Abstract
Purpose of Review
This review aims to describe the latest advances in autonomic neuromodulation approaches to treating cardiac arrhythmias, with a focus on ventricular arrhythmias.
Recent Findings
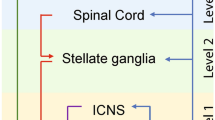
The increasing understanding of neuronal remodeling in cardiac diseases has led to the development and improvement of novel neuromodulation therapies targeting multiple levels of the autonomic nervous system. Thoracic epidural anesthesia, spinal cord stimulation, stellate ganglion modulatory therapies, vagal stimulation, renal denervation, and interventions on the intracardiac nervous system have all been studied in preclinical models, with encouraging preliminary clinical data.
Summary
The autonomic nervous system regulates all the electrical processes of the heart and plays an important role in the pathophysiology of cardiac arrhythmias. Despite recent advances in the clinical application of cardiac neuromodulation, our comprehension of the anatomy and function of the cardiac autonomic nervous system is still limited. Hopefully in the near future, more preclinical data combined with larger clinical trials will lead to further improvements in neuromodulatory treatment for heart rhythm disorders.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Armour JA, Murphy DA, Yuan BX, Mac Donald S, Hopkins DA. Gross and microscopic anatomy of the human intrinsic cardiac nervous system. Anat Rec. 1997;247:289–98.
Vincentz JW, Rubart M, Firulli AB. Ontogeny of cardiac sympathetic innervation and its implications for cardiac disease. Pediatr Cardiol. 2012;33:923–8. https://doi.org/10.1007/s00246-012-0248-1.
Ardell JL, Randall WC, Cannon WJ, Schmacht DC, Tasdemiroglu E. Differential sympathetic regulation of automatic, conductile, and contractile tissue in dog heart. Am J Phys. 1988;1988(255):H1050–9. https://doi.org/10.1152/ajpheart.1988.255.5.H1050.
Ajijola OA, Vaseghi M, ZhouW YK, Benharash P, Hadaya J, et al. Functional differences between junctional and extrajunctional adrenergic receptor activation in mammalian ventricle. Am J Physiol Heart Circ Physiol. 2013;304:H579–88. https://doi.org/10.1152/ajpheart.00754.2012.
Andresen MC, Kuntz DL, Mendelowitz D. In: Armour JA, Ardell JL, editors. Central nervous system regulation of the heart. New York: Oxford University Press; 2004. p. 187–219.
Hopkins DA, Andrew AJ. Ganglionic distribution of afferent neurons innervating the canine heart and cardiopulmonary nerves. J Auton Nerv Syst. 1989;26:213–22.
Armour JA. Potential clinical relevance of the “little brain” on the mammalian heart. Exp Physiol. 2008;93:165–76. https://doi.org/10.1113/expphysiol.2007.041178.
Pauza DH, Skripka V, Pauziene N, Stropus R. Morphology, distribution, and variability of the epicardiac neural ganglionated subplexuses in the human heart. Anat Rec. 2000;259:353–82.
Charpentier F, Drouin E, Gauthier C, LeMarec H. Early after/depolarizations and triggered activity: mechanisms and autonomic regulation. Fundam Clin Pharmacol. 1993;7:39–49.
Zipes DP, Barber MJ, Takahashi N, Gilmour RF Jr. Influence of the autonomic nervous system on the genesis of cardiac arrhythmias. Pacing Clin Electrophysiol. 1983;6:1210–20.
Ajijola OA, Lux RL, Khahera A, Kwon O, Aliotta E, Ennis DB, et al. Sympathetic modulation of electrical activation in normal and infarcted myocardium: implications for arrhythmogenesis. Am J Physiol Heart Circ Physiol. 2017;312:H608–21. https://doi.org/10.1152/ajpheart.00575.2016.
Shen MJ, Zipes DP. Role of the autonomic nervous system in modulating cardiac arrhythmias. Circ Res. 2014;114:1004–21. https://doi.org/10.1161/CIRCRESAHA.113.302549.
