Abstract
Purpose
Cisplatin-induced hearing loss (CIHL) is a common late effect after childhood cancer treatment having profound, lifelong consequences that lower quality of life. The recent identification of intravenous sodium thiosulfate (STS) as an effective agent for preventing pediatric CIHL represents a paradigm shift that has created new opportunities for expanding STS usage and developing additional otoprotectants. The purpose of this paper is to discuss key considerations and recommendations for the design and implementation of future pediatric otoprotection trials.
Methods
An approach synthesizing published data and collective experience was used.
Results
Key issues were identified in the categories of translational research, trial designs for systemic and intratympanic agents, measurement of ototoxicity, and biostatistical challenges.
Conclusions
Future pediatric otoprotection trials should emphasize (1) deep integration of preclinical and early-phase studies; (2) an embedded or free-standing design for systemic agents based on mechanistic considerations; (3) use of suitable audiologic testing batteries for children, SIOP grading criteria, and submission of raw audiologic data for central review; and (4) novel endpoints and innovative study designs that maximize trial efficiency for limited sample sizes. Additional recommendations include routine collection of DNA specimens for assessing modifying effects of genetic susceptibility and meaningful inclusion of patient/family advocates for informing trial development.
Implications for Cancer Survivors
Changing the historical paradigm from acceptance to prevention of pediatric CIHL through expanded research with existing and emerging otoprotectants will dramatically improve quality of life for future childhood cancer survivors exposed to cisplatin.


Similar content being viewed by others
Data Availability
All data cited in this review article are available in the public domain.
References
Ghosh S. Cisplatin: the first metal based anticancer drug. Bioorg Chem. 2019;88:102925.
Brock PR, et al. Platinum-induced ototoxicity in children: a consensus review on mechanisms, predisposition, and protection, including a new International Society of Pediatric Oncology Boston ototoxicity scale. J Clin Oncol. 2012;30(19):2408–17.
van As JW, van den Berg H, van Dalen EC. Platinum-induced hearing loss after treatment for childhood cancer. Cochrane Database Syst Rev. 2016;(8):CD010181.
Moke DJ, et al. Prevalence and risk factors for cisplatin-induced hearing loss in children, adolescents, and young adults: a multi-institutional North American cohort study. Lancet Child Adolesc Health. 2021;5(4):274–83.
Knight KR, Kraemer DF, Neuwelt EA. Ototoxicity in children receiving platinum chemotherapy: underestimating a commonly occurring toxicity that may influence academic and social development. J Clin Oncol. 2005;23(34):8588–96.
Gurney JG, et al. Hearing loss, quality of life, and academic problems in long-term neuroblastoma survivors: a report from the Children’s Oncology Group. Pediatrics. 2007;120(5):e1229–36.
Landier W, et al. Ototoxicity in children with high-risk neuroblastoma: prevalence, risk factors, and concordance of grading scales–a report from the Children’s Oncology Group. J Clin Oncol. 2014;32(6):527–34.
Brinkman TM, et al. Treatment-induced hearing loss and adult social outcomes in survivors of childhood CNS and non-CNS solid tumors: results from the St. Jude Lifetime Cohort Study Cancer. 2015;121(22):4053–61.
Orgel E, et al. Effect of sensorineural hearing loss on neurocognitive functioning in pediatric brain tumor survivors. Pediatr Blood Cancer. 2016;63(3):527–34.
Bass JK, et al. Association of hearing impairment with neurocognition in survivors of childhood cancer. JAMA Oncol. 2020;6(9):1363–71.
Sininger YS, Grimes A, Christensen E. Auditory development in early amplified children: factors influencing auditory-based communication outcomes in children with hearing loss. Ear Hear. 2010;31(2):166–85.
Frisina RD, et al. Comprehensive audiometric analysis of hearing impairment and tinnitus after cisplatin-based chemotherapy in survivors of adult-onset cancer. J Clin Oncol. 2016;34(23):2712–20.
The Voice of the Patient Hyattsville, MD2018 [updated September 13, 2018. Available from: https://www.fda.gov/media/132522/download
Orgel E, et al. Assessment of provider perspectives on otoprotection research for children and adolescents: a Children’s Oncology Group Cancer Control and Supportive Care Committee survey. Pediatr Blood Cancer. 2020;67(11):e28647.
Mukherjea D, et al. Strategies to reduce the risk of platinum containing antineoplastic drug-induced ototoxicity. Expert Opin Drug Metab Toxicol. 2020;16(10):965–82.
Steyger PS. Mechanisms of aminoglycoside- and cisplatin-induced ototoxicity. Am J Audiol. 2021;30(3S):887–900.
