a comprehensive intervention. Front Psych. 2018;9:786. https://doi.org/10.3389/fpsyt.2018.00786.
Daneshvari NO, Mojtabai R, Eaton WW, Cullen BA, Rodriguez KM, Spivak S. Symptom severity and care delay among patients with serious mental illness. J Health Care Poor Underserved. 2021;32(3):1312–9. https://doi.org/10.1353/hpu.2021.0134.
Mojtabai R, Cullen B, Everett A, et al. Reasons for not seeking general medical care among individuals with serious mental illness. Psychiatr Serv. 2014;65(6):818–21. https://doi.org/10.1176/appi.ps.201300348.
McGinty EE, Stone EM, Daumit GL. Serious mental illness in primary care: a national physician survey. J Gen Intern Med. 2021;36(3):833–5. https://doi.org/10.1007/s11606-020-05950-8.
Vanderlip ER, Raney LE, Druss BG. A framework for extending psychiatrists’ roles in treating general health conditions. Am J Psychiatry. 2016;173(7):658–63. https://doi.org/10.1176/appi.ajp.2015.15070950.
Parameswaran SG, Chang C, Swenson AK, Shumway M, Olfson M, Mangurian CV. Roles in and barriers to metabolic screening for people taking antipsychotic medications: a survey of psychiatrists. Schizophr Res. 2013;143(2–3):395–6. https://doi.org/10.1016/j.schres.2012.08.031.
Mangurian C, Modlin C, Williams L, et al. A doctor is in the house: stakeholder focus groups about expanded scope of practice of community psychiatrists. Community Ment Health J. 2018;54(5):507–13. https://doi.org/10.1007/s10597-017-0198-4.
Corrigan PW, Mittal D, Reaves CM, et al. Mental health stigma and primary health care decisions. Psychiatry Res. 2014;218(1–2):35–8. https://doi.org/10.1016/j.psychres.2014.04.028.
Sullivan G, Mittal D, Reaves CM, et al. Influence of schizophrenia diagnosis on providers’ practice decisions. J Clin Psychiatry. 2015;76(8):1068–74; quiz 1074. https://doi.org/10.4088/JCP.14m09465.
Stone EM, Chen LN, Daumit GL, Linden S, McGinty EE. General medical clinicians’ attitudes toward people with serious mental illness: a scoping review. J Behav Health Serv Res. 2019;46(4):656–79. https://doi.org/10.1007/s11414-019-09652-w.
Murphy KA, Stone EM, Presskreischer R, McGinty EE, Daumit GL, Pollack CE. Cancer screening among adults with and without serious mental illness: a mixed methods study. Med Care. 2021;59(4):327–33. https://doi.org/10.1097/mlr.0000000000001499.
Lester H, Tritter JQ, Sorohan H. Patients’ and health professionals’ views on primary care for people with serious mental illness: focus group study. BMJ (Clinical Research ed). 2005;330(7500):1122. https://doi.org/10.1136/bmj.38440.418426.8F.
Mangurian C, Niu GC, Schillinger D, Newcomer JW, Dilley J, Handley MA. Utilization of the behavior change wheel framework to develop a model to improve cardiometabolic screening for people with severe mental illness. Implement Sci : IS. 2017;12(1):134. https://doi.org/10.1186/s13012-017-0663-z.
Berren MR, Santiago JM, Zent MR, Carbone CP. Health care utilization by persons with severe and persistent mental illness. Psychiatr Serv. 1999;50(4):559–61. https://doi.org/10.1176/ps.50.4.559.
Copeland LA, Zeber JE, Wang CP, et al. Patterns of primary care and mortality among patients with schizophrenia or diabetes: a cluster analysis approach to the retrospective study of healthcare utilization. BMC Health Serv Res. 2009;9:127. https://doi.org/10.1186/1472-6963-9-127.
Vistorte AOR, Ribeiro WS, Jaen D, Jorge MR, Evans-Lacko S, Mari JJ. Stigmatizing attitudes of primary care professionals towards people with mental disorders: a systematic review. Int J Psychiatry Med. 2018;53(4):317–38. https://doi.org/10.1177/0091217418778620.
Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504–10. https://doi.org/10.1007/s11606-013-2441-1.
Valery KM, Prouteau A. Schizophrenia stigma in mental health professionals and associated factors: a systematic review. Psychiatry Res. 2020;290:113068. https://doi.org/10.1016/j.psychres.2020.113068.
Dehon E, Weiss N, Jones J, Faulconer W, Hinton E, Sterling S. A systematic review of the impact of physician implicit racial bias on clinical decision making. Acad Emerg Med Off J Soc Acad Emerg Med. 2017;24(8):895–904. https://doi.org/10.1111/acem.13214.
