Abstract
Purpose of Review
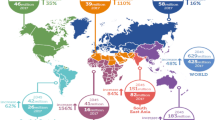
South Asia has around 1/6th of the current global population. Epidemiological studies suggest that South Asians living in South Asia and diaspora are at an increased risk of premature atherosclerotic cardiovascular diseases (ASCVDs). This is due to an interplay of genetic, acquired, and environmental risk factors. Due to its increasing share of the global population, clinicians need to know the reasons for this early predisposition, and strategies for early identification and mitigation.
Recent Findings
South Asians have earlier onset of cardiometabolic risk factors such as insulin resistance, hypertension, and central adiposity. This increased risk is seen in both native South Asians and the diaspora.
Summary
South Asians have earlier onset of ASCVD due to an earlier onset of cardiometabolic risk factors. Health promotion and early identification of these risk factors are essential to mitigate this ongoing crisis.


Similar content being viewed by others
Abbreviations
- apoA:
-
Apolipoprotein A
- apoB:
-
Apolipoprotein B
- ASCVD:
-
Atherosclerotic cardiovascular disease
- BMI:
-
Body mass index
- BRAVE:
-
Bangladesh Risk of Acute Vascular Event
- CAC:
-
Coronary artery calcium
- CAD:
-
Coronary artery disease
- CARRS:
-
Centre for Cardiometabolic Risk Reduction in South-Asia study
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CRP:
-
C-reactive protein
- CVD:
-
Cardiovascular disease
- DM:
-
Diabetes mellitus
- eGFR:
-
Estimated glomerular filtration rate
- GBD:
-
Global Burden of Diseases
- HDL-C:
-
High-density lipoprotein cholesterol
- HOMA:
-
Homeostasis model assessment of insulin resistance
- HR:
-
Hazard ratio
- IHD:
-
Ischemic heart disease
- INTERHEART:
-
Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries
- LDL-C:
-
Low-density lipoprotein cholesterol
- Lp(a):
-
Lipoprotein(a)
- MASALA:
-
Mediators of Atherosclerosis in South Asians Living in America
- MESA:
-
Multi-Ethnic Study of Atherosclerosis
- MI:
-
Myocardial infarction
- NCD:
-
Non-communicable disease
- NHANES:
-
National Health and Nutrition Examination Survey
- PA:
-
Physical activity
- RCT:
-
Randomized control trials
- SHARE:
-
Study of Health Assessment and Risk in Ethnic Groups
- TG:
-
Triglyceride
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Roser M, Ritchie H, Ortiz-Ospina E, Rodés-Guirao L. World population growth. Our World Data. Published online May 9, 2013. https://ourworldindata.org/world-population-growth. Accessed 1 Apr 2023.
Population growth (annual %) | Data. https://data.worldbank.org/indicator/SP.POP.GROW. Accessed 1 Apr 2023.
Budiman A, Ruiz NG. Key facts about Asian Americans, a diverse and growing population. Pew Research Center. https://www.pewresearch.org/fact-tank/2021/04/29/key-facts-about-asian-americans/. Accessed 1 Apr 2023
Vaduganathan M, Mensah GA, Turco JV, Fuster V, Roth GA. The global burden of cardiovascular diseases and risk. J Am Coll Cardiol. 2022;80(25):2361–71. https://doi.org/10.1016/j.jacc.2022.11.005.
Lindstrom M, DeCleene N, Dorsey H, et al. Global burden of cardiovascular diseases and risks collaboration, 1990–2021. J Am Coll Cardiol. 2022;80(25):2372–425. https://doi.org/10.1016/j.jacc.2022.11.001.
Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021. https://doi.org/10.1016/j.jacc.2020.11.010. ()
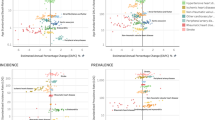
Patel AP, Wang M, Kartoun U, Ng K, Khera AV. Quantifying and understanding the higher risk of atherosclerotic cardiovascular disease among South Asian individuals. Circulation. 2021;144(6):410–22. https://doi.org/10.1161/CIRCULATIONAHA.120.052430. One the largest contemporary cohort studies comparing risk factors and ASCVD outcomes among South Asians and Europeans in the UK.
Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet Lond Engl. 2004;364(9438):937–52. https://doi.org/10.1016/S0140-6736(04)17018-9. One of the first large-scale epidemiological studies highlighting significantly lower age for first myocardial infarction among South Asians and underlying risk factors.
Sacco RL, Roth GA, Reddy KS, et al. The Heart of 25 by 25: Achieving the goal of reducing global and regional premature deaths from cardiovascular diseases and stroke: a modeling study from the American Heart Association and World Heart Federation. Circulation. 2016;133(23):e674-690. https://doi.org/10.1161/CIR.0000000000000395. Study projecting incidence of premature ASCVD globally and among regions.
Kianoush S, Rifai MA, Jain V, et al. Prevalence and predictors of premature coronary heart disease among Asians in the United States: a National Health Interview Survey study. Curr Probl Cardiol. 26 2022:101152. https://doi.org/10.1016/j.cpcardiol.2022.101152
Joseph P, Kutty VR, Mohan V, et al. Cardiovascular disease, mortality, and their associations with modifiable risk factors in a multi-national South Asia cohort: a PURE substudy. Eur Heart J. 2022;43(30):2831–40. https://doi.org/10.1093/eurheartj/ehac249. Epidemiological study comparing CV and all cause mortality rates across South Asian regions.
Gupta K, Al Rifai M, Hussain A, et al. South Asian ethnicity: what can we do to make this risk enhancer a risk equivalent? Prog Cardiovasc Dis. 2022;75:21–32. https://doi.org/10.1016/j.pcad.2022.10.001.
Volgman AS, Palaniappan LS, Aggarwal NT, et al. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American Heart Association. Circulation. 2018;138(1):e1–34. https://doi.org/10.1161/CIR.0000000000000580.
Mehta A, Vasquez N, Ayers CR, et al. Independent association of lipoprotein(a) and coronary artery calcification with atherosclerotic cardiovascular risk. J Am Coll Cardiol. 2022;79(8):757–68. https://doi.org/10.1016/j.jacc.2021.11.058.
Ahmed ST, Rehman H, Akeroyd JM, et al. Premature coronary heart disease in South Asians: burden and determinants. Curr Atheroscler Rep. 2018;20(1):6. https://doi.org/10.1007/s11883-018-0706-1.
Kanaya AM, Herrington D, Vittinghoff E, et al. Understanding the high prevalence of diabetes in U.S. South Asians compared with four racial/ethnic groups: the MASALA and MESA studies. Diabetes Care. 2014;37(6):1621–8. https://doi.org/10.2337/dc13-2656. ()
Yajnik CS, Lubree HG, Rege SS, et al. Adiposity and hyperinsulinemia in Indians are present at birth. J Clin Endocrinol Metab. 2002;87(12):5575–80. https://doi.org/10.1210/jc.2002-020434.O. One the earliest studies reporting higher insulin resistance and adiposity among South Asian newborns.
Ikehara S, Tabák AG, Akbaraly TN, et al. Age trajectories of glycaemic traits in non-diabetic South Asian and white individuals: the Whitehall II cohort study. Diabetologia. 2015;58(3):534–42. https://doi.org/10.1007/s00125-014-3448-9.
Jainandunsing S, Özcan B, Rietveld T, et al. Failing beta-cell adaptation in South Asian families with a high risk of type 2 diabetes. Acta Diabetol. 2015;52(1):11–9. https://doi.org/10.1007/s00592-014-0588-9.
Whincup PH, Nightingale CM, Owen CG, et al. Early emergence of ethnic differences in type 2 diabetes precursors in the UK: the Child Heart and Health Study in England (CHASE Study). PLOS Med. 2010;7(4):1000263. https://doi.org/10.1371/journal.pmed.1000263.
