Abstract
Background
This study aimed to assess the determinants of burnout among healthcare providers in the primary care setting.
Methods
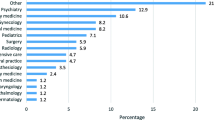
A web-based cross-sectional study was conducted among 1280 healthcare providers aged 18 years and older from 30 primary care clinics in Selangor, Malaysia. In this study, the Copenhagen Burnout Inventory was used to assess burnout. The results were analyzed using multiple logistic regression.
Results
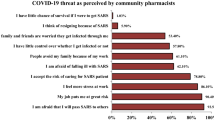
The prevalence of personal burnout was 41.7%, followed by work-related burnout (32.2%) and client-related burnout (14.5%). The determinants for personal burnout in this study were younger age, being a doctor, higher COVID-19 exposure risk, do not know where to seek help, inability to handle stress, poorer sleep quality score, higher total COVID-19 fear score, higher total stress score, and lower total BRS score. The determinants of work-related burnout were younger age, being a doctor, longer years of working, higher COVID-19 exposure risk, do not know where to seek help, lower altruistic score, poorer sleep quality score, higher total stress score, and lower total brief resilience score (BRS) score. The determinants of client-related burnout were doctor, single/divorced, more than one attachment site, and higher satisfaction toward the infection control, inability to handle stress, higher total depression score, and lower total BRS score.
Conclusion
Every fourth out of ten suffered from personal burnout, one-third from work-related burnout, and one-seventh from client-related burnout among healthcare providers during the COVID-19 pandemic. Healthcare systems must take care of healthcare workers’ physical and emotional depletion, reducing the risk of burnout.
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
World Health Organization (2020) Coronavirus disease COVID-19: situation report 126
Ministry of health Malaysia (2022) COVID NOW in Malaysia 2022. https://covidnow.moh.gov.my/. Accessed 17 Mar 2022
Schaufeli WB, Enzmann D, Girault N (2018) Measurement of burnout: a review. Professional burnout: Theory Res Educ 199–215
Kristensen TS, Borritz M, Villadsen E et al (2005) The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress 19:192–207
Cohen R, Healthcare CR (2017) Meta-analysis of relation of vital exhaustion to cardiovascular disease events. Am J Cardiol 119:1211–1216
Jackson ER, Shanafelt TD, Hasan O (2016) Burnout and alcohol abuse/dependence among US medical students. Acad Med 919:1251–1256
Kumar SJ (2016) Burnout and doctors: prevalence, prevention and intervention. In Healthcare 3:37
Bridgeman PJ, Bridgeman MB, Barone J (2018) Burnout syndrome among healthcare professionals. Am J Health Syst Pharm 753:147–152
Hall LH, Johnson J, Heyhoe J et al (2020) Exploring the impact of primary care physician burnout and well-being on patient care: a focus group study. J Patient Saf 164:e278–e283
Dyrbye LN, Shanafelt TD, Johnson PO et al (2019) A cross-sectional study exploring the relationship between burnout, absenteeism, and job performance among American nurses. BMC Nurs 181:1–8
Buchbinder SB, Wilson M, Melick CF et al (2001) Primary care physician job satisfaction and turnover. Am J Manag Care 77:701–716
Shanafelt T, Trockel M, Wang H et al (2022) Assessing professional fulfillment and burnout among CEOs and other healthcare administrative leaders in the United States. J Healthc Manag 675:317–338
Walton DM (2020) Physiotherapists’ perspectives on the threats facing their profession in the areas of leadership, burnout, and branding: a pan-Canadian perspective from the physio moves Canada project, part 3. Physiother Can 721:43–51
Roslan NS, Yusoff MSB, Asrenee AR et al (2021) Burnout prevalence and its associated factors among Malaysian healthcare workers during COVID-19 pandemic: an embedded mixed-method study. In Healthcare 9:1–90
Yao LM, Hung CS, Ain SN et al (2022) Prevalence of burnout syndrome and its associated factors among doctors in Sabah, Malaysia. Psychol Health Med 276:1373–1380
Zakaria MI, Remeli R, Ahmad Shahamir MF et al (2021) Assessment of burnout among emergency medicine healthcare workers in a teaching hospital in Malaysia during COVID-19 pandemic. Hong Kong J Emerg Med 28(4):254–259
Chin RWA, Chua YY, Chu MN et al (2018) Investigating validity evidence of the Malay translation of the Copenhagen Burnout Inventory. J Taibah Univ Medical Sci 131:1–9
Ahorsu DK, Lin CY, Imani V (2020) The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict 1–9