Yagishita D, Chui RW, Yamakawa K, Rajendran PS, Ajijola OA, Nakamura K, et al. Sympathetic nerve stimulation, not circulating norepinephrine, modulates T-peak to T-end interval by increasing global dispersion of repolarization. Circ Arrhythm Electrophysiol. 2015;8:174–85. https://doi.org/10.1161/CIRCEP.114.002195.
Vanhoutee PM, Verbeuren TJ. Inhibition by acetylcholine of the norepinephrine release evoked by potassium in canine saphenous veins. Circ Res. 1976;39:263–9.
Shanks J, Herring N. Peripheral cardiac sympathetic hyperactivity in cardiovascular disease: role of neuropeptides. Am J Physiol Regul Integr Comp Physiol 2013;305:R1411–20. https://doi.org/10.1152/ajpregu.00118.2013
Calvillo L, Vanoli E, Andreoli E, Besana A, Omodeo E, Gnecchi, et al. Vagal stimulation, through its nicotinic action, limits infarct size and the inflammatory response to myocardial ischemia and reperfusion. J Cardiovasc Pharmacol. 2011;58:500–7. https://doi.org/10.1097/FJC.0b013e31822b7204.
Floras JS. Sympathetic nervous system activation in human heart failure. Clinical implications of an updated model. J Am Coll Cardiol. 2009;54:375–85. https://doi.org/10.1016/j.jacc.2009.03.061.
Schwartz PJ, Pagani M, Lombardi F, Malliani A, Brown AM. A cardio-cardiac sympatho-vagal reflex in the cat. Circ Res. 1973;32:215–20.
Cerati D, Schwartz PJ. Single cardiac vagal fibers activity, acute myocardial ischemia, and risk for sudden death. Circ Res. 1991;69:1389–401.
Zahner MR, Li DP, Chen SR, Pan HL. Cardiac vanilloid receptor 1-expressing afferent nerves and their role in the cardiogenic sympathetic reflex in rats. J Physiol. 2003;2003(551):515–23. https://doi.org/10.1113/jphysiol.2003.048207.
Pan HL, Chen SR. Sensing tissue ischemia: another new function for capsaicin receptors? Circulation. 2004;110:1826–31. https://doi.org/10.1161/01.CIR.0000142618.20278.7A.
Uchida Y, Murao S. Bradykinin-induced excitation of afferent cardiac sympathetic nerve fibers. Jpn Heart J. 1974;15:84–91. https://doi.org/10.1536/ihj.15.84.
Schultz HD, Ustinova EE. Capsaicin receptors mediate free radical-induced activation of cardiac afferent endings. Cardiovasc Res. 1998;38:348–55. https://doi.org/10.1016/S0008-6363(98)00031-5.
Wang W, Schultz HD, Ma R. Cardiac sympathetic afferent sensitivity is enhanced in heart failure. Am J Physiol Heart Circ Physiol. 1999;277:H812–7.
Wang HJ, Wang W, Cornish KG, Rozanski GJ, Zucker IH. Cardiac sympathetic afferent denervation attenuates cardiac remodeling and improves cardiovascular dysfunction in rats with heart failure. Hypertension. 2014;64:745–55. https://doi.org/10.1161/HYPERTENSIONAHA.114.03699.
Cha YM, Redfield MM, Shah S, Shen WK, Fishbein MC, Chen PS. Effects of omapatrilat on cardiac nerve sprouting and structural remodeling in experimental congestive heart failure. Heart Rhythm. 2005;2:984–90. https://doi.org/10.1016/j.hrthm.2005.05.016.
Inoue H, Zipes DP. Results of sympathetic denervation in the canine heart: supersensitivity that may be arrhythmogenic. Circulation. 1987;75:877–87.
Inoue H, Zipes DP. Time course of denervation of efferent sympathetic and vagal nerves after occlusion of the coronary artery in the canine heart. Circ Res. 1988;62:1111–20.
