Abstract
Purpose
To assess healthcare costs and utilization of treatment-related pain among breast cancer survivors.
Methods
A retrospective matched cohort study using Surveillance Epidemiology and End Results SEER-Medicare linked data was conducted. The study population included older breast cancer survivors continuously enrolled in Medicare parts A, B, and D in the baseline and 1-year follow-up periods. Survivors with pain were matched to survivors without pain using PSM. Incremental all-cause healthcare costs associated with pain were calculated using a two-part model. Incremental healthcare utilization of inpatient hospitalizations, ER, outpatient, and physician services were estimated using the negative binomial model.
Results
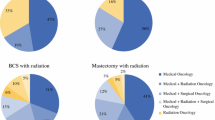
The study included 101,120 non-metastatic breast cancer patients between July 2007 and September 2013. The final analytical cohort after matching included 5891 survivors in both groups. The incremental annual all-cause total healthcare costs per patient were higher in survivors with pain as compared to survivors without pain (Δ = 4379.00 (95% CI: 4308.00–4448.80). The main cost drivers were hospitalizations at 71%, followed by ER at 16% and physician services at 9% for survivors diagnosed with pain. Annual all-cause healthcare resource utilization was also found to be higher in survivors with pain as compared to survivors without pain across all categories of use. Similar trends were observed when stratified by surgery type and subgrouped by pain type and pain-related costs.
Conclusion
This study provided baseline data that can be used for future cost-effectiveness analysis studies and burden of illness studies.
Implication for Cancer Survivors
Treatment-related costs have a substantial burden on healthcare costs and the utilization of Medicare.


Similar content being viewed by others
References
Breast cancer: the facts | McLaren Health Care Blog. https://www.mclaren.org/main/blog/breast-cancer-the-facts-1324. Accessed November 23, 2020.
Guy GP, Ekwueme DU, Yabroff KR, et al. Economic burden of cancer survivorship among adults in the United States. J Clin Oncol. 2013;31(30):3749–57. https://doi.org/10.1200/JCO.2013.49.1241.
Financial burden of cancer care | cancer trends progress report. https://progressreport.cancer.gov/after/economic_burden. Accessed September 21, 2020.
Park J, Look KA. Health care expenditure burden of cancer care in the United States. Inq J Heal Care Organ Provision, Financ. 56:1–9. doi:https://doi.org/10.1177/0046958019880696
Scott Baker K, Broderick G, Demark-Wahnefried W, et al. NCCN guidelines version 2.2020 survivorship NCCN guidelines panel disclosures.; 2020.
Dean LT, Moss SL, Rollinson SI, Frasso Jaramillo L, Paxton RJ, Owczarzak JT. Patient recommendations for reducing long-lasting economic burden after breast cancer. Cancer. 2019;125(11):1929–40. https://doi.org/10.1002/cncr.32012.
Dean LT, Moss SL, Ransome Y, et al. BIt still affects our economic situation: long-term economic burden of breast cancer and lymphedema. Support Care Cancer. 2019;27:1697–708. https://doi.org/10.1007/s00520-018-4418-4.
Dean LT, Ransome Y, Frasso-Jaramillo L, et al. Drivers of cost differences between US breast cancer survivors with or without lymphedema. J Cancer Surviv. 2019;13(5):804–14. https://doi.org/10.1007/s11764-019-00799-1.
Cheville A, Lee M, Moynihan T, et al. The impact of arm lymphedema on healthcare utilization during long-term breast cancer survivorship: a population-based cohort study. J Cancer Surviv. 2020;14(3):347–55. https://doi.org/10.1007/s11764-019-00851-0.
Shih YCT, Xu Y, Cormier JN, et al. Incidence, treatment costs, and complications of lymphedema after breast cancer among women of working age: a 2-year follow-up study. J Clin Oncol. 2009;27(12):2007–14. https://doi.org/10.1200/JCO.2008.18.3517.
Glare PA, Davies PS, Finlay E, et al. Pain in cancer survivors. J Clin Oncol. 2014;32(16):1739–47. https://doi.org/10.1200/JCO.2013.52.4629.
Goucke CR. Essentials of Interventional Cancer Pain Management, 1st Ed.; 2019. https://doi.org/10.1213/ane.0000000000004450
Brown M, Farquhar-Smith P. Pain in cancer survivors; filling in the gaps. Br J Anaesth. 2017;119(4):723–36. https://doi.org/10.1093/bja/aex202.
Mariotto AB, Enewold L, Zhao J, Zeruto CA, Yabroff KR. Medical care costs associated with cancer survivorship in the United States. Cancer Epidemiol Biomarkers Prev. 2020;29(7):1304–12. https://doi.org/10.1158/1055-9965.EPI-19-1534.