Smith BW, Dalen J, Wiggins K (2008) The brief resilience scale: assessing the ability to bounce back. Int J Behav Med 15:194–200
Lovibond PF, Lovibond SH (1995) The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales DASS with the Beck Depression and Anxiety Inventories. Behav Res Ther 333:335–343
Mohammad AH, Shamsudin SB, Kamarudin NA et al (2021) Occupational burnout among public medical officers during the early stage of Covid-19 pandemic in Kota Kinabalu, Sabah. Malaysian J Public Health Med 211:317–326
Carr E, Murray ET, Zaninotto P et al (2018) The association between informal caregiving and exit from employment among older workers: prospective findings from the UK Household Longitudinal Study. J Gerontol B Psychol Sci Soc Sci 737:1253–1262
Swazo NK, Talukder MMH et al (2020) A duty to treat? A right to refrain? Bangladeshi physicians in moral dilemma during COVID-19. Philos Ethics Humanit Med 15:1–23
Dyrbye LN, West CP, Halasy M et al (2020) Burnout and satisfaction with work-life integration among PAs relative to other workers. JAAPA 335:35–44
Luceño-Moreno L, Talavera-Velasco B et al (2020) Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. Int J Environ Res Public Health 1715:5514
Iacovides A, Fountoulakis KN, Kaprinis S et al (2003) The relationship between job stress, burnout and clinical depression. J Affect Disord 753:209–221
Romani M, Ashkar K et al (2014) Burnout among physicians. Libyan J Med 91
McCain RS, McKinley N, Dempster M et al (2018) A study of the relationship between resilience, burnout and coping strategies in doctors. Postgrad Med J 941107:43–47
West CP, Dyrbye LN, Sinsky C et al (2020) Resilience and burnout among physicians and the general US working population. JAMA Netw Open 37:e209385–e209385
Sayılan AA, Kulakac N, Uzun S (2021). Burnout levels and sleep quality of COVID-19 heroes. Perspect Psychiatr Care
Giorgi F, Mattei A, Notarnicola I et al (2018) Can sleep quality and burnout affect the job performance of shift-work nurses? A hospital cross-sectional study. J Adv Nurs 743:698–708
Nteveros A, Kyprianou M, Artemiadis A et al (2020) Burnout among medical students in Cyprus: a cross-sectional study. PLoS ONE 1511:e0241335
Khattak SR, Saeed I, Rehman SU et al (2021) Impact of fear of COVID-19 pandemic on the mental health of nurses in Pakistan. J Loss Trauma 265:421–435
Alharbi J, Jackson D, Usher K (2020) The potential for COVID-19 to contribute to compassion fatigue in critical care nurses. J Clin Nurs 29:2762
Abdelghani M, El-Gohary HM, Fouad E (2020) Addressing the relationship between perceived fear of COVID-19 virus infection and emergence of burnout symptoms in a sample of Egyptian physicians during COVID-19 pandemic: a cross-sectional study. Middle East Curr Psychiatry 27:1–9
Urooj U, Ansari A, Siraj A et al (2020) Expectations, fears and perceptions of doctors during Covid-19 pandemic. Pak J Med Sci 36(COVID19-4):37
Golabi F, Bagher M, Akbarian H (2021) Correlation between job burnout and Fear of COVID-19 among ICU and CCU Nurses Case study: Shahid Madani Cardiac Hospital, Tabriz. Iran Arch Nurs Pract Care 71:24–28
Duarte I, Teixeira A, Castro L et al (2020) Burnout among Portuguese healthcare workers during the COVID-19 pandemic. BMC Public Health 201:1–10
Jose S, Dhandapani M, Cyriac MC et al (2020) Burnout and resilience among frontline nurses during COVID-19 pandemic: a cross-sectional study in the emergency department of a tertiary care center, North India. Indian J Crit Care Med 2411:1081
Ferreira P, Gomes S (2021) The role of resilience in reducing burnout: a study with healthcare workers during the COVID-19 pandemic. Soc Sci 109:317
Damman M, Henkens K, Kalmijn M (2013) Late-career work disengagement: the role of proximity to retirement and career experiences. J Gerontol B Psychol Sci Soc Sci 683:455–463
Karasek RA Jr (1979) Job demands, job decision latitude, and mental strain: Implications for job redesign. Adm Sci Q 285–308
De Hert S (2020) Burnout in healthcare workers: prevalence, impact and preventative strategies. Local Reg Anesthesia 13:171
Baptista S, Teixeira A, Castro L et al (2021) Physician burnout in primary care during the COVID-19 pandemic: a cross-sectional study in Portugal. J Prim Care Community Health 12:21501327211008436
Youssef D, Youssef J, Hassan H et al (2021) Prevalence and risk factors of burnout among Lebanese community pharmacists in the era of COVID-19 pandemic: results from the first national cross-sectional survey. J Pharm Policy Pract 141:1–12
Mira JJ, Carrillo I, Guilabert M, Mula A (2020) Acute stress of the healthcare workforce during the COVID-19 pandemic evolution: a cross-sectional study in Spain. BMJ Open 1011:e042555