Wolf RM, Nagpal M, Magge SN. Diabetes and cardiometabolic risk in South Asian Youth: a review. Pediatr Diabetes. 2021;22(1):52–66. https://doi.org/10.1111/pedi.13078.
Pu J, Zhao B, Wang EJ, et al. Racial/ethnic differences in gestational diabetes prevalence and contribution of common risk factors. Paediatr Perinat Epidemiol. 2015;29(5):436–43. https://doi.org/10.1111/ppe.12209.
Lawlor DA, West J, Fairley L, et al. Pregnancy glycaemia and cord-blood levels of insulin and leptin in Pakistani and white British mother–offspring pairs: findings from a prospective pregnancy cohort. Diabetologia. 2014;57(12):2492–500. https://doi.org/10.1007/s00125-014-3386-6.
Clapp JF, Kiess W. Cord blood leptin reflects fetal fat mass. J Soc Gynecol Investig. 1998;5(6):300–3. https://doi.org/10.1177/107155769800500604.
Mantzoros CS, Rifas-Shiman SL, Williams CJ, Fargnoli JL, Kelesidis T, Gillman MW. Cord blood leptin and adiponectin as predictors of adiposity in children at 3 years of age: a prospective cohort study. Pediatrics. 2009;123(2):682–9. https://doi.org/10.1542/peds.2008-0343.
Bilen O, Kamal A, Virani SS. Lipoprotein abnormalities in South Asians and its association with cardiovascular disease: Current state and future directions. World J Cardiol. 2016;8(3):247–57. https://doi.org/10.4330/wjc.v8.i3.247. Review article discussing lipid abnormalities among South Asians.
Karthikeyan G, Teo KK, Islam S, et al. Lipid profile, plasma apolipoproteins, and risk of a first myocardial infarction among Asians: an analysis from the INTERHEART Study. J Am Coll Cardiol. 2009;53(3):244–53. https://doi.org/10.1016/j.jacc.2008.09.041. Study reporting higher apolipoprotein B concentration for similar level of LDL-C among South Asians.
Singh K, Thanassoulis G, Dufresne L, et al. A comparison of lipids and apoB in Asian Indians and Americans. Glob Heart. 2021;16(1):7. https://doi.org/10.5334/gh.882.
Patel JV, Caslake MJ, Vyas A, et al. Triglycerides and small dense low density lipoprotein in the discrimination of coronary heart disease risk in South Asian populations. Atherosclerosis. 2010;209(2):579–84. https://doi.org/10.1016/j.atherosclerosis.2009.10.010.
Virani SS, Koschinsky ML, Maher L, et al. Global think tank on the clinical considerations and management of lipoprotein(a): the top questions and answers regarding what clinicians need to know. Prog Cardiovasc Dis. 2022;73:32–40. https://doi.org/10.1016/j.pcad.2022.01.002.
Emerging Risk Factors Collaboration, Erqou S, Kaptoge S, et al. Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA. 2009;302(4):412-423https://doi.org/10.1001/jama.2009.1063
Paré G, Çaku A, McQueen M, et al. Lipoprotein(a) levels and the risk of myocardial infarction among 7 ethnic groups. Circulation. 2019;139(12):1472–82. https://doi.org/10.1161/CIRCULATIONAHA.118.034311. Study comparing lipoprotein(a) concentration across race/ethnicity.
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2019;140(11):e596–646. https://doi.org/10.1161/CIR.0000000000000678. ACC/AHA guidelines discussing the risk enhancer role of South Asians among those with borderline-intermediate 10-year ASCVD risk.
Narayan KMV, Kanaya AM. Why are South Asians prone to type 2 diabetes? A hypothesis based on underexplored pathways. Diabetologia. 2020;63(6):1103–9. https://doi.org/10.1007/s00125-020-05132-5.
Selvaraj S, Martinez EE, Aguilar FG, et al. Association of central adiposity with adverse cardiac mechanics. Circ Cardiovasc Imaging. 2016;9(6):e004396. https://doi.org/10.1161/CIRCIMAGING.115.004396.