STATISTICAL BRIEF #331: Top 10 most costly conditions among men and women, 2008: estimates for the U.S. Civilian noninstitutionalized adult population, age 18 and older. https://meps.ahrq.gov/data_files/publications/st331/stat331.shtml. Accessed 3 Sept 2020.
Overview of the SEER Program. https://seer.cancer.gov/about/overview.html. Accessed 5 Sept 2020.
Overview of the SEER Program. https://seer.cancer.gov/about/overview.html. Accessed 15 Feb 2022.
Nih, Nci, DCCPS. Surveillance, Epidemiology, and End Results (SEER). https://seer.cancer.gov. Accessed 5 May 2020.
Barbash RB, Brown M, Ph D, Warren J, Ph D. Overview of the SEER ‐ Medicare data what are the SEER ‐ Medicare data? 2009.
Brief description of SEER-Medicare database. https://healthcaredelivery.cancer.gov/seermedicare/overview/. Accessed 18 May 2020.
Nattinger AB, Laud PW, Bajorunaite R, Sparapani RA, Freeman JL. An algorithm for the use of medicare claims data to identify women with incident breast cancer. Health Serv Res. 2004;39(6 I):1733–50. https://doi.org/10.1111/j.1475-6773.2004.00315.x.
Boero IJ, Paravati AJ, Triplett DP, et al. The impact of radiotherapy costs on clinical outcomes in breast cancer. Radiother Oncol. 2015;117(2):393–9. https://doi.org/10.1016/j.radonc.2015.10.004.
Smith BD, Jiang J, Shih YC, et al. Cost and complications of local therapies for early-stage breast cancer. J Natl Cancer Inst. 2017;109(1). https://doi.org/10.1093/jnci/djw178
National Drug Code Directory. https://www.accessdata.fda.gov/scripts/cder/ndc/index.cfm. Accessed 10 Sept 2020.
CMS’ ICD-9-CM to and from ICD-10-CM and ICD-10-PCS crosswalk or general equivalence mappings. http://data.nber.org/data/icd9-icd-10-cm-and-pcs-crosswalk-general-equivalence-mapping.html. Accessed 9 Sept 2020.
Blumen H, Fitch K, Polkus V. Comparison of treatment costs for breast cancer, by tumor stage and type of service. Am Heal Drug Benefits. 2016;9(1):23–31.
Reiner AS, Jacks LM, Van Zee KJ, Panageas KS. A SEER-medicare population-based study of lymphedema-related claims incidence following breast cancer in men. Breast Cancer Res Treat. 2011;130(1):301–6. https://doi.org/10.1007/s10549-011-1649-1.
(No Title). https://www.wellstar.org/about-us/icd-10/documents/topdiagnosiscodes(crosswalks)all.pdf. Accessed 29 March 2020.
Staats PS. Atlas of uncommon pain syndromes. Anesthesiology. 2003;99(2):518. https://doi.org/10.1097/00000542-200308000-00050.
Atlas of common pain syndromes E-Book - Steven D. Waldman - Google Books. https://books.google.com/books?id=y794gKjfZGUC&pg=PA68&lpg=PA68&dq=radiation+induced+brachial+plexopathy+diagnosis+code&source=bl&ots=TjpjAeOcM_&sig=ACfU3U0WOIXhKaY0O7S-rolk9A6TRpl9sA&hl=en&sa=X&ved=2ahUKEwjn1uSkm6_oAhUR1qwKHdJlBrM4ChDoATABegQICxAB#v=onepage&q=radiationinducedbrachialplexopathydiagnosiscode&f=false. Accessed 22 March 2020.
COMPLETE LIST OF ICD-10-CM Medical Diagnosis Codes.
Manchikanti L, Hammer MJ, Boswell M V, Kaye AD, Hirsch JA. Health Policy Review A Seamless navigation to ICD-10-CM for interventional pain physicians: is a rude awakening avoidable? 2015. www.painphysicianjournal.com. Accessed 22 March 2020.
Richardson LC, Royalty J, Howe W, Helsel W, Kammerer W, Benard VB. Timeliness of breast cancer diagnosis and initiation of treatment in the National Breast and Cervical Cancer Early Detection Program, 1996–2005. Am J Public Health. 2010;100(9):1769–76. https://doi.org/10.2105/AJPH.2009.160184.
You’ve been diagnosed with breast cancer. How soon do you need treatment? – Science-Based Medicine. https://sciencebasedmedicine.org/you-have-breast-cancer-how-soon-do-you-need-treatment/. Accessed 12 Oct 2020.