Ferry AV, Wereski R, Strachan FE et al (2021) Predictors of UK healthcare worker burnout during the COVID-19 pandemic. QJM-Int J Med 1146:374–380
Győrffy Z, Birkás E, Sándor I (2016) Career motivation and burnout among medical students in Hungary-could altruism be a protection factor? BMC Med Educ 16:1–8
Vaughn EC (2013) Assessing altruistic behavior, burnout, and wellness outcomes of entry level, live-in and live on residence life professionals. Louisiana State University and Agricultural & Mechanical College
West CP, Dyrbye LN, Shanafelt TD (2018) Physician burnout: contributors, consequences and solutions. J Intern Med 2836:516–529
Bakker AB, Demerouti E (2017) Job demands–resources theory: taking stock and looking forward. J Occup Health Psychol 223:273
Huo L, Zhou Y, Li S et al (2021) Burnout and its relationship with depressive symptoms in medical staff during the COVID-19 epidemic in China. Front Psychol 12:616369
Lee D, McLanahan S (2015) Family structure transitions and child development: instability, selection, and population heterogeneity. Am Sociol Rev 804:738–763
Maunder RG, Hunter JJ (2016) Can patients be ‘attached’ to healthcare providers? An observational study to measure attachment phenomena in patient–provider relationships. BMJ Open 65:e011068
Chirico F, Nucera G, Magnavita N (2020) COVID-19: protecting healthcare workers is a priority. Infect Control Hosp Epidemiol 419:1117–1117
Azlan AA, Hamzah MR, Sern TJ et al (2020) Public knowledge, attitudes and practices towards COVID-19: a cross-sectional study in Malaysia. PLoS ONE 155:e0233668
Sazali MF, Rahim SSSA, Mohamed MH et al (2021) Knowledge, attitude and practice on COVID-19 among students during the early phase of pandemic in a university in Borneo. Malaysia J Public Health Res 103:2021
Arnetz JE, Zhdanova L, Arnetz BB (2016) Patient involvement: a new source of stress in health care work? Health commun 3112:1566–1572
Haghighinejad H, Ghazipoor H, Jafari P et al (2020) Investigating the impact of modified mindfulness-based stress reduction MBSR program on occupational burnout and other mental health status among nonmedical staff in a hospital: a randomized controlled trial. Int Arch Occup Enviro 9510:2005–2016
Koutsimani P, Montgomery A, Georganta K (2019) The relationship between burnout, depression, and anxiety: a systematic review and meta-analysis. Front Psychol 284
Segal DL (2010) Diagnostic and statistical manual of mental disorders DSM‐IV‐TR. The Corsini Encyclopedia of Psychol 1–3
Ahola K, Hakanen J, Perhoniemi R (2014) Relationship between burnout and depressive symptoms: a study using the person-centred approach. Burn Res 11:29–27
Aumayr-Pintar C, Cerf C, Parent-Thirion A (2018) Burnout in the workplace: a review of the data and policy responses in the EU
Gusmano MK, Maschke KJ, Solomon MZ (2019) Patient-centered care, yes; patients as consumers, no. Health Aff 383:368–373
Acknowledgements
We would like to thank the Director General of Health Malaysia for his permission to publish this article. The author would like to acknowledge the Selangor JKNS Health Office and the Director of Health for their support of our study. The author would like to thank all Family Medicine Specialist for providing support during the data collection. We would like to extend our appreciation to all respondents in this study.
Funding
This research received funding from the Family Medicine Specialist Association (FMSA (5) 02/20–22). The funder had no role in study design, data collection and analysis, the decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
CSM, ATC, PYL, IIZ, KWL, and SWT involved in the design of the study design of the study, or acquisition of data, or analysis and interpretation of data. CSM, VR, and KWL involved in drafting the article or revising it critically for important intellectual content. All authors involved in review and editing and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was obtained from the Ethics Committee of the National Malaysia Research Registry (NMRR ID-21–02084-IUO (IIR)) prior to data collection. Written informed consent was obtained from the all the respondents.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ching, SM., Cheong, A.T., Yee, A. et al. Prevalence and factors associated with burnout among healthcare providers in Malaysia: a web-based cross-sectional study. Ir J Med Sci 193, 851–863 (2024). https://doi.org/10.1007/s11845-023-03483-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-023-03483-7