Park MS, De Leon M, Devarajan P. Cisplatin induces apoptosis in LLC-PK1 cells via activation of mitochondrial pathways. J Am Soc Nephrol. 2002;13(4):858–65.
Bragado P, et al. Apoptosis by cisplatin requires p53 mediated p38alpha MAPK activation through ROS generation. Apoptosis. 2007;12(9):1733–42.
Sheth S, et al. Mechanisms of cisplatin-induced ototoxicity and otoprotection. Front Cell Neurosci. 2017;11:338.
Yu W, et al. Cisplatin generates oxidative stress which is accompanied by rapid shifts in central carbon metabolism. Sci Rep. 2018;8(1):4306.
Dasari S, Tchounwou PB. Cisplatin in cancer therapy: molecular mechanisms of action. Eur J Pharmacol. 2014;740:364–78.
Guthrie OW. DNA repair proteins and telomerase reverse transcriptase in the cochlear lateral wall of cisplatin-treated rats. J Chemother. 2009;21(1):74–9.
Laurell G, et al. Effects of a single high dose of cisplatin on the melanocytes of the stria vascularis in the guinea pig. Audiol Neurootol. 2007;12(3):170–8.
Slattery EL, et al. Cisplatin exposure damages resident stem cells of the mammalian inner ear. Dev Dyn. 2014;243(10):1328–37.
Breglio AM, et al. Cisplatin is retained in the cochlea indefinitely following chemotherapy. Nat Commun. 2017;8(1):1654.
Yancey A, et al. Risk factors for cisplatin-associated ototoxicity in pediatric oncology patients. Pediatr Blood Cancer. 2012;59(1):144–8.
Li Y, Womer RB, Silber JH. Predicting cisplatin ototoxicity in children: the influence of age and the cumulative dose. Eur J Cancer. 2004;40(16):2445–51.
Clemens E, et al. Genetic variation of cisplatin-induced ototoxicity in non-cranial-irradiated pediatric patients using a candidate gene approach: the International PanCareLIFE study. Pharmacogenomics J. 2020;20(2):294–305.
Drogemoller BI, et al. Pharmacogenomics of cisplatin-induced ototoxicity: successes, shortcomings, and future avenues of research. Clin Pharmacol Ther. 2019;106(2):350–9.
Meijer AJM, et al. TCERG1L allelic variation is associated with cisplatin-induced hearing loss in childhood cancer, a PanCareLIFE study. NPJ Precis Oncol. 2021;5(1):64.
Langer T, et al. Usefulness of current candidate genetic markers to identify childhood cancer patients at risk for platinum-induced ototoxicity: results of the European PanCareLIFE cohort study. Eur J Cancer. 2020;138:212–24.
Lewis MJ, et al. Ototoxicity in children treated for osteosarcoma. Pediatr Blood Cancer. 2009;52(3):387–91.
Qaddoumi I, et al. Carboplatin-associated ototoxicity in children with retinoblastoma. J Clin Oncol. 2012;30(10):1034–41.
Parsons SK, et al. Severe ototoxicity following carboplatin-containing conditioning regimen for autologous marrow transplantation for neuroblastoma. Bone Marrow Transplant. 1998;22(7):669–74.
Walker DA, et al. Enhanced cis-platinum ototoxicity in children with brain tumours who have received simultaneous or prior cranial irradiation. Med Pediatr Oncol. 1989;17(1):48–52.
Kohn S, et al. Ototoxicity resulting from combined administration of cisplatin and gentamicin. Laryngoscope. 1997;107(3):407–8.
Lin X, et al. Experimental animal models of drug-induced sensorineural hearing loss: a narrative review. Ann Transl Med. 2021;9(17):1393.
Todd DW, et al. A fully automated high-throughput zebrafish behavioral ototoxicity assay. Zebrafish. 2017;14(4):331–42.
Hazlitt RA, et al. Development of second-generation CDK2 inhibitors for the prevention of cisplatin-induced hearing loss. J Med Chem. 2018;61(17):7700–9.
Ingersoll MA, et al. BRAF inhibition protects against hearing loss in mice. Sci Adv. 2020;6(49).
Teitz T, et al. Development of cell-based high-throughput chemical screens for protection against cisplatin-induced ototoxicity. Methods Mol Biol. 2016;1427:419–30.
Fernandez K, et al. An optimized, clinically relevant mouse model of cisplatin-induced ototoxicity. Hear Res. 2019;375:66–74.
