Abstract
Purpose
Previous studies have merely investigated oncology providers’ a priori attitudes toward SCPs. The purpose of the current study was to longitudinally evaluate oncology providers’ expectations and actual experiences with the use of an automatically generated Survivorship Care Plan (SCP) in daily clinical practice.
Methods
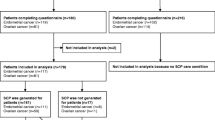
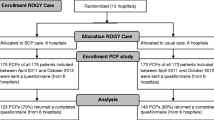
Between April 2011 and October 2012, the participating oncology providers (i.e., gynecologists, gynecologic oncologists, oncology nurses) provided usual care or SCP care to 222 endometrial and 85 ovarian cancer patients included in the Registrationsystem Oncological GYnecology (ROGY) Care trial. All (n = 43) oncology providers in both arms were requested to complete a questionnaire before and after patient inclusion regarding their expectations and evaluation of SCP care.
Results
Before patient inclusion, 38 (88 %; 21 SCP, 17 usual care), and after patient inclusion, 35 (83 %; 20 SCP, 15 usual care) oncology providers returned the questionnaire. After patient inclusion, oncology providers were generally satisfied with the SCP (M = 7.1, SD = 1.3, with 1 = not at all–10 = very much) and motivated to keep using the SCP (M = 7.9, SD = 1.5). Most providers (64 %) encountered barriers. Twenty-five percent felt they used more time for consultations (M = 7.3 min, SD = 4.6). However, self-reported consultation time did not differ between before (M = 21.8 min, SD = 11.6) and after patient inclusion (M = 18.7, SD = 10.6; p = 0.22) or between SCP care (M = 18.5, SD = 10.3) and usual care (M = 22.0, SD = 12.2; p = 0.21).
Conclusions
Oncology providers using the SCP were generally satisfied and motivated to keep using the SCP. However, the findings of the current study suggest that even when the SCP can be generated automatically, oncology providers still have difficulties with finding the time to discuss the SCP with their patients.
Implications for Cancer Survivors
If SCP care is indeed effective, overcoming the perceived barriers is needed before large-scale implementation in order for cancer survivors to fully benefit from the potential advantages of SCPs.

Similar content being viewed by others
References
Erikson C, Salsberg E, Forte G, Bruinooge S, Goldstein M. Future supply and demand for oncologists: challenges to assuring access to oncology services. J Oncol Pract. 2007;3:79–86.
Signaleringscommissie Kanker van KWF Kankerbestrijding: Kanker in Nederland tot 2020. Trends en prognoses (online attachment