Vaseghi M, Lux RL, Mahajan A, Shivkumar K. Sympathetic stimulation increases dispersion of repolarization in humans with myocardial infarc- tion. Am J Physiol Heart Circ Physiol. 2012;302:H1838–46. https://doi.org/10.1152/ajpheart.01106.2011.
Verma A, Marrouche NF, Schweikert RA, Saliba W, Wazni O, Cummings J, et al. Relationship between successful ablation sites and the scar border zone defined by substrate mapping for ventricular tachycardia post-myocardial infarction. J Cardiovasc Electrophysiol. 2005;16:465–71. https://doi.org/10.1046/j.1540-8167.2005.40443.x.
• Klein T, Abdulghani M, Smith M, Huang R, Asoglu R, Remo BF, et al. Three-Dimensional 123I-Meta-Iodobenzylguanidine Cardiac Innervation Maps to Assess Substrate and Successful Ablation Sites for Ventricular Tachycardia: Feasibility Study for a Novel Paradigm of Innervation Imaging. Circ Arrhythm Electrophysiol. 2015;8:583–91. https://doi.org/10.1161/CIRCEP.114.002105. First in humans study who demonstrated the possibility of using 123I-Meta-Iodobenzylguanidine to build three-dimensional innervation maps of the heart to guide VT ablation procedures.
Han S, Kobayashi K, Joung B, Piccirillo G, Maruyama M, Vinters HV, et al. Electroanatomic remodeling of the left stellate ganglion after myocardial infarction. J Am Coll Cardiol. 2012;59:954–61. https://doi.org/10.1016/j.jacc.2011.11.030.
Ajijola OA, Yagishita D, Reddy NK, Yamakawa K, Vaseghi M, Downs AM, et al. Remodeling of stellate ganglion neurons after spatially targeted myocardial infarction: neuropeptide and morphologic changes. Heart Rhythm. 2015;12:1027–35. https://doi.org/10.1016/j.hrthm.2015.01.045.
Ajijola OA, Wisco JJ, Lambert HW, Mahajan A, Stark E, Fishbein MC, et al. Extracardiac neural remodeling in humans with cardiomyopathy. Circ Arrhythm Electrophysiol. 2012;5:1010–116. https://doi.org/10.1161/CIRCEP.112.972836.
• Ajijola OA, Hoover DB, Simerly TM, Brown TC, Yanagawa J, Biniwale RM, et al. Inflammation, oxidative stress, and glial cell activation characterize stellate ganglia from humans with electrical storm. JCI Insight. 2017;2:e94715. https://doi.org/10.1172/jci.insight.94715. Detailed in vitro evaluation of the stellate ganglia from humans with structural heart disease and electrical storm showing neuronal remodeling.
Xiao L, Haack KK, Zucker IH. Angiotensin II regulates ACE and ACE2 in neurons through p38 mitogen-activated protein kinase and extracellular signal-regulated kinase 1/2 signaling. Am J Phys Cell Phys. 2013;304:C1073–9. https://doi.org/10.1152/ajpcell.00364.2012.
Zucker IH, Gao L. The regulation of sympathetic nerve activity by angiotensin II involves reactive oxygen species and MAPK. Circ Res. 2005;97:737–9. https://doi.org/10.1161/01.RES.0000188261.94569.1f.
Lambert GW, Kaye DM, Lefkovits J, Jennings GL, Turner AG, Cox HS, et al. Increased central nervous system monoamine neurotransmitter turnover and its association with sympathetic nervous activity in treated heart failure patients. Circulation. 1995;92:1813–8.
Rizzo S, Basso C, Troost D, Aronica E, Frigo AC, Driessen AH, et al. T-cell-mediated inflammatory activity in the stellate ganglia of patients with ion-channel disease and severe ventricular arrhythmias. Circ Arrhythm Electrophysiol. 2014;7:224–9. https://doi.org/10.1161/CIRCEP.113.001184.
Nador F, Beria G, De Ferrari GM, Stramba-Badiale M, Locati EH, Lotto A, et al. Unsuspected echocardiographic abnormality in the long QT syndrome: diagnostic, prognostic, and pathogenetic implications. Circulation. 1991;84:1530–42.