InterAct Consortium, Langenberg C, Sharp SJ, et al. Long-term risk of incident type 2 diabetes and measures of overall and regional obesity: the EPIC-InterAct case-cohort study. PLoS Med. 2012;9(6):e1001230. https://doi.org/10.1371/journal.pmed.1001230
Ellulu MS, Patimah I, Khaza’ai H, Rahmat A, Abed Y. Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci AMS. 2017;13(4):851–63. https://doi.org/10.5114/aoms.2016.58928.
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71(6):e13–115. https://doi.org/10.1161/HYP.0000000000000065.
Gupta K, Jain V, Qamar A, et al. Regional impact of updated guidelines on prevalence and distribution of blood pressure categories for hypertension in India: Results from the National Family Health Survey 4. Indian Heart J. 2021;73(4):481–6. https://doi.org/10.1016/j.ihj.2021.06.004. Study reporting updated prevalence of hypertension in India.
Kibria GMA, Swasey K, Kc A, et al. Estimated Change in Prevalence of Hypertension in Nepal Following Application of the 2017 ACC/AHA Guideline. JAMA Netw Open. 2018;1(3):e180606. https://doi.org/10.1001/jamanetworkopen.2018.0606
Jafar TH, Islam M, Poulter N, et al. Children in South Asia have higher body mass–adjusted blood pressure levels than white children in the United States: a comparative study. Circulation. 2005;111(10):1291–7. https://doi.org/10.1161/01.CIR.0000157699.87728.F1.
Vasudevan A, Thomas T, Kurpad A, Sachdev HS. Prevalence of and factors associated with high blood pressure among adolescents in India. JAMA Netw Open. 2022;5(10):e2239282. https://doi.org/10.1001/jamanetworkopen.2022.39282.
Mehta A, Singh S, Saeed A, et al. Pathophysiological mechanisms underlying excess risk for diabetes and cardiovascular disease in South Asians: the perfect storm. Curr Diabetes Rev. 2021;17(9):070320183447. https://doi.org/10.2174/1573399816666200703182458.
Gupta K, Modi S, Ananthasubramaniam K. Toward understanding cardiovascular risk burden in South Asians. JACC Asia. 2022;2(7):912–5. https://doi.org/10.1016/j.jacasi.2022.10.005.
Rajagopalan S, Landrigan PJ. Pollution and the heart. N Engl J Med. 2021;385(20):1881–92. https://doi.org/10.1056/NEJMra2030281.
Gupta K, Ananthasubramaniam K. If you don’t kill pollution it could kill you: pathophysiologic insights into pollution mediated cardiovascular risk through FDG PET imaging. J Nucl Cardiol. Published online July 20, 2022. https://doi.org/10.1007/s12350-022-03022-4
Brook RD, Motairek I, Rajagopalan S, Al-Kindi S. Excess global blood pressure associated with fine particulate matter air pollution levels exceeding World Health Organization guidelines. J Am Heart Assoc. 2023;12(8):029206. https://doi.org/10.1161/JAHA.122.029206.
Castañeda H, Holmes SM, Madrigal DS, Young MED, Beyeler N, Quesada J. Immigration as a social determinant of health. Annu Rev Public Health. 2015;36(1):375–92. https://doi.org/10.1146/annurev-publhealth-032013-182419.
Holmboe-Ottesen G, Wandel M. Changes in dietary habits after migration and consequences for health: a focus on South Asians in Europe. Food Nutr Res. Published online November 6, 2012. https://doi.org/10.3402/fnr.v56i0.18891
Shah NS, Xi K, Kapphahn KI, et al. Cardiovascular and cerebrovascular disease mortality in Asian American subgroups. Circ Cardiovasc Qual Outcomes. 2022;15(5):e008651. https://doi.org/10.1161/CIRCOUTCOMES.121.008651. ()
Anand SS, Yusuf S, Vuksan V, et al. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE). Lancet Lond Engl. 2000;356(9226):279–84. https://doi.org/10.1016/s0140-6736(00)02502-2.