Wong HH, Halford S. Dose-limiting toxicity and maximum tolerated dose: still fit for purpose? Lancet Oncol. 2015;16(13):1287–8.
Filloon TG. Estimating the minimum therapeutically effective dose of a compound via regression modelling and percentile estimation. Stat Med. 1995;14(9–10):925–32; discussion 33.
Fraisse J, et al. Optimal biological dose: a systematic review in cancer phase I clinical trials. BMC Cancer. 2021;21(1):60.
Muldoon LL, et al. Delayed administration of sodium thiosulfate in animal models reduces platinum ototoxicity without reduction of antitumor activity. Clin Cancer Res. 2000;6(1):309–15.
Muldoon LL, et al. N-acetylcysteine chemoprotection without decreased cisplatin antitumor efficacy in pediatric tumor models. J Neurooncol. 2015;121(3):433–40.
Wang X, et al. Dose-dependent sustained release of dexamethasone in inner ear cochlear fluids using a novel local delivery approach. Audiol Neurootol. 2009;14(6):393–401.
Al Shoyaib A, Archie SR, Karamyan VT. Intraperitoneal route of drug administration: should it be used in experimental animal studies? Pharm Res. 2019;37(1):12.
Harned TM, et al. Sodium thiosulfate administered six hours after cisplatin does not compromise antineuroblastoma activity. Clin Cancer Res. 2008;14(2):533–40.
Neuwelt EA, et al. Bone marrow chemoprotection without compromise of chemotherapy efficacy in a rat brain tumor model. J Pharmacol Exp Ther. 2004;309(2):594–9.
Dickey DT, et al. Protection against cisplatin-induced toxicities by N-acetylcysteine and sodium thiosulfate as assessed at the molecular, cellular, and in vivo levels. J Pharmacol Exp Ther. 2005;314(3):1052–8.
Juhn SK, Rybak LP, Prado S. Nature of blood-labyrinth barrier in experimental conditions. Ann Otol Rhinol Laryngol. 1981;90(2 Pt 1):135–41.
Gersten BK, et al. Ototoxicity and platinum uptake following cyclic administration of platinum-based chemotherapeutic agents. J Assoc Res Otolaryngol. 2020;21(4):303–21.
Viglietta V, et al. Phase 1 study to evaluate safety, tolerability and pharmacokinetics of a novel intra-tympanic administered thiosulfate to prevent cisplatin-induced hearing loss in cancer patients. Invest New Drugs. 2020;38(5):1463–71.
Prykhozhij SV, Caceres L, Berman JN. New developments in CRISPR/Cas-based functional genomics and their implications for research using zebrafish. Curr Gene Ther. 2017;17(4):286–300.
Wertman JN, et al. The identification of dual protective agents against cisplatin-induced oto- and nephrotoxicity using the zebrafish model. Elife. 2020;9.
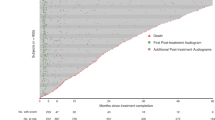
Freyer DR, et al. Effects of sodium thiosulfate versus observation on development of cisplatin-induced hearing loss in children with cancer (ACCL0431): a multicentre, randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2017;18(1):63–74.
Brock PR, et al. Sodium thiosulfate for protection from cisplatin-induced hearing loss. N Engl J Med. 2018;378(25):2376–85.
Minasian LM, et al. Prevention of cisplatin-induced hearing loss in children: informing the design of future clinical trials. Cancer Med. 2018.
Freyer DR, et al. Prevention of cisplatin-induced ototoxicity in children and adolescents with cancer: a clinical practice guideline. Lancet Child Adolesc Health. 2020;4(2):141–50.
FDA approves sodium thiosulfate to reduce the risk of ototoxicity associated with cisplatin in pediatric patients with localized, non-metastatic solid tumors. 2022 [updated September 20, 2022.
Schroeder RJ 2nd, et al. Pharmacokinetics of sodium thiosulfate in Guinea pig perilymph following middle ear application. J Otol. 2018;13(2):54–8.
Fernandez R, et al. The sustained-exposure dexamethasone formulation OTO-104 offers effective protection against cisplatin-induced hearing loss. Audiol Neurootol. 2016;21(1):22–9.
Berglin CE, et al. Prevention of cisplatin-induced hearing loss by administration of a thiosulfate-containing gel to the middle ear in a guinea pig model. Cancer Chemother Pharmacol. 2011;68(6):1547–56.
Freyer DR, et al. Interventions for cisplatin-induced hearing loss in children and adolescents with cancer. Lancet Child Adolesc Health. 2019;3(8):578–84.