Haugaa KH, Amlie JP, Berge KE, Leren TP, Smiseth OA, Edvardsen T. Transmural differences in myocardial contraction in long-QT syndrome: mechanical consequences of ion channel dysfunction. Circulation. 2010;122:1355–63. https://doi.org/10.1161/CIRCULATIONAHA.110.960377.
Leren IS, Hasselberg NE, Saberniak J, Håland TF, Kongsgård E, Smiseth OA, et al. Cardiac mechanical alterations and genotype specific differences in subjects with long QT syndrome. J Am Coll Cardiol Img. 2015;8:501–10. https://doi.org/10.1016/j.jcmg.2014.12.023.
Haugaa KH, Edvardsen T, Leren TP, Gran JM, Smiseth OA, Amlie JP. Left ventricular mechanical dispersion by tissue Doppler imaging: a novel approach for identifying high-risk individuals with long QT syndrome. Eur Heart J. 2009;30:330–7. https://doi.org/10.1093/eurheartj/ehn466.
Hamon D, Rajendran PS, Chui RW, Ajijola OA, Irie T, Talebi R, et al. Premature ventricular contraction coupling interval variability destabilizes cardiac neuronal and electrophysiological control: insights from simultaneous cardioneural mapping. Circ Arrhythm Electrophysiol. 2017;10. https://doi.org/10.1161/CIRCEP.116.004937.
Tung R, Shivkumar K. Neuraxial modulation for treatment of VT storm. J Biomed Res. 2015;29:56–60. https://doi.org/10.7555/JBR.29.20140161.
Howard-Quijano K, Takamiya T, Dale EA, Kipke J, Kubo Y, Grogan T, et al. Spinal cord stimulation reduces ventricular arrhythmias during acute ischemia by attenuation of regional myocardial excitability. Am J Physiol Heart Circ Physiol. 2017;313:H421–31. https://doi.org/10.1152/ajpheart.00129.2017.
Bourke T, Vaseghi M, Michowitz Y, Sankhla V, Shah M, Swapna N, et al. Neuraxial modulation for refractory ventricular arrhythmias: value of thoracic epidural anesthesia and surgical left cardiac sympathetic denervation. Circulation. 2010;121:2255–62. https://doi.org/10.1161/CIRCULATIONAHA.109.929703.
Mannheimer C, Camici P, Chester MR, Collins A, DeJongste M, Eliasson T, et al. The problem of chronic refractory angina; report from the ESC Joint Study Group on the Treatment of Refractory Angina. Eur Heart J. 2002;23:355–70.
Zhang TC, Janik JJ, Grill WM. Mechanisms and models of spinal cord stimulation for the treatment of neuropathic pain. Brain Res. 2014;1569:19–31. https://doi.org/10.1016/j.brainres.2014.04.039.
Wang S, Zhou X, Huang B, Wang Z, Liao K, Saren G, et al. Spinal cord stimulation protects against ventricular arrhythmias by suppressing left stellate ganglion neural activity in an acute myocardial infarction canine model. Heart Rhythm. 2015;12:1628–35. https://doi.org/10.1016/j.hrthm.2015.03.023.
Odenstedt J, Linderoth B, Bergfeldt L, Ekre O, Grip L, Mannheimer C, et al. Spinal cord stimulation effects on myocardial ischemia, infarct size, ventricular arrhythmia, and noninvasive electrophysiology in a porcine ischemia–reperfusion model. Heart Rhythm. 2011;8:892–8. https://doi.org/10.1016/j.hrthm.2011.01.029.
Grimaldi R, de Luca A, Kornet L, Castagno D, Gaita F. Can spinal cord stimulation reduce ventricular arrhythmias? Heart Rhythm. 2012;9:1884–7. https://doi.org/10.1016/j.hrthm.2012.08.007.