Kianoush S, Al Rifai M, Merchant AT, et al. Heterogeneity in the prevalence of premature hypertension among Asian American populations compared with white individuals: a National Health Interview Survey study. Int J Cardiol Cardiovasc Risk Prev. 2022;14:200147. https://doi.org/10.1016/j.ijcrp.2022.200147.
Kanaya AM, Herrington D, Vittinghoff E, et al. Understanding the high prevalence of diabetes in U.S. south Asians compared with four racial/ethnic groups: the MASALA and MESA studies. Diabetes Care. 2014;37(6):1621–8. https://doi.org/10.2337/dc13-2656. Study comparing prevalence of insulin resistance and diabetes among South Asians and other race/ethnicities in 2 of the largest cohort studies in the US.
Gujral UP, Narayan KMV, Pradeepa RG, et al. Comparing type 2 diabetes, prediabetes, and their associated risk factors in Asian Indians in India and in the U.S.: the CARRS and MASALA studies. Diabetes Care. 2015;38(7):1312–8. https://doi.org/10.2337/dc15-0032.
Al Rifai M, Kianoush S, Jain V, et al. Healthcare access among individuals of Asian descent in the U.S. Kans J Med. 2022;15:352–7. https://doi.org/10.17161/kjm.vol15.17942.
Implementation roadmap for accelerating the prevention and control of noncommunicable diseases in South-East Asia 2022–2030. https://www.who.int/publications-detail-redirect/9789290210054. Accessed 5 Apr 2023.
Multi-sectoral action plan for prevention and control of non-communicable diseases 2018–2025. Published online 2018. https://www.who.int/docs/default-source/searo/ncd/ban-ncd-action-plan-2018-2025.pdf?sfvrsn. Accessed 5 Apr 2023
WHO package of essential noncommunicable (PEN) disease interventions for primary health care. Published online 2020.
Bhutan making its people healthier, happier by beating noncommunicable diseases. https://www.who.int/news-room/feature-stories/detail/bhutan-making-its-people-healthier-happier-by-beating-noncommunicable-diseases. Accessed 5 Apr 2023
National Programme for prevention & Control of Cancer, Diabetes, Cardiovascular Diseases & stroke (NPCDCS) :: National Health Mission. https://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=1048&lid=604. Accessed 5 Apr 2023
Kumar AMV, Satyanarayana S, Wilson NC, et al. Operational research leading to rapid national policy change: tuberculosis-diabetes collaboration in India. Public Health Action. 2014;4(2):85–8. https://doi.org/10.5588/pha.14.0012.
Multi-sectoral Action Plan for the Prevention and Control of Noncommunicable Diseases In Maldives (2016–2020). https://extranet.who.int/nutrition/gina/sites/default/filesstore/MDV_2015_Multi-sectoral%20Action%20Plan%20For%20The%20Prevention%20And%20Control%20of%20Noncommunicable%20Diseases%20in%20Maldives%20%282016-2020%29_1.pdf. Accessed 5 Apr 2023
The Nepal NCDI Poverty Commission: An equity initiative to address noncommunicable diseases and injuries national report – 2018. Published online 2018. https://static1.squarespace.com/static/55d4de6de4b011a1673a40a6/t/5abe85111ae6cfa98183e7a9/1522435346791/Nepal+NCDI+Poverty+Commission+National+Report+2018.pdf. Accessed 5 Apr 2023
Shams P, Hussain M, Karani S, et al. Can sound public health policies stem the tide of burgeoning epidemic of cardiovascular disease in South Asians? Curr Cardiol Rep. 2021;23(12):181. https://doi.org/10.1007/s11886-021-01612-1.
National Guildline for Cardiovascular Risk Management for Primary Health care (Total Cardiovascular Risk Assessment Approach) Providers. Published online 2022. https://www.ncd.health.gov.lk/index.php?option=com_content&view=article&id=14&Itemid=142&lang=en. Accessed 5 Apr 2023
Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–337. https://doi.org/10.1093/eurheartj/ehab484.