Chavez-MacGregor M, Clarke CA, Lichtensztajn DY, Giordano SH. Delayed initiation of adjuvant chemotherapy among patients with breast cancer. JAMA Oncol. 2016;2(3):322–9. https://doi.org/10.1001/jamaoncol.2015.3856.
Warren JL, Mariotto A, Melbert D, et al. Sensitivity of medicare claims to identify cancer recurrence in elderly colorectal and breast cancer patients. https://doi.org/10.1097/MLR.0000000000000058
Komen perspectives - what can I expect? late effects of breast cancer treatment (August 2012) | Susan G. Komen®. https://ww5.komen.org/KomenPerspectives/Komen-Perspectives---What-can-I-expect--Late-effects-of-breast-cancer-treatment-(August-2012).html. Accessed 16 Oct 2020.
Coping with long term side effects of treatment. https://www.breastcancerfoundation.org.nz/support/moving-forward-after-treatment/coping-with-long-term-side-effects-of-treatment. Accessed 16 Oct 2020.
Breast reconstruction after mastectomy - National Cancer Institute. https://www.cancer.gov/types/breast/reconstruction-fact-sheet. Accessed 18 Jan 2022.
Greenwald MK, Ruterbusch JJ, Beebe-Dimmer JL, Simon MS, Albrecht TL, Schwartz AG. Risk of incident claims for chemotherapy-induced peripheral neuropathy among women with breast cancer in a medicare population. Cancer. 2019;125(2):269–77. https://doi.org/10.1002/cncr.31798.
Parsons LS. Performing a 1:N case-control match on propensity score.
(DOC) A SAS macro for calculating standardized differences of means and proportions | Joe Caswell - Academia.edu. https://www.academia.edu/37917760/A_SAS_Macro_for_Calculating_Standardized_Differences_of_Means_and_Proportions. Accessed 11 March 2022.
Seal KH, Shi Y, Cohen G, et al. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA - J Am Med Assoc. 2012;307(9):940–7. https://doi.org/10.1001/jama.2012.234.
Desai R, Camacho F, Tan X, LeBaron V, Blackhall L, Balkrishnan R. Mental health comorbidities and elevated risk of opioid use in elderly breast cancer survivors using adjuvant endocrine treatments. J Oncol Pract. 2019;15(9):e777–86. https://doi.org/10.1200/jop.18.00781.
Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53(12):1258–67. https://doi.org/10.1016/S0895-4356(00)00256-0.
Martin BC, Ganguly R, Pannicker S, Frech F, Barghout V. Utilization patterns and net direct medical cost to Medicaid of irritable bowel syndrome. Curr Med Res Opin. 2003;19:771–80. https://doi.org/10.1185/030079903125002540.
Kenzik KM, Williams GR, Bhakta N, et al. Healthcare utilization and spending among older patients diagnosed with non-Hodgkin lymphoma. J Geriatr Oncol. 2021;12(8):1225–32. https://doi.org/10.1016/J.JGO.2021.06.006.
How to identify hospital claims for emergency room visits in the Medicare claims data | ResDAC. https://resdac.org/articles/how-identify-hospital-claims-emergency-room-visits-medicare-claims-data. Accessed 22 Feb 2022.
Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20(4):461–94. https://doi.org/10.1016/S0167-6296(01)00086-8.
Kapitula LR. When two are better than one: fitting two-part models using SAS ®. 3600–2015.
Subramanian S, Trogdon J, Ekwueme DU, Gardner JG, Whitmire JT, Rao C. Cost of cervical cancer treatment: implications for providing coverage to low-income women under the Medicaid expansion for cancer care. Women’s Heal Issues. 2010;20(6):400–5. https://doi.org/10.1016/J.WHI.2010.07.002.
Jutkowitz E, Kane RL, Dowd B, Gaugler JE, MacLehose RF, Kuntz KM. Effects of cognition, function, and behavioral and psychological symptoms on Medicare expenditures and health care utilization for persons with dementia. J Gerontol A Biol Sci Med Sci. 2017;72(6):818–24. https://doi.org/10.1093/gerona/glx035.
Buntin MB, Zaslavsky AM. Too much ado about two-part models and transformation? comparing methods of modeling Medicare expenditures. J Health Econ. 2004;23(3):525–42. https://doi.org/10.1016/j.jhealeco.2003.10.005.
12 Additional GLM topics | Exam PA Study Guide, Spring 2022. https://sdcastillo.github.io/PA-R-Study-Manual/additional-glm-topics.html. Accessed 21 March 2022.