Zomer E, Osborn D, Nazareth I, et al. Effectiveness and cost-effectiveness of a cardiovascular risk prediction algorithm for people with severe mental illness (PRIMROSE). BMJ Open. 2017;7(9):e018181. https://doi.org/10.1136/bmjopen-2017-018181.
Horvitz-Lennon M, Kilbourne AM, Pincus HA. From silos to bridges: meeting the general health care needs of adults with severe mental illnesses. Health Aff (Project Hope). 2006;25(3):659–69. https://doi.org/10.1377/hlthaff.25.3.659.
Care Coordination Measures Atlas Update. Content last reviewed June 2014. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/ncepcr/care/coordination/atlas.html.
National Alliance on Mental Illness. Mental Health by the Numbers. 2022. https://nami.org/mhstats. Accessed 30 Oct 2022.
Świtaj P, Anczewska M, Chrostek A, et al. Disability and schizophrenia: a systematic review of experienced psychosocial difficulties. BMC Psychiatry. 2012;12:193. https://doi.org/10.1186/1471-244x-12-193.
Khaykin E, Eaton WW, Ford DE, Anthony CB, Daumit GL. Health insurance coverage among persons with schizophrenia in the United States. Psychiatr Serv. 2010;61(8):830–4. https://doi.org/10.1176/ps.2010.61.8.830.
Pesa J, Rotter D, Papademetriou E, Potluri R, Patel C, Benson C. Real-world analysis of insurance churn among young adults with schizophrenia using the Colorado All-Payer Claims Database. J Manag Care Spec Pharm. 2022;28(1):26–38. https://doi.org/10.18553/jmcp.2022.28.1.26.
Toulany A, Stukel TA, Kurdyak P, Fu L, Guttmann A. Association of primary care continuity with outcomes following transition to adult care for adolescents with severe mental illness. JAMA Netw Open. 2019;2(8):e198415. https://doi.org/10.1001/jamanetworkopen.2019.8415.
Bartlett J, Manderscheid R. What does mental health parity really mean for the care of people with serious mental illness? Psychiatr Clin North Am. 2016;39(2):331–42. https://doi.org/10.1016/j.psc.2016.01.010.
Druss BG, Von Esenwein SA, Glick GE, et al. Randomized trial of an integrated behavioral health home: the Health Outcomes Management and Evaluation (HOME) Study. Am J Psychiatry. 2017;174(3):246–55. https://doi.org/10.1176/appi.ajp.2016.16050507.
Mangurian C, Thomas MD, Mitsuishi F, et al. Lessons learned from a new reverse-integration model to improve primary care screening in community mental health settings. Psychiatr Serv. 2022;73(8):942–5. https://doi.org/10.1176/appi.ps.202100177.
Scharf DM, Eberhart NK, Hackbarth NS, et al. Evaluation of the SAMHSA Primary and Behavioral Health Care Integration (PBHCI) grant program: final report. Rand Health Q. 2014;4(3):6.
Druss BG, Rohrbaugh RM, Levinson CM, Rosenheck RA. Integrated medical care for patients with serious psychiatric illness: a randomized trial. Arch Gen Psychiatry. 2001;58(9):861–8.
Bao Y, Casalino LP, Pincus HA. Behavioral health and health care reform models: patient-centered medical home, health home, and accountable care organization. J Behav Health Serv Res. 2013;40(1):121–32. https://doi.org/10.1007/s11414-012-9306-y.
McGinty EE, Presskreischer R, Breslau J, et al. Improving physical health among people with serious mental illness: the role of the specialty mental health sector. Psychiatr Serv. 2021;72(11):1301–10. https://doi.org/10.1176/appi.ps.202000768.
Vanderlip ER, Henwood BF, Hrouda DR, et al. Systematic literature review of general health care interventions within programs of assertive community treatment. Psychiatr Serv. 2017;68(3):218–24. https://doi.org/10.1176/appi.ps.201600100.
Druss BG, Goldman HH. Integrating Health and Mental Health Services: A Past and Future History. Am J Psychiatry. 2018;appiajp201818020169. https://doi.org/10.1176/appi.ajp.2018.18020169.
Brown JD. Availability of integrated primary care services in community mental health care settings. Psychiatr Serv. 2019;70(6):499–502. https://doi.org/10.1176/appi.ps.201800448.
Mangurian C, Giwa A, Brosey E, et al. Opinions of primary care clinicians and psychiatrists on monitoring the metabolic effects of antipsychotics. J Am Board Fam Med : JABFM. 2019;32(3):418–423. https://doi.org/10.3122/jabfm.2019.03.180176.
Daumit GL, Stone EM, Kennedy-Hendricks A, Choksy S, Marsteller JA, McGinty EE. Care coordination and population health management strategies and challenges in a behavioral health home model. Med Care. 2019;57(1):79–84. https://doi.org/10.1097/mlr.0000000000001023.
