Abstract
Background
Medication discrepancies at the time of hospital discharge are common and can result in error, patient/carer inconvenience or patient harm. Providing accurate medication information to the next care provider is necessary to prevent adverse events.
Aims
To investigate the quality and consistency of medication details generated for such transfer from an Irish teaching hospital.
Methods
This was an observational study of 139 cardiology patients admitted over a 3 month period during which a pharmacist prospectively recorded details of medication inconsistencies.
Results
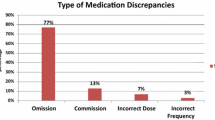
A discrepancy in medication documentation at discharge occurred in 10.8% of medication orders, affecting 65.5% of patients. While patient harm was assessed, it was only felt necessary to contact three (2%) patients. The most common inconsistency was drug omission (20.9%).
Conclusions
Inaccuracy of medication information at hospital discharge is common and compromises quality of care.
Similar content being viewed by others
References
Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW (2003) The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Int Med 138(3):161–167
Forster AJ, Clark HD, Menard A, Dupuis N, Chernish R, Chandok N et al (2004) Adverse events among medical patients after discharge from hospital. CMAJ 170(3):345–349
Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW (2005) Adverse drug events occurring following hospital discharge. J Gen Inter Med 20(4):317–323
Duggan C, Feldman R, Hough J, Bates I (1998) Reducing adverse prescribing discrepancies following hospital discharge. Int J Pharm Pract 6:77–82
Colemann A (2002) Discharge information needs to be improved to prevent prescribing errors. Pharm J 268:81–86
Gandhi T, Sittig D, Franklin M, Sussman A, Fairchild D, Bates D (2000) Communication breakdown in the outpatient referral process. J Gen Intern Med 15:626–631
Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW (2007) Deficits in communication and information transfer between hospital based and primary care physicians. Implications for patient safety and continuity of care. JAMA 297(8):831–841
Smith J (2004) Building a safer NHS for patients: improving medication safety: Department of Health (UK)
Joint Commission on Accreditation of Healthcare Organizations (JCAHO) 2006 National Patient Safety Goals, Goal 8 hospital version accurately and completely reconcile medications across the continuum of care http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/06_npsg_cah.htm. Accessed 23 Nov 2006
Dean BS, Barber ND (1999) A validated, reliable method of scoring the severity of medication errors. AJHP 56:57–62
Dean B, Barber N, Schachter M (2000) What is a prescribing error? Qual Health Care 9:232–237
Sexton J, Brown A (1999) Problems with medicines following hospital discharge: not always the patient’s fault? J Soc Adm Pharm 16(3/4):199–207
Coleman EA, Parry C, Chalmers S, Min SJ (2006) The care transitions intervention: results of a randomised controlled trial. Arch Intern Med 166(17):1822–1828
Franklin BD, O’Grady K, Paschalides C, Utley M, Gallivan S, Jacklin A, Barber N (2007) Providing feedback to hospital doctors about prescribing errors: a pilot study. Pharm World Sci 29(3):213–220
Tully MP, McElduff P (2005) Identification of prescribing errors at different stages of hospital admission. IJPP 13:R29 (abstract)
Reason J (1997) Managing the risks of organisational accidents. Ashgate, Vermont
Cohen MR (2007) Medication errors, 2nd edn. American Pharmacists Association, Washington
Dean B, Schachter M, Vincent C, Barber N (2002) Causes of prescribing errors in hospital inpatients: a prospective study. Lancet 359(9315):1373–1378
Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, Burdick E, Hickey M, Kleefield S, Shea B, Vander Vliet M, Seger DL (1998) Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA 280:1311–1316
Bates DW, Teich JM, Lee J, Seger D, Kuperman GJ, Ma’Luf N, Boyle D, Leape L (1999) the impact of computerized physician order entry on medication error prevention. JAMIA 6:313–321
Donyai P, O Grady K, Jacklin A, Barber N, Franklin BD (2007) The effects of electronic prescribing on the quality of prescribing. Br J Clin Pharm; Online early article (July), doi:10.1111/j.1365–2125.2007.02995.x
Schnipper JL, Kirwin JL, Cotungo MC, Wahlstrom SA, Brown BA, Tarvin E et al (2006) Role of pharmacist counselling in preventing adverse drug events after hospitalization. Arch Intern Med 166(5):565–571
Beagon P, Scott M, McElnay J (2004) Quantifying the impact of an intensive clinical pharmacy service on readmission rates to hospital. Pharm World Sci 26:A9
Scullin C, Scott MG, Hogg A, McElnay JC (2007) An innovative approach to integrated medicines management. J Eval Clin Pract; online early release July 2007: doi: 10.1111/j.1365–2753.2006.00753.x
Sexton J, Ho YJ, Green CF, Caldwell NA (2000) Ensuring seamless care at hospital discharge: a national survey. J Clin Pharm Ther 25(5):385–393
Jackson C, Owe P, Lea R (1993) Pharmacy discharge—a professional necessity for the 1990s. Pharm J 250:502–506
Delaney T (2007) Hospital pharmacy staffing and workload in Irish acute hospitals. IPJ 85(4):136–144
Health Service Executive. Transformation programme 2007–2010. http://www.hse.ie/en/Publications/TransformationProgramme2007–2010/FiletoUpload,4309,en.pdf. Accessed 30 Aug 2007
Acknowledgments
Completion of this study would not have been possible without the help of nursing, pharmacy, medical and administrative staff in the study hospital. The authors also wish to acknowledge the time and input of those involved in assessing the clinical importance of medication errors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grimes, T., Delaney, T., Duggan, C. et al. Survey of medication documentation at hospital discharge: implications for patient safety and continuity of care. Ir J Med Sci 177, 93–97 (2008). https://doi.org/10.1007/s11845-008-0142-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-008-0142-2