Tse HF, Turner S, Sanders P, Okuyama Y, Fujiu K, Cheung CW, et al. Thoracic Spinal Cord Stimulation for Heart Failure as a Restorative Treatment (SCS HEART study): first-in-man experience. Heart Rhythm. 2015;12:588–95. https://doi.org/10.1111/j.1540-8167.2011.02230.x.
Zipes DP, Neuzil P, Theres H, Caraway D, Mann DL, Mannheimer C, et al. Determining the feasibility of spinal cord neuromodulation for the treatment of chronic systolic heart failure: the DEFEAT-HF study. JACC Heart Fail. 2016;4:129–36. https://doi.org/10.1016/j.jchf.2015.10.006.
Schwartz PJ, Stone HL, Brown AM. Effects of unilateral stellate ganglion blockade on the arrhythmias associated with coronary occlusion. Am. Heart J. 1976;92:589–99.
Schwartz PJ, Billman GE, Stone HL. Autonomic mechanisms in ventricular fibrillation induced by myocardial ischemia during exercise in dogs with healed myocardial infarction: an experimental preparation for sudden cardiac death. Circulation. 1984;69:790–800.
• Irie T, Yamakawa K, Hamon D, Nakamura K, Shivkumar K, Vaseghi M. Cardiac sympathetic innervation via middle cervical and stellate ganglia and antiarrhythmic mechanism of bilateral stellectomy. Am J Physiol Heart Circ Physiol. 2017;312:H392–405. https://doi.org/10.1152/ajpheart.00644.2016. First demonstration in a big animal model of the rule of middle cervical ganglia in regulating electrical properties of the heart and cardiovascular reflexes.
Schwartz PJ, Snebold NG, Brown AM. Effects of unilateral cardiac sympathetic denervation on the ventricular fibrillation threshold. Am J Cardiol. 1976;37:1034–40.
Schwartz PJ, Malliani A. Electrical alternation of the T wave: clinical and experimental evidence of its relationship with the sympathetic nervous system and with the long QT syndrome. Am. Heart J. 1975;89:45–50.
Cao JM, Chen LS, KenKnight BH, Ohara T, Lee MH, Tsai J, et al. Nerve sprouting and sudden cardiac death. Circ Res. 2000;86:816–21.
Schwartz PJ, De Ferrari GM, Pugliese L. Cardiac sympathetic denervation 100 years later: Jonnesco would have never believed it. Int J Cardiol. 2017;237:25–8. https://doi.org/10.1016/j.ijcard.2017.03.020.
Schwartz PJ, Priori SG, Cerrone M, Spazzolini C, Odero A, Napolitano C, et al. Left cardiac sympathetic denervation in the management of high-risk patients affected by the long QT syndrome. Circulation. 2004;109:1826–33. https://doi.org/10.1161/01.CIR.0000125523.14403.1E.
•• De Ferrari GM, Dusi V, Spazzolini C, Bos JM, Abrams DJ, Berul CI, et al. Clinical management of catecholaminergic polymorphic ventricular tachycardia: the role of left cardiac sympathetic denervation. Circulation. 2015;131:2185–93. https://doi.org/10.1161/CIRCULATIONAHA.115.015731. The largest human study showing the efficacy of LCSD in VAs in CVPT.
Odero A, Bozzani A, De Ferrari GM, Schwartz PJ. Left cardiac sympathetic denervation for the prevention of life-threatening arrhythmias: the surgical supraclavicular approach to cervicothoracic sympathectomy. Heart Rhythm. 2010;7:1161–5. https://doi.org/10.1016/j.hrthm.2010.03.046.
Collura CA, Johnson JN, Moir C, Ackerman MJ. Left cardiac sympathetic denervation for the treatment of long QT syndrome and catecholaminergic polymorphic ventricular tachycardia using video-assisted thoracic surgery. Heart Rhythm. 2009;6:752–9. https://doi.org/10.1016/j.hrthm.2009.03.024.
Kwon OJ, Pendekanti S, Fox JN, Yanagawa J, Fishbein MC, Shivkumar K, et al. Morphological spectra of adult human stellate ganglia: implications for thoracic sympathetic denervation. Anat Rec. 2018. https://doi.org/10.1002/ar.23797.
