Abstract
Purpose
To investigate whether health literacy (HL) among informal caregivers of breast cancer (BC) survivors is associated with patient psychological outcomes.
Methods
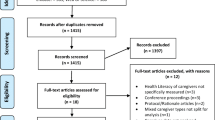
We used data (n = 340 pairs) from baseline questionnaires administered in the MyHealth trial investigating nurse-led BC follow-up. All BC survivors and their invited caregivers were included immediately after completion of primary treatment. We performed multivariate regression analyses to examine the association between caregiver HL (nine dimensions as measured by the Health Literacy Questionnaire) as exposure and patient depression, anxiety, and health-related quality of life (HQoL) as outcomes. We further examined whether any association differed according to type of caregiver, patient HL, and patient activation (skill in managing one’s health).
Results
Three dimensions, “ability to engage with providers” (β = − 0.2), “navigating the system” (β = − 0.2), and “understand health information” (β = − 0.2), were significantly associated with lower patient depression (p < 0.05), while four dimensions, “having sufficient information” (β = 0.3), “navigating the system” (β = 0.2), “find health information” (β = 0.2), and “understand health information” (β = 0.2), were significantly associated with better patient HQoL (p < 0.05). No significant associations were found for anxiety. Patient HL and activation did not significantly modify the associations, while certain associations for depression were stronger in patients with non-partner caregivers.
Conclusions
The HL of informal caregivers may play an important role in optimizing psychological outcomes in cancer survivors.
Implications for Cancer Survivors
Involving informal caregivers, who can provide support related to health information and services, may be beneficial for the psychological well-being of cancer survivors.

Similar content being viewed by others
References
Bevan JL, Pecchioni LL. Understanding the impact of family caregiver cancer literacy on patient health outcomes. Patient Educ Couns. 2008;71(3):356–64. https://doi.org/10.1016/j.pec.2008.02.022.
Buchbinder R, Batterham R, Ciciriello S, Newman S, Horgan B, Ueffing E, et al. Health literacy: what is it and why is it important to measure? J Rheumatol. 2011;38:1791–7. https://doi.org/10.3899/jrheum.110406.
Osborne RH, Batterham RW, Elsworth GR, Hawkins M, Buchbinder R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health. 2013;13(1):1–17. https://doi.org/10.1186/1471-2458-13-658.
Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. https://doi.org/10.7326/0003-4819-155-2-201107190-00005.
Husson O, Mols F, Fransen MP, van de Poll-Franse LV, Ezendam NPM. Low subjective health literacy is associated with adverse health behaviors and worse health-related quality of life among colorectal cancer survivors: results from the profiles registry. Psychooncology. 2015;24(4):478–86. https://doi.org/10.1002/pon.3678.
Kugbey N, Meyer-Weitz A, Oppong AK. Access to health information, health literacy and health-related quality of life among women living with breast cancer: depression and anxiety as mediators. Patient Educ Couns. 2019;102(7):1357–63. https://doi.org/10.1016/j.pec.2019.02.014.
Goodwin BC, March S, Zajdlewicz L, Osborne RH, Dunn J, Chambers SK. Health literacy and the health status of men with prostate cancer. Psychooncology. 2018;27(10):2374–81. https://doi.org/10.1002/pon.4834.
Halverson JL, Martinez-Donate AP, Palta M, Leal T, Lubner S, Walsh MC, et al. Health literacy and health-related quality of life among a population-based sample of cancer patients. J Health Commun. 2015;20(11):1320–9. https://doi.org/10.1080/10810730.2015.1018638.
Song L, Mishel M, Bensen JT, Chen RC, Knafl GJ, Blackard B, et al. How does health literacy affect quality of life among men with newly diagnosed clinically localized prostate cancer? Findings from the North Carolina-Louisiana Prostate Cancer Project (PCaP). Cancer. 2012;118(15):3842–51. https://doi.org/10.1002/cncr.26713.
Plummer LC, Chalmers KA. Health literacy and physical activity in women diagnosed with breast cancer. Psychooncology. 2017;26(10):1478–83. https://doi.org/10.1002/pon.4318.
Mitchell AJ, Ferguson DW, Gill J, Paul J, Symonds P. Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: a systematic review and meta-analysis. Lancet Oncol. 2013;14(8):721–32. https://doi.org/10.1016/S1470-2045(13)70244-4.