Kale HP, Kale HP, Carroll N V. Economic burden of renal cell carcinoma (RCC) and treatment economic burden of renal cell carcinoma (RCC) and treatment patterns, overall survival and healthcare costs among older patterns, overall survival and healthcare costs among older metastatic RCC patients metastatic RCC patients downloaded from downloaded from economic burden of renal cell carcinoma (RCC) and treatment patterns, overall survival and healthcare costs among older metastatic RCC patients. 2018. https://scholarscompass.vcu.edu/etd/5555. Accessed 2 Nov 2020.
BLS Data Viewer. https://beta.bls.gov/dataViewer/view/timeseries/CUSR0000SAM2. Accessed 22 Feb 2022.
Ismail N, Zamani H. Estimation of claim count data using negative binomial, generalized poisson, zero-inflated negative binomial and zero-inflated generalized poisson regression models.
SAS/STAT Fitting zero-inflated count data models by using PROC GENMOD. https://support.sas.com/rnd/app/stat/examples/GENMODZIP/roots.htm. Accessed 23 Feb 2022.
Moon S, Shin J. Health care utilization among Medicare-Medicaid dual eligibles: a count data analysis. BMC Public Health. 2006;6(1):1–10. https://doi.org/10.1186/1471-2458-6-88/TABLES/3.
Mullahy J. Specification and testing of some modified count data models. J Econom. 1986;33(3):341–65. https://doi.org/10.1016/0304-4076(86)90002-3.
Female breast cancer — cancer stat facts. https://seer.cancer.gov/statfacts/html/breast.html. Accessed 13 Aug 2020.
Narod SA, Iqbal J, Miller AB. Why have breast cancer mortality rates declined? J Cancer Policy. 2015;5:8–17. https://doi.org/10.1016/J.JCPO.2015.03.002.
Mariotto AB, Enewold L, Zhao J, Zeruto CA, Yabroff KR. Medical care costs associated with cancer survivorship in the United States. Cancer Epidemiol Biomarkers Prev. 2020;1–10. https://doi.org/10.1158/1055-9965.epi-19-1534
Arondekar B, Curkendall SM, Monberg M, et al. Economic burden associated with adverse events in patients with metastatic melanoma. Value Heal. 2013;16(3):A137. https://doi.org/10.1016/J.JVAL.2013.03.667.
Halpern MT, de Moor JS, Yabroff KR. Impact of pain on employment and financial outcomes among cancer survivors. J Clin Oncol. 2022;40(1):24–31. https://doi.org/10.1200/JCO.20.03746.
Latremouille-Viau D, Chang J, Guerin A, et al. The economic burden of common adverse events associated with metastatic colorectal cancer treatment in the United States. J Med Econ. 2017;20(1):54–62. https://doi.org/10.1080/13696998.2016.1225577.
Zhang X, Liu S, Liu Y, et al. Economic burden for lung cancer survivors in urban China. Int J Environ Res Public Health. 2017;14(3):308. https://doi.org/10.3390/IJERPH14030308.
Rose MI. 1 nerve decompression for chemotherapy-induced neuropathic pain.
Lymphedema: What are your surgical options? | Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/lymphedema-what-are-your-surgical-options. Accessed 3 May 2022.
De Oliveira AJM, Castro JP de S, Foroni LH, Siqueira MG, Martins RS. Treatment of radiation-induced brachial plexopathy with omentoplasty. Autops Case Reports. 2020;10(3). https://doi.org/10.4322/ACR.2020.202
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424. https://doi.org/10.1080/00273171.2011.568786.
Acknowledgements
The authors would like to thank Mr. Adrian Jemal Williams for providing technical assistance, proofreading, finalizing, and submitting this manuscript.
Funding
This manuscript did not receive any specific funding and all authors declare that they have no conflicts of interest. Dr. Li is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1 TR003107-02S2. Support of data acquisition has been provided in part by the Arkansas Biosciences Institute, the major research component of the Arkansas Tobacco Settlement Proceeds Act of 2000. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, National Cancer Institute, or Arkansas Biosciences Institute.
Author information
Authors and Affiliations
Contributions
All authors were involved in the development of the study concepts and manuscript review. Lakkad and Painter were both responsible for the development of the study design, quality control involving data, and manuscript preparation. Lakkad was responsible for data and statistical analysis as well as manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lakkad, M., Martin, B., Li, C. et al. Healthcare costs and utilization associated with pain among breast cancer survivors: a propensity score matched cohort study using SEER-Medicare data. J Cancer Surviv 17, 917–950 (2023). https://doi.org/10.1007/s11764-022-01282-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-022-01282-0