Abstract
Background and aims
The learning curve for robotic-assisted radical prostatectomy (RARP) is estimated to be about 50–200 cases. This study will evaluate the benefit of a mentorship programme after completing a mini-fellowship in RARP by an experienced surgeon who previously trained in open and laparoscopic surgery.
Methods
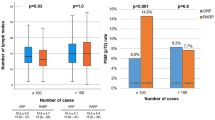
Our study was a retrospective comparative analysis of RARP performed by a single consultant urologist. A retrospective chart review of the first 120 cases was performed. The 120 patients were divided into three groups of 40 cases. For the first 40 cases, an appropriately qualified mentor was present. The peri-operative and oncological outcomes were compared between the three groups.
Results
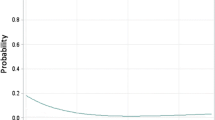
Operative times significantly decreased with experience (250 min vs 234 min vs 225 min, p < 0.05). Complication rates, estimated blood loss, and length of stay were similar between all groups. There was a higher rate of positive margins in the final group (20% vs 17.5% vs 32.5%, p < 0.5). There was a greater number of pT3 tumours in group 3 (42%, n = 17) compared to groups 1 and 2 (20%, n = 8, and 22.5%, n = 9) which may account for the higher rate of positive margins in this group.
Conclusion
In the transition of an experienced laparoscopic surgeon to robotic surgery, we showed that there is a benefit of a mentorship programme after a mini-fellowship in reducing the impact of the learning curve on patient outcomes. Ongoing mentorship may be of benefit in cases where a high volume of tumour is suspected and should be avoided in the early part of the learning curve to maximise oncological outcomes.

Similar content being viewed by others
Abbreviations
- RARP:
-
Robotic-assisted robotic prostatectomy
- BAUS:
-
British Association of Urological Surgery
- ERUS:
-
European Association of Urology Robotic Urology Section
- RP:
-
Radical prostatectomy
- ISUP:
-
International Society of Urological Pathology
- ERAS:
-
Enhanced recovery assessment protocol
- IHD:
-
Ischaemic heart disease
- EBL:
-
Estimated blood loss
- IV:
-
Intravenous
References
Binder J, Kramer W (2001) Robotically-assisted laparoscopic radical prostatectomy. BJU Int 87(4):408–410
Khadhouri S, Miller C, Fowler S et al (2018) The British Association of Urological Surgeons (BAUS) radical prostatectomy audit 2014/2015 - an update on current practice and outcomes by centre and surgeon case-volume. BJU Int 121(6):886–892
Nyberg M, Hugosson J, Wiklund P et al (2018) Functional and oncologic outcomes between open and robotic radical prostatectomy at 24-month follow-up in the Swedish LAPPRO Trial. Eur Urol Oncol 1(5):353–360
Kowalewski KF, Schmidt MW, Proctor T et al (2018) Skills in minimally invasive and open surgery show limited transferability to robotic surgery: results from a prospective study. Surg Endosc 32(4):1656–1667
Volpe A, Ahmed K, Dasgupta P et al (2015) Pilot validation study of the European Association of Urology robotic training curriculum. Eur Urol 68(2):292–299
Lovegrove C, Novara G, Mottrie A et al (2016) Structured and modular training pathway for robot-assisted radical prostatectomy (RARP): validation of the RARP assessment score and learning curve assessment. Eur Urol 69(3):526–535
Merseburger AS, Herrmann TRW, Shariat SF et al (2013) EAU Guidelines on Robotic and Single-site Surgery in Urology. Eur Urol [Internet]. 64(2):277–91. Available from: http://www.sciencedirect.com/science/article/pii/S0302283813005022
Sooriakumaran P, John M, Wiklund P et al (2011) Learning curve for robotic assisted laparoscopic prostatectomy: a multi-institutional study of 3794 patients. Minerva Urol Nefrol 63(3):191–198
Brierley J, Gospodarowicz MK, Wittekind C (2018) TNM Classification of Malignant Tumours. 8th editio. Blackwell, Oxford
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Doumerc N, Yuen C, Savdie R et al (2010) Should experienced open prostatic surgeons convert to robotic surgery? The real learning curve for one surgeon over 3 years. BJU Int 106(3):378–384
Abboudi H, Khan MS, Guru KA et al (2014) Learning curves for urological procedures: a systematic review. BJU Int 114(4):617–629
Rashid HH, Leung YYM, Rashid MJ et al (2006) Robotic surgical education: a systematic approach to training urology residents to perform robotic-assisted laparoscopic radical prostatectomy. Urology 68(1):75–9.
McDougall EM, Corica FA, Chou DS et al (2006) Short-term impact of a robot-assisted laparoscopic prostatectomy “mini-residency” experience on postgraduate urologists’ practice patterns. Int J Med Robot 2(1):70–74
Kwon EO, Bautista TC, Jung H et al (2010) Impact of robotic training on surgical and pathologic outcomes during robot-assisted laparoscopic radical prostatectomy. Urology 76(2):363–368
Vasdev N, Bishop C, Kass-Iliyya A et al (2013) Developing a robotic prostatectomy service and a robotic fellowship programme - defining the learning curve. Curr Urol 7(3):136–144
Islamoglu E, Karamik K, Ozsoy C et al (2018) The learning curve does not affect positive surgical margin status in robot-assisted laparoscopic prostatectomy. Urol J 15(6):333–338
Wang L, Diaz M, Stricker H et al (2017) Adding a newly trained surgeon into a high-volume robotic prostatectomy group: are outcomes compromised? J Robot Surg 11(1):69–74
Gamboa AJR, Santos RT, Sargent ER et al (2009) Long-term impact of a robot assisted laparoscopic prostatectomy mini fellowship training program on postgraduate urological practice patterns. J Urol 181(2):778–782
Badani KK, Hemal AK, Peabody JO, Menon M (2006) Robotic radical prostatectomy: the Vattikuti Urology Institute training experience. World J Urol [Internet] 24(2):148—151. Available from: https://doi.org/10.1007/s00345-006-0072-4
Birch DW, Asiri AH, de Gara CJ (2007) The impact of a formal mentoring program for minimally invasive surgery on surgeon practice and patient outcomes. Am J Surg [Internet] 193(5):589—91; discussion 591—2. Available from: https://doi.org/10.1016/j.amjsurg.2007.01.0032007
Hung AJ, Chen J, Shah A, Gill IS (2018) Telementoring and telesurgery for minimally invasive procedures. J Urol 199(2):355–369
Funding
The authors received no funding as part of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Ryan, J.P.C., Lynch, O., Broe, M.P. et al. Robotic-assisted radical prostatectomy—impact of a mentorship program on oncological outcomes during the learning curve. Ir J Med Sci 191, 479–484 (2022). https://doi.org/10.1007/s11845-021-02556-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02556-9