Zaidi ZF, Ashraf A. The nerve of Kunz: incidence, location and variations. J Appl Sci Res. 2010;6:659–64.
Waddell-Smith KE, Ertresvaag KN, Li J, Chaudhuri K, Crawford JR, Hamill JK, et al. Physical and psychological consequences of left cardiac sympathetic denervation in long-QT syndrome and catecholaminergic polymorphic ventricular tachycardia. Circ Arrhythm Electrophysiol. 2015;8:1151–8. https://doi.org/10.1161/CIRCEP.115.003159.
Coleman MA, Bos MJ, Johnson JN, Owen HJ, Deschamps C, Moir C, et al. Videoscopic left cardiac sympathetic denervation for patients with recurrent ventricular fibrillation/malignant ventricular arrhythmia syndromes besides congenital long-QT syndrome. Circ Arrhythm Electrophysiol. 2012;5:782–8. https://doi.org/10.1161/CIRCEP.112.971754.
Ajijola OA, Lellouche N, Bourke T, Tung R, Ahn S, Mahajan A, et al. Bilateral cardiac sympathetic denervation for the management of electrical storm. J Am Coll Cardiol. 2012;59:91–2. https://doi.org/10.1016/j.jacc.2011.09.043.
Vaseghi M, Gima J, Kanaan C, Ajijola OA, Marmureanu A, Mahajan A, et al. Cardiac sympathetic denervation in patients with refractory ven- tricular arrhythmias or electrical storm: intermediate and long-term follow-up. Heart Rhythm. 2014;11:360–6. https://doi.org/10.1016/j.hrthm.2013.11.028.
•• Vaseghi M, Barwad P, Malavassi Corrales FJ, Tandri H, Mathuria N, et al. Cardiac sympathetic denervation for refractory ventricular arrhythmias. J Am Coll Cardiol. 2017;69:3070–80. https://doi.org/10.1016/j.jacc.2017.04.035. The largest and most recent study showing that CSD decreased VAs in patients with structural heart disease.
Romero J, Di Biase L, Diaz JC, Quispe R, Du X, Briceno D, et al. Early versus late referral for catheter ablation of ventricular tachycardia in patients with structural heart disease. JACC. 2018;3:374–82. https://doi.org/10.1016/j.jacep.2017.12.008.
Leriche R, Fontaine R. L’Anesthe ́ sie isole ́ e du ganglion e ́ toile ́ . Sa technique, ses indications, ses re ́ sultats. Presse Med. 1934;42:849–50.
Gofeld M, Bhatia A, Abbas S, Ganapathy S, Johnson M. Development and validation of a new technique for ultrasound-guided stellate ganglion block. Reg Anesth Pain Med. 2009;34:475–9. https://doi.org/10.1097/AAP.0b013e3181b494de.
Hayase J, Vampola S, Ahadian F, Narayan SM, Krummen DE. Comparative efficacy of stellate ganglion block with bupivacaine vs pulsed radiofrequency in a patient with refractory ventricular arrhythmias. J Clin Anesth. 2016;31:162–5. https://doi.org/10.1016/j.jclinane.2016.01.026.
Meng L, Tseng CH, Shivkumar K, Ajijola O. Efficacy of stellate ganglion blockade in managing electrical storm: a systematic review. JACC Clin Electrophysiol. 2017;9:942–9. https://doi.org/10.1016/j.jacep.2017.06.006.
Kumar R, Woo MA, Birrer BV, Macey PM, Fonarow GC, Hamilton MA, et al. Mammillary bodies and fornix fibers are injured in heart failure. Neurobiol Dis. 2009;33:236–42. https://doi.org/10.1016/j.nbd.2008.10.004.
Woo MA, Palomares JA, Macey PM, Fonarow GC, Harper RM, Kumar R. Global and regional brain mean diffusivity changes in patients with heart failure. J Neurosci Res. 2015;93:678–85. https://doi.org/10.1002/jnr.23525.