Pitman A, Suleman S, Hyde N, Hodgkiss A. Depression and anxiety in patients with cancer. BMJ. 2018;361:k1415. https://doi.org/10.1136/bmj.k1415.
Suppli NP, Johansen C, Kessing LV, Toender A, Kroman N, Ewertz M, et al. Survival after early-stage breast cancer of women previously treated for depression: a nationwide Danish cohort study. J Clin Oncol. 2016;35(3):334–42. https://doi.org/10.1200/JCO.2016.68.8358.
Hartung TJ, Brähler E, Faller H, Härter M, Hinz A, Johansen C, et al. The risk of being depressed is significantly higher in cancer patients than in the general population: prevalence and severity of depressive symptoms across major cancer types. Eur J Cancer. 2017;72:46–53. https://doi.org/10.1016/j.ejca.2016.11.017.
Suppli NP, Johansen C, Christensen J, Kessing LV, Kroman N, Dalton SO. Increased risk for depression after breast cancer: a nationwide population-based cohort study of associated factors in Denmark, 1998-2011. J Clin Oncol. 2014;32(34):3831–9. https://doi.org/10.1200/JCO.2013.54.0419.
Kent EE, Rowland JH, Northouse L, Litzelman K, Chou W-YS, Shelburne N, et al. Caring for caregivers and patients: research and clinical priorities for informal cancer caregiving. Cancer. 2016;122(13):1987–95. https://doi.org/10.1002/cncr.29939.
Rottmann N, Hansen DG, Larsen PV, Nicolaisen A, Flyger H, Johansen C, et al. Dyadic coping within couples dealing with breast cancer: a longitudinal, population-based study. Health Psychol. 2015;34(5):486–95. https://doi.org/10.1037/hea0000218.
Regan TW, Lambert SD, Kelly B, McElduff P, Girgis A, Kayser K, et al. Cross-sectional relationships between dyadic coping and anxiety, depression, and relationship satisfaction for patients with prostate cancer and their spouses. Patient Educ Couns. 2014;96(1):120–7. https://doi.org/10.1016/j.pec.2014.04.010.
Maass SWMC, Roorda C, Berendsen AJ, Verhaak PFM, de Bock GH. The prevalence of long-term symptoms of depression and anxiety after breast cancer treatment: a systematic review. Maturitas. 2015;82(1):100–8. https://doi.org/10.1016/j.maturitas.2015.04.010.
Niedzwiedz CL, Knifton L, Robb KA, Katikireddi SV, Smith DJ. Depression and anxiety among people living with and beyond cancer: a growing clinical and research priority. BMC Cancer. 2019;19(1):943. https://doi.org/10.1186/s12885-019-6181-4.
Danckert B, Ferlay J, Engholm G, Hansen H, Johannesen T, Khan S et al. NORDCAN: cancer incidence, mortality, prevalence and survival in the Nordic countries. Association of the Nordic Cancer Registries. Danish Cancer Society. 2019. http://www-dep.iarc.fr/NORDCAN/english/frame.asp. Accessed 20 January 2020.
Cancer Research UK. Worldwide cancer statistics. 2019. https://www.cancerresearchuk.org/health-professional/cancer-statistics/worldwide-cancer. .
Yuen EYN, Knight T, Ricciardelli LA, Burney S. Health literacy of caregivers of adult care recipients: a systematic scoping review. Health Soc Care Community. 2018;26(2):e191–206. https://doi.org/10.1111/hsc.12368.
Yuen EYN, Dodson S, Batterham RW, Knight T, Chirgwin J, Livingston PM. Development of a conceptual model of cancer caregiver health literacy. Eur J Cancer Care. 2016;25(2):294–306. https://doi.org/10.1111/ecc.12284.
Bevans M, Sternberg EM. Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. JAMA. 2012;307(4):398–403. https://doi.org/10.1001/jama.2012.29.
Levin JB, Peterson PN, Dolansky MA, Boxer RS. Health literacy and heart failure management in patient-caregiver dyads. J Card Fail. 2014;20(10):755–61. https://doi.org/10.1016/j.cardfail.2014.07.009.
Rahman TTA. Health literacy: Prevalence among elderly care givers and its impact on the frequency of elderly hospitalization and elderly health-related quality of life. Adv Aging Res. 2014;3(5):380–7.
Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 Pt 1):1005–26. https://doi.org/10.1111/j.1475-6773.2004.00269.x.