•• Daumit GL, Dalcin AT, Dickerson FB, et al. Effect of a comprehensive cardiovascular risk reduction intervention in persons with serious mental illness: a randomized clinical trial. JAMA Network Open. 2020;3(6):e207247–e207247. https://doi.org/10.1001/jamanetworkopen.2020.7247. Findings from this study suggest that comprehensive care coordination and care management can reduce CVD risk in a population with serious mental illness and at least one CVD risk factor.
Murphy KA, Dalcin A, McGinty EE, Goldsholl S, Heller A, Daumit GL. Applying care coordination principles to reduce cardiovascular disease risk factors in people with serious mental illness: a case study approach. Front Psychiatry. 2021;12:742169. https://doi.org/10.3389/fpsyt.2021.742169.
Samal L, Dykes PC, Greenberg JO, et al. Care coordination gaps due to lack of interoperability in the United States: a qualitative study and literature review. BMC Health Serv Res. 2016;16:143. https://doi.org/10.1186/s12913-016-1373-y.
McGinty EE, Murphy KA, Dalcin AT, et al. A model for advancing scale-up of complex interventions for vulnerable populations: the ALACRITY Center for Health and Longevity in Mental Illness. J Gen Intern Med. 2020. https://doi.org/10.1007/s11606-020-06137-x.
Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611–20. https://doi.org/10.1056/NEJMoa1003955.
Miller CJ, Grogan-Kaylor A, Perron BE, Kilbourne AM, Woltmann E, Bauer MS. Collaborative chronic care models for mental health conditions: cumulative meta-analysis and metaregression to guide future research and implementation. Med Care. 2013;51(10):922–30. https://doi.org/10.1097/MLR.0b013e3182a3e4c4.
Woltmann E, Grogan-Kaylor A, Perron B, Georges H, Kilbourne AM, Bauer MS. Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: systematic review and meta-analysis. Am J Psychiatry. 2012;169(8):790–804. https://doi.org/10.1176/appi.ajp.2012.11111616.
Bartels SJ, DiMilia PR, Fortuna KL, Naslund JA. Integrated care for older adults with serious mental illness and medical comorbidity: evidence-based models and future research directions. Psychiatr Clin North Am. 2018;41(1):153–64. https://doi.org/10.1016/j.psc.2017.10.012.
Chwastiak LA, Luongo M, Russo J, et al. Use of a Mental Health Center Collaborative Care Team to improve diabetes care and outcomes for patients with psychosis. Psychiatr Serv. 2018;69(3):349–52. https://doi.org/10.1176/appi.ps.201700153.
Baker E, Gwernan-Jones R, Britten N, et al. Refining a model of collaborative care for people with a diagnosis of bipolar, schizophrenia or other psychoses in England: a qualitative formative evaluation. BMC Psychiatry. 2019;19(1):7. https://doi.org/10.1186/s12888-018-1997-z.
Figueroa JF, Phelan J, Orav EJ, Patel V, Jha AK. Association of mental health disorders with health care spending in the Medicare population. JAMA Netw Open. 2020;3(3):e201210–e201210. https://doi.org/10.1001/jamanetworkopen.2020.1210.
Njie GJ, Proia KK, Thota AB, et al. Clinical decision support systems and prevention: a community guide cardiovascular disease systematic review. Am J Prev Med. 2015;49(5):784–95. https://doi.org/10.1016/j.amepre.2015.04.006.
•• Rossom RC, Crain AL, O’Connor PJ, et al. Effect of clinical decision support on cardiovascular risk among adults with bipolar disorder, schizoaffective disorder, or schizophrenia: a cluster randomized clinical trial. JAMA Netw Open. 2022;5(3):e220202. https://doi.org/10.1001/jamanetworkopen.2022.0202. Findings from this study suggest that a population health approach using clinical decision support system can improve management of cardiovascular risk factors for populations with serious mental illness.
Cohen S, Bostwick JR, Marshall VD, Kruse K, Dalack GW, Patel P. The effect of a computerized best practice alert system in an outpatient setting on metabolic monitoring in patients on second-generation antipsychotics. J Clin Pharm Ther. 2020;45(6):1398–404. https://doi.org/10.1111/jcpt.13236.
DelMonte MT, Bostwick JR, Bess JD, Dalack GW. Evaluation of a computer-based intervention to enhance metabolic monitoring in psychiatry inpatients treated with second-generation antipsychotics. J Clin Pharm Ther. 2012;37(6):668–73. https://doi.org/10.1111/j.1365-2710.2012.01369.x.