Edmunds AL. Otiprio: an FDA-approved ciprofloxacin suspension gel for pediatric otitis media with effusion. P T. 2017;42(5):307–11.
Freyer DR DD, Orgel E et al. . Intratympanic injection of sustained-exposure dexamethasone thermosensitive gel (OTO-104) for prevention of cisplatin-induced hearing loss in children is feasible and safe. 2022(SIOP 2022 Annual Meeting Abstract 1172).
Neuwelt EA, Brock P. Critical need for international consensus on ototoxicity assessment criteria. J Clin Oncol. 2010;28(10):1630–2.
Meijer AJM, et al. Recommendations for age-appropriate testing, timing, and frequency of audiologic monitoring during childhood cancer treatment: an International Society of Paediatric Oncology Supportive Care Consensus Report. JAMA Oncol. 2021;7(10):1550–8.
Beahan N, et al. High-frequency pure-tone audiometry in children: a test-retest reliability study relative to ototoxic criteria. Ear Hear. 2012;33(1):104–11.
Reuter W, et al. Extended high frequency audiometry in pre-school children. Audiology. 1998;37(5):285–94.
Knight KR, et al. Early changes in auditory function as a result of platinum chemotherapy: use of extended high-frequency audiometry and evoked distortion product otoacoustic emissions. J Clin Oncol. 2007;25(10):1190–5.
Abujamra AL, et al. The use of high-frequency audiometry increases the diagnosis of asymptomatic hearing loss in pediatric patients treated with cisplatin-based chemotherapy. Pediatr Blood Cancer. 2013;60(3):474–8.
Knight KR, et al. Group-wide, prospective study of ototoxicity assessment in children receiving cisplatin chemotherapy (ACCL05C1): a report from the Children’s Oncology Group. J Clin Oncol. 2017;35(4):440–5.
Guidelines for the audiologic management of individuals receiving cochleotoxic drug therapy 1994 [Available from: https://www.asha.org/policy/gl1994-00003/.
Common Terminology Criteria for Adverse Events (CTCAE) 2017 [updated November 27, 2017. 5.0:[Available from: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/ctcae_v5_quick_reference_5x7.pdf.
Brock PR, et al. Cisplatin ototoxicity in children: a practical grading system. Med Pediatr Oncol. 1991;19(4):295–300.
Chang KW, Chinosornvatana N. Practical grading system for evaluating cisplatin ototoxicity in children. J Clin Oncol. 2010;28(10):1788–95.
King KA, Brewer CC. Clinical trials, ototoxicity grading scales and the audiologist’s role in therapeutic decision making. Int J Audiol. 2018;57(sup4):S89–98.
Schmidt CM, et al. The “Muenster classification” of high frequency hearing loss following cisplatin chemotherapy. HNO. 2007;55(4):299–306.
Gans RE, Rauterkus G, Research A. Vestibular toxicity: causes, evaluation protocols, intervention, and management. Semin Hear. 2019;40(2):144–53.
Camet ML, et al. Determining the prevalence of vestibular screening failures in pediatric cancer patients whose therapies include radiation to the head/neck and platin-based therapies: a pilot study. Pediatr Blood Cancer. 2018;65(6):e26992.
Rosenberg AR. We cannot change what we cannot see: a rationale for patient-reported outcomes in pediatric oncology clinical research. J Clin Oncol. 2022;40(15):1601–3.
Katzenstein HM, et al. Minimal adjuvant chemotherapy for children with hepatoblastoma resected at diagnosis (AHEP0731): a Children’s Oncology Group, multicentre, phase 3 trial. Lancet Oncol. 2019;20(5):719–27.
McCoy CE. Understanding the use of composite endpoints in clinical trials. West J Emerg Med. 2018;19(4):631–4.
Kuss O, McLerran D. A note on the estimation of the multinomial logistic model with correlated responses in SAS. Comput Methods Programs Biomed. 2007;87(3):262–9.
Cousins RPC. Medicines discovery for auditory disorders: challenges for industry. J Acoust Soc Am. 2019;146(5):3652.
Funding
Partial funding for this work is reported by EO (1K23DC014291 from NIH/NIDCD).
Author information
Authors and Affiliations
Contributions
The manuscript was conceptualized by DRF. The original draft manuscript was written by DRF with sections contributed by EO (translational considerations) and KK (measurement of ototoxicity). Critical review and editing of the manuscript was done by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Freyer, D.R., Orgel, E., Knight, K. et al. Special considerations in the design and implementation of pediatric otoprotection trials. J Cancer Surviv 17, 4–16 (2023). https://doi.org/10.1007/s11764-022-01312-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-022-01312-x