Zuanetti G, De Ferrari GM, Priori SG, Schwartz PJ. Protective effect of vagal stimulation on reperfusion arrhythmias in cats. Circ Res. 1987;61:429–35.
Vanoli E, De Ferrari GM, Stramba-Badiale M, Hull SS Jr, Foreman RD, Schwartz PJ. Vagal stimulation and prevention of sudden death in conscious dogs with a healed myocardial infarction. Circ Res. 1991;68:1471–81.
Nazeri A, Elayda MA, Dragnev L, Frank CM, Qu J, Afonso VX, et al. Heterogeneity of left ventricular signal characteristics in response to acute vagal stimulation during ventricular fibrillation in dogs. Tex Heart Inst J. 2011;38:621–6.
Ardell JL, Rajendran PS, Nier HA, KenKnight BH, Armour JA. Central-peripheral neural network interactions evoked by vagus nerve stimulation: functional consequences on control of cardiac function. Am J Physiol Heart Circ Physiol. 2015;309:H1740–52. https://doi.org/10.1152/ajpheart.00557.2015.
Yoo PB, Lubock NB, Hincapie JG, Ruble SB, Hamann JJ, Grill WM. High-resolution measurement of electrically-evoked vagus nerve activity in the anesthetized dog. J Neural Eng. 2013;10:026003. https://doi.org/10.1088/1741-2560/10/2/026003.
• Yamaguchi N, Yamakawa K, Rajendran PS, Takamiya T, Vaseghi M. Antiarrhythmic effects of vagal nerve stimulation after cardiac sympathetic denervation in the setting of chronic myocardial infarction. Heart Rhythm. 2018;15:1214–22. https://doi.org/10.1016/j.hrthm.2018.03.012. First animal study showing the beneficial antiarrhythmic effects of VNS after CSD in the setting of chronic myocardial infarction.
Uthman BM, Reichl AM, Dean JC, Eisenschenk S, Gilmore R, Reid S, et al. Effectiveness of vagus nerve stimulation in epilepsy patients: a 12-year observation. Neurology. 2004;63:1124–6.
Shuchman M. Approving the vagus-nerve stimulator for depression. N Engl J Med. 2007;356:1604–7. https://doi.org/10.1056/NEJMp078035.
•• Shivkumar K, Ajijola OA, Anand I, Armour JA, Chen PS, Esler M, et al. Clinical neurocardiology defining the value of neuroscience-based cardiovascular therapeutics. J Physiol. 2016;594:3911–54. https://doi.org/10.1113/JP271870. First position paper by international experts in the field defining the rationale and the clinical impact of neuroscience-based cardiovascular therapeutics.
Yu L, Wang S, Zhou X, Wang Z, Huang B, Liao K, et al. Chronic intermittent low-level stimulation of tragus reduces cardiac autonomic remodeling and ventricular arrhythmia inducibility in a post-infarction canine model. JACC Clin Electrophysiol. 2016;2:330–9. https://doi.org/10.1016/j.jacep.2015.11.006.
• Yu L, Huang B, Po SS, Tan T, Wang M, Zhou L, et al. Low-Level tragus stimulation for the treatment of ischemia and reperfusion injury in patients with ST-segment elevation myocardial infarction: a proof-of-concept study. JACC Cardiovasc Interv. 2017;10:1511–20. https://doi.org/10.1016/j.jcin.2017.04.036. First in humans, randomized study showing the beneficial effect of low-level tragus stimulation for the treatment of ischemia and reperfusion injury.
Shen MJ, Shinohara T, Park HW, Frick K, Ice DS, Choi EK, et al. Continuous low-level vagus nerve stimulation reduces stellate ganglion nerve activity and paroxysmal atrial tachyarrhythmias in ambulatory canines. Circulation. 2011;123:2204–12. https://doi.org/10.1161/CIRCULATIONAHA.111.018028.
