Abstract
Background
The recognition of sleep disorders is important because in the long term, they are associated with numerous deleterious health outcomes. Despite the high prevalence of sleep disorders, they are widely under-diagnosed at general practice level.
Aim
This study aims to investigate the association between demographic and morbidity factors, and self-reported sleep disturbance symptoms.
Methods
A quantitative cross-sectional study design was used. The data collection tool was an anonymous questionnaire consisting of 22 sleep symptoms categorised into four subscales: 1. Insomnia, 2. Daytime Distress, 3. Sleep Disorder, 4. Psychological Distress. Participants were adults ≥18 years of age attending their general practitioner.
Results
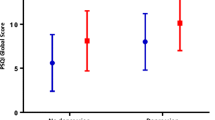
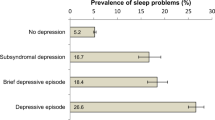
A total of 281 questionnaires were analysed (70.3% response rate). Participants with a diagnosis of depression and those who experienced low mood ‘very frequently’ had significantly higher median scores on all four subscales. Those with a body mass index (BMI) >30 kg/m2 had a higher median score on subscale 3, compared to those with lower BMIs. Smokers had higher median scores on subscales 1–3 compared to non-smokers. Participants >65 years of age had lower median scores on all subscales compared to younger participants. Married participants had lower median scores on subscales 1–3 compared to unmarried participants. A total of 37% reported that they would be willing to participate in an overnight sleep study, and 5.3% had been formally diagnosed with a sleep disorder.
Conclusions
A number of factors are significantly associated with sleep disturbance, particularly depression, low mood, elevated BMI and smoking. General practitioners should consider these factors to increase recognition of patients who would benefit from sleep disorder investigation.

Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- GP:
-
General practitioner
- IQR:
-
Interquartile range
- OR:
-
Odds ratio
- OSA:
-
Obstructive sleep apnoea
- PSG:
-
Polysomnography
- SD:
-
Standard deviation
- SSC:
-
Sleep symptom checklist
References
Sorscher AJ (2008) How is your sleep: a neglected topic for health care screening. Journal of the American Board of Family Medicine : JABFM. 21(2):141–148
Irish Sleep Society. Guidelines for the assessment and management of patients with sleep disorders. [Online]. 2010 Feb 1 [cited 2014 Oct 5]. Available from: URL:http://www.irishsleepsociety.org/.
Irish Sleep Apnoea Trust. Sleep apnoea is a very serious medical condition. [Online]. 2014 Aug 19 [cited 2014] Available from: URL:http://www.isat.ie/index.html.
Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N (2010) "sleep disparity" in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health 10:475
Mold JW, Quattlebaum C, Schinnerer E, Boeckman L, Orr W, Hollabaugh K (2011) Identification by primary care clinicians of patients with obstructive sleep apnea: a practice-based research network (PBRN) study. Journal of the American Board of Family Medicine : JABFM. 24(2):138–145
Hayes SM, Murray S, Castriotta RJ, Landrigan CP, Malhotra A (2012) (Mis) perceptions and interactions of sleep specialists and generalists: obstacles to referrals to sleep specialists and the multidisciplinary team management of sleep disorders. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine. 8(6):633–642
Sivertsen B, Nordhus IH, Bjorvatn B, Pallesen S (2010) Sleep problems in general practice: a national survey of assessment and treatment routines of general practitioners in Norway. J Sleep Res 19(1 Pt 1):36–41
Bailes S, Baltzan M, Rizzo D, Fichten CS, Grad R, Wolkove N et al (2009) Sleep disorder symptoms are common and unspoken in Canadian general practice. Fam Pract 26(4):294–300
Senthilvel E, Auckley D, Dasarathy J (2011) Evaluation of sleep disorders in the primary care setting: history taking compared to questionnaires. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine. 7(1):41–48
Unruh MLRSM-WDJNFJJ-LAB (2008) Subjective and objective sleep quality and aging in the sleep heart health study. J am Geriatr Soc 56(7):1218–1227
Alattar M, Harrington JJ, Mitchell CM, Sloane P (2007) Sleep problems in primary care: a North Carolina Family Practice Research Network (NC-FP-RN) study. Journal of the American Board of Family Medicine : JABFM. 20(4):365–374
Dregan A, Armstrong D (2011) Cross-country variation in sleep disturbance among working and older age groups: an analysis based on the European Social Survey. Int Psychogeriatr 23(9):1413–1420
Wall H, Smith C, Hubbard R (2012) Body mass index and obstructive sleep apnoea in the UK: a cross-sectional study of the over-50s. Primary Care Respiratory Journal : Journal of the General Practice Airways Group 21(4):371–376
Namyslowski G, Scierski W, Mrowka-Kata K, Kawecka I, Kawecki D, Czecior E (2005) Sleep study in patients with overweight and obesity. Journal of Physiology and Pharmacology : an Official Journal of the Polish Physiological Society 56(Suppl 6):59–65
Troxel WM, Buysse DJ, Matthews KA, Kravitz HM, Bromberger JT, Sowers M et al (2010) Marital/cohabitation status and history in relation to sleep in midlife women. Sleep 33(7):973–981
Meyer KA, Wall MM, Larson NI, Laska MN, Neumark-Sztainer D (2012) Sleep duration and BMI in a sample of young adults. Obesity (Silver Spring, md) 20(6):1279–1287
Aamhe M, Weir NA, Gillum RF (2014) Gender and the association of smoking with sleep quantity and quality in American adults. Women & Health 54(1):1–14
McNamara JPHWJDBWJYMAM-BJCS (2014) Sleep disturbances associated with cigarette smoking. Psychology, Health & Medicine 19(4):410–419
Vinson DC, Manning BK, Galliher JM, Dickinson LM, Pace WD, Turner BJ (2010) Alcohol and sleep problems in primary care patients: a report from the AAFP National Research Network. Ann fam med 8(6):484–492
Peppard PE, Austin D, Brown RL (2007) Association of alcohol consumption and sleep disordered breathing in men and women. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine 3(3):265–270
Almeida OP, Pfaff JJ (2005) Sleep complaints among older general practice patients: association with depression. The British Journal of General Practice : the Journal of the Royal College of General Practitioners. 55(520):864–866
Bluestein D, Rutledge CM, Healey AC (2010) Psychosocial correlates of insomnia severity in primary care. Journal of the American Board of Family Medicine : JABFM 23(2):204–211
Livingston G, Blizard B, Mann A (1993) Does sleep disturbance predict depression in elderly people? A study in inner London. The British Journal of General Practice : the Journal of the Royal College of General Practitioners 43(376):445–448
Omachi TA (2011) Measures of sleep in rheumatologic diseases: Epworth Sleepiness Scale (ESS), Functional Outcome of Sleep Questionnaire (FOSQ), Insomnia Severity Index (ISI), and Pittsburgh Sleep Quality Index (PSQI). Arthritis Care & Research 63(Suppl 11):S287–S296
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no potential conflicts of interest.
Research involving human participants
Questionnaires were distributed at selected general practices. Questionnaires were accompanied by an information sheet for participants. Questionnaires were anonymous so no consent forms were required.
Appendices
Appendices
1. Questionnaire


2. Ethical approval and application documents

Rights and permissions
About this article
Cite this article
Mullane, N., Bradley, C. An investigation into the association between demographic and morbidity factors, and sleep disturbance. Ir J Med Sci 187, 163–175 (2018). https://doi.org/10.1007/s11845-017-1640-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-017-1640-x