ElSayed NA, Aleppo G, Aroda VR, et al. 2 Classification and diagnosis of diabetes: standards of care in diabetes. Diabetes Care. 2022;46(1):S19–40. https://doi.org/10.2337/dc23-S002.
Bukhsh A, Khan TM, Phisalprapa P, et al. Impact of pharmacist-led diabetes self-care education on patients with type 2 diabetes in Pakistan: a randomized controlled trial. Front Pharmacol. 2022;13:754999. https://doi.org/10.3389/fphar.2022.754999.
Tandon N, Gupta Y, Kapoor D, et al. Effects of a lifestyle intervention to prevent deterioration in glycemic status among South Asian women with recent gestational diabetes: a randomized clinical trial. JAMA Netw Open. 2022;5(3):e220773. https://doi.org/10.1001/jamanetworkopen.2022.0773.
Yu J, Thout SR, Li Q, et al. Effects of a reduced-sodium added-potassium salt substitute on blood pressure in rural Indian hypertensive patients: a randomized, double-blind, controlled trial. Am J Clin Nutr. 2021;114(1):185–93. https://doi.org/10.1093/ajcn/nqab054.
Ranasinghe C, Devage S, Constantine GR, Katulanda P, Hills AP, King NA. Glycemic and cardiometabolic effects of exercise in South Asian Sri Lankans with type 2 diabetes mellitus: A randomized controlled trial Sri Lanka diabetes aerobic and resistance training study (SL-DARTS). Diabetes Metab Syndr. 2021;15(1):77–85. https://doi.org/10.1016/j.dsx.2020.12.011.
Ali MK, Chwastiak L, Poongothai S, et al. Effect of a collaborative care model on depressive symptoms and glycated hemoglobin, blood pressure, and serum cholesterol among patients with depression and diabetes in India: the INDEPENDENT randomized clinical trial. JAMA. 2020;324(7):651–62. https://doi.org/10.1001/jama.2020.11747.
Kaur J, Kaur M, Chakrapani V, Webster J, Santos JA, Kumar R. Effectiveness of information technology-enabled “SMART Eating” health promotion intervention: a cluster randomized controlled trial. PloS One. 2020;15(1):e0225892. https://doi.org/10.1371/journal.pone.0225892.
Javaid Z, Imtiaz U, Khalid I, et al. A randomized control trial of primary care-based management of type 2 diabetes by a pharmacist in Pakistan. BMC Health Serv Res. 2019;19(1):409. https://doi.org/10.1186/s12913-019-4274-z.
Naseem S, Ghazanfar H, Assad S, Ghazanfar A. Role of sodium-restricted dietary approaches to control blood pressure in Pakistani hypertensive population. JPMA J Pak Med Assoc. 2016;66(7):837–42.
Ajay VS, Jindal D, Roy A, et al. Development of a smartphone-enabled hypertension and diabetes mellitus management package to facilitate evidence-based care delivery in primary healthcare facilities in India: the mPower Heart Project. J Am Heart Assoc Cardiovasc Cerebrovasc Dis. 2016;5(12):e004343. https://doi.org/10.1161/JAHA.116.004343.
Ali MK, Singh K, Kondal D, et al. Effectiveness of a multicomponent quality improvement strategy to improve achievement of diabetes care goals: a randomized, controlled trial. Ann Intern Med. 2016;165(6):399–408. https://doi.org/10.7326/M15-2807.
Muilwijk M, Loh M, Siddiqui S, et al. Effects of a lifestyle intervention programme after 1 year of follow-up among South Asians at high risk of type 2 diabetes: a cluster randomised controlled trial. BMJ Glob Health. 2021;6(11):e006479. https://doi.org/10.1136/bmjgh-2021-006479.