Van Dort BA, Zheng WY, Sundar V, Baysari MT. Optimizing clinical decision support alerts in electronic medical records: a systematic review of reported strategies adopted by hospitals. J Am Med Inform Assoc. 2021;28(1):177–83. https://doi.org/10.1093/jamia/ocaa279.
Daumit GL, Dickerson FB, Wang NY, et al. A behavioral weight-loss intervention in persons with serious mental illness. N Engl J Med. 2013;368(17):1594–602. https://doi.org/10.1056/NEJMoa1214530.
McGinty EE, Gudzune KA, Dalcin A, et al. Bringing an effective behavioral weight loss intervention for people with serious mental illness to scale. Front Psych. 2018;9:604. https://doi.org/10.3389/fpsyt.2018.00604.
McGinty E, Thompson D, Murphy KA, et al. Adapting the Comprehensive Unit Safety Program (CUSP) implementation strategy to increase delivery of evidence-based cardiovascular risk factor care in community mental health organizations: protocol for a pilot study. Implement Sci Commun. 2021;2(1):26. https://doi.org/10.1186/s43058-021-00129-6.
Swanson AJ, Pantalon MV, Cohen KR. Motivational interviewing and treatment adherence among psychiatric and dually diagnosed patients. J Nerv Ment Dis. 1999;187(10):630–5. https://doi.org/10.1097/00005053-199910000-00007.
Blixen C, Perzynski A, Kanuch S, et al. Training peer educators to promote self-management skills in people with serious mental illness (SMI) and diabetes (DM) in a primary health care setting. Prim Health Care Res Dev. 2015;16(2):127–37. https://doi.org/10.1017/s1463423614000176.
Druss BG, Singh M, Von Esenwein SA, et al. Peer-led self-management of general medical conditions for patients with serious mental illnesses: a randomized trial. Psychiatr Serv. 2018;69(5):529–35. https://doi.org/10.1176/appi.ps.201700352.
Aschbrenner KA, Brunette MF. The role of peers in health interventions for serious mental illness. Psychiatr Serv. 2018;69(5):497. https://doi.org/10.1176/appi.ps.69501.
McBain H, Mulligan K, Haddad M, Flood C, Jones J, Simpson A. Self management interventions for type 2 diabetes in adult people with severe mental illness. Cochrane Database of Syst Rev. 2016;4:Cd011361. https://doi.org/10.1002/14651858.CD011361.pub2.
Coxon A, McBain H, Pavlova N, Rowlands H, Mulligan K. Are diabetes self-management programmes for the general diabetes population effective for people with severe mental illness?: a systematic review. BMC Psychiatry. 2020;20(1):386. https://doi.org/10.1186/s12888-020-02779-7.
Jorm AF. Effect of contact-based interventions on stigma and discrimination: a critical examination of the evidence. Psychiatr Serv. 2020;71(7):735–7. https://doi.org/10.1176/appi.ps.201900587.
Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rüsch N. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatr Serv. 2012;63(10):963–73. https://doi.org/10.1176/appi.ps.201100529.
Kohrt BA, Jordans MJD, Turner EL, et al. Collaboration with people with lived experience of mental illness to reduce stigma and improve primary care services: a pilot cluster randomized clinical trial. JAMA Netw Open. 2021;4(11):e2131475. https://doi.org/10.1001/jamanetworkopen.2021.31475.
Rai S, Gurung D, Kaiser BN, et al. A service user co-facilitated intervention to reduce mental illness stigma among primary healthcare workers: utilizing perspectives of family members and caregivers. Fam Syst Health. 2018;36(2):198–209. https://doi.org/10.1037/fsh0000338.
Amsalem D, Valeri L, Jankowski SE, et al. Reducing public stigma toward individuals with psychosis across race and gender: a randomized controlled trial of young adults. Schizophr Res. 2022;243:195–202. https://doi.org/10.1016/j.schres.2022.03.011.
Rodríguez-Rivas ME, Cangas AJ, Cariola LA, Varela JJ, Valdebenito S. Innovative technology-based interventions to reduce stigma toward people with mental illness: systematic review and meta-analysis. JMIR Serious Games. 2022;10(2):e35099. https://doi.org/10.2196/35099.
Daumit GL, McGinty EE, Pronovost P, et al. Patient safety events and harms during medical and surgical hospitalizations for persons with serious mental illness. Psychiatr Serv. 2016;67(10):1068–75. https://doi.org/10.1176/appi.ps.201500415.
Funding
Gail L. Daumit reports grants from NIMH (P50 MH115842) and NHLBI (UG3154280).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Psychological Aspects of Cardiovascular Diseases
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Murphy, K.A., Daumit, G.L. Establishing a Care Continuum for Cardiometabolic Conditions for Patients with Serious Mental Illness. Curr Cardiol Rep 25, 193–202 (2023). https://doi.org/10.1007/s11886-023-01848-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-023-01848-z