Saltbaek L, Karlsen RV, Bidstrup PE, Hoeg BL, Zoffmann V, Horsbol TA, et al. MyHealth: specialist nurse-led follow-up in breast cancer. A randomized controlled trial - development and feasibility. Acta Oncol. 2019;58:1–8. https://doi.org/10.1080/0284186x.2018.1563717.
ClinicalTrials.gov. MyHealth: Follow-up After Breast Cancer Treatment (MyHealth). 2016. https://clinicaltrials.gov/ct2/show/NCT02949167. Accessed 1 Sept 2019.
Maindal HT, Kayser L, Norgaard O, Bo A, Elsworth GR, Osborne RH. Cultural adaptation and validation of the Health Literacy Questionnaire (HLQ): robust nine-dimension Danish language confirmatory factor model. SpringerPlus. 2016;5(1):1232. https://doi.org/10.1186/s40064-016-2887-9.
Brady MJ, Cella DF, Mo F, Bonomi AE, Tulsky DS, Lloyd SR, et al. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J Clin Oncol. 1997;15(3):974–86. https://doi.org/10.1200/jco.1997.15.3.974.
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. https://doi.org/10.1001/archinte.166.10.1092.
Rutter LA, Brown TA. Psychometric Properties of the Generalized Anxiety Disorder Scale-7 (GAD-7) in outpatients with anxiety and mood disorders. J Psychopathol Behav Assess. 2017;39(1):140–6. https://doi.org/10.1007/s10862-016-9571-9.
Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood). 2013;32(2):207–14. https://doi.org/10.1377/hlthaff.2012.1061.
Patient Activation Measure (PAM). Insignia Health. https://www.insigniahealth.com/products/pam-survey. Accessed 1 September 2016.
Beauchamp A, Buchbinder R, Dodson S, Batterham RW, Elsworth GR, McPhee C, et al. Distribution of health literacy strengths and weaknesses across socio-demographic groups: a cross-sectional survey using the Health Literacy Questionnaire (HLQ). BMC Public Health. 2015;15:678. https://doi.org/10.1186/s12889-015-2056-z.
Bartlett JW, Seaman SR, White IR, Carpenter JR. Multiple imputation of covariates by fully conditional specification: accommodating the substantive model. Stat Methods Med Res. 2014;24(4):462–87. https://doi.org/10.1177/0962280214521348.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2019. https://www.R-project.org/.
Saltbæk L, Bidstrup PE, Karlsen RV, Høeg BL, Horsboel TA, Belmonte F et al. Nurse-led individualized follow-up versus regular physician-led visits after breast cancer (MyHealth) - a randomized controlled trial. Manuscript submitted for publication. 2020.
Goldsmith JV, Terui S. Family oncology caregivers and relational health literacy. Challenges. 2018;9(2):35.
Wittenberg E, Goldsmith J, Ferrell B, Ragan SL. Promoting improved family caregiver health literacy: evaluation of caregiver communication resources. Psychooncology. 2017;26(7):935–42. https://doi.org/10.1002/pon.4117.
Lowe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the patient health questionnaire-9. Med Care. 2004;42(12):1194–201. https://doi.org/10.1097/00005650-200412000-00006.
Fernández-González L, Bravo-Valenzuela P. Effective interventions to improve the health literacy of cancer patients. Ecancermedicalscience. 2019;13:966. https://doi.org/10.3332/ecancer.2019.966.
Yuen EY, Knight T, Dodson S, Ricciardelli L, Burney S, Livingston PM. Development of the Health Literacy of Caregivers Scale - Cancer (HLCS-C): item generation and content validity testing. BMC Fam Pract. 2014;15(1):202. https://doi.org/10.1186/s12875-014-0202-9.
Funding
The MyHealth trial was funded by the Danish Cancer Society, Region Zealand, Rigshospitalet (Copenhagen University Hospital) and the Capital Region of Denmark.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by BLH, MHF, EAWA, LS, RVK, and PEB. The first draft of the manuscript was written by BLH and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 35 kb)
Rights and permissions
About this article
Cite this article
Høeg, B.L., Frederiksen, M.H., Andersen, E.A.W. et al. Is the health literacy of informal caregivers associated with the psychological outcomes of breast cancer survivors?. J Cancer Surviv 15, 729–737 (2021). https://doi.org/10.1007/s11764-020-00964-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-020-00964-x