Katritsis DG, Pokushalov E, Romanov A, Giazitzoglou E, Siontis GC, Po SS, et al. Autonomic denervation added to pulmonary vein isolation for paroxysmal atrial fibrillation: a randomized clinical trial. JAmColl Cardiol. 2013;62:2318–25. https://doi.org/10.1016/j.jacc.2013.06.053.
• Driessen AH, Berger WR, Krul SP, Vanden Berg NW, Neefs J, Piersma FR, et al. Ganglion plexus ablation in advanced atrial fibrillation: the AFACT study. J Am Coll Cardiol. 2016;68:1155–65. https://doi.org/10.1016/j.jacc.2016.06.036 .The largest, randomized clinical trial of ganglion plexus ablation in advanced atrial fibrillation, with negative finding.
Pokushalov E, Kozlov B, Romanov A, Strelnikov A, Bayramova S, Sergeevichev D, et al. Long-term suppression of atrial fibrillation by botulinum toxin injection into epicardial fat pad in patients undergoing cardiac surgery: one-year follow-up of a randomized pilot study. Circ Arrhythm Electrophysiol. 2015;8:1334–41. https://doi.org/10.1161/CIRCEP.115.003199.
Lo LW, Scherlag BJ, Chang HY, Lin YJ, Chen SA, Po SS. Paradoxical long-term proarrhythmic effects after ablating the “head station” ganglionated plexi of the vagal innervation to the heart. Heart Rhythm. 2013;10:751–7. https://doi.org/10.1016/j.hrthm.2013.01.030.
He B, Lu Z, He W, Wu L, Cui B, Hu X, et al. Effects of ganglionated plexi ablation on ventricular electrophysiological properties in normal hearts and after acute myocardial ischemia. Int J Cardiol. 2013;168:86–93. https://doi.org/10.1016/j.ijcard.2012.09.067.
Vaseghi M, Lellouche N, Ritter H, Fonarow GC, Patel JK, Moriguchi J, et al. Mode and mechanisms of death after orthotopic heart transplantation. Heart Rhythm. 2009;6:503–9. https://doi.org/10.1016/j.hrthm.2009.01.005.
Vaseghi M, Boyle NG, Kedia R, Patel JK, Cesario DA, Wiener I, et al. Supraventricular tachycardia after orthotopic cardiac transplantation. J Am Coll Cardiol. 2008;51:2241–9. https://doi.org/10.1016/j.jacc.2008.02.065.
Jackson N, Gizurarson S, Azam MA, King B, Ramadeen A, Zamiri N, et al. Effects of renal artery denervation on ventricular arrhythmias in a postinfarct model. Circ Cardiovasc Interv. 2017;10:e004172. https://doi.org/10.1161/CIRCINTERVENTIONS.116.004172.
Armaganijan LV, Staico R, Moreira DA, Lopes RD, Medeiros PT, Habib R, et al. 6-month outcomes in patients with implantable cardioverter-defibrillators undergoing renal sympathetic denervation for the treatment of refractory ventricular arrhythmias. JACC Cardiovasc Interv. 2015;8:984–90. https://doi.org/10.1016/j.jcin.2015.03.012.
Evranos B, Canpolat U, Kocyigit D, Coteli C, Yorgun H, Aytemir K, et al. Role of adjuvant renal sympathetic denervation in the treatment of ventricular arrhythmias. Am J Cardiol. 2016;118:1207–10. https://doi.org/10.1016/j.amjcard.2016.07.036.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Veronica Dusi, Ching Zhu, and Olujimi A. Ajijola declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This is a review article so we have referenced studies done in humans and animals, but these studies were not done as part of this article, and they are just referenced here. For those studies, all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. And all applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Invasive Electrophysiology and Pacing
Rights and permissions
About this article
Cite this article
Dusi, V., Zhu, C. & Ajijola, O.A. Neuromodulation Approaches for Cardiac Arrhythmias: Recent Advances. Curr Cardiol Rep 21, 32 (2019). https://doi.org/10.1007/s11886-019-1120-1
Published:
DOI: https://doi.org/10.1007/s11886-019-1120-1