Vlaar EMA, Nierkens V, Nicolaou M, et al. Effectiveness of a targeted lifestyle intervention in primary care on diet and physical activity among South Asians at risk for diabetes: 2-year results of a randomised controlled trial in the Netherlands. BMJ Open. 2017;7(6):e012221. https://doi.org/10.1136/bmjopen-2016-012221.
Anand SS, Samaan Z, Middleton C, et al. A digital health intervention to lower cardiovascular risk: a randomized clinical trial. JAMA Cardiol. 2016;1(5):601–6. https://doi.org/10.1001/jamacardio.2016.1035.
Kandula NR, Dave S, De Chavez PJ, et al. Translating a heart disease lifestyle intervention into the community: the South Asian Heart Lifestyle Intervention (SAHELI) study; a randomized control trial. BMC Public Health. 2015;15:1064. https://doi.org/10.1186/s12889-015-2401-2.
Samaan Z, Schulze KM, Middleton C, et al. South Asian Heart Risk Assessment (SAHARA): randomized controlled trial design and pilot study. JMIR Res Protoc. 2013;2(2):e33. https://doi.org/10.2196/resprot.2621.
Ramakrishnan S, Zachariah G, Gupta K, et al. Prevalence of hypertension among Indian adults: Results from the great India blood pressure survey. Indian Heart J. 2019;71(4):309–13. https://doi.org/10.1016/j.ihj.2019.09.012.
Roy A, Praveen PA, Amarchand R, et al. Changes in hypertension prevalence, awareness, treatment and control rates over 20 years in National Capital Region of India: results from a repeat cross-sectional study. BMJ Open. 2017;7(7):e015639. https://doi.org/10.1136/bmjopen-2016-015639.
Anchala R, Kannuri NK, Pant H, et al. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32(6):1170–7. https://doi.org/10.1097/HJH.0000000000000146.
Basu S, Malik M, Anand T, Singh A. Hypertension control cascade and regional performance in India: a repeated cross-sectional analys is (2015-2021). Cureus. 15(2):e35449 https://doi.org/10.7759/cureus.35449
Gupta R, Kaur M, Islam S, et al. Association of household wealth index, educational status, and social capital with hypertension awareness, treatment, and control in South Asia. Am J Hypertens. 2017;30(4):373–81. https://doi.org/10.1093/ajh/hpw169.
Irazola VE, Gutierrez L, Bloomfield G, et al. Hypertension prevalence, awareness, treatment, and control in selected LMIC communities: results from the NHLBI/UHG Network of centers of excellence for chronic diseases. Glob Heart. 2016;11(1):47–59. https://doi.org/10.1016/j.gheart.2015.12.008.
Mitchell JD, Fergestrom N, Gage BF, et al. Impact of statins on cardiovascular outcomes following coronary artery calcium scoring. J Am Coll Cardiol. 2018;72(25):3233–42. https://doi.org/10.1016/j.jacc.2018.09.051.
Haque W, Grandhi GR, Kanaya AM, et al. Implications of the 2019 American College of Cardiology/American Heart Association Primary Prevention Guidelines and potential value of the coronary artery calcium score among South Asians in the US: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Atherosclerosis. 2021;334:48–56. https://doi.org/10.1016/j.atherosclerosis.2021.08.030. (Study assessing impact of coronary artery calcium assessment on ASCVD risk prediction and statin prescription among South Asians enrolled in the MASALA cohort in the US.)
Funding
Dr. Virani is supported by the Department of Veterans Affairs, NIH, and Tahir, and Jooma Family Foundation. Farhala Baloch is a Fogarty fellow of NIH Award number D43TW011625.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Virani is a Section Editor for the Springer journals Current Atherosclerosis Reports and Current Cardiology Reports. The other authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Kartik Gupta and Farhala Baloch are co-first authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gupta, K., Baloch, F., Kakar, T.S. et al. The Pandemic of Coronary Heart Disease in South Asia: What Clinicians Need to Know. Curr Atheroscler Rep 25, 359–372 (2023). https://doi.org/10.1007/s11883-023-01110-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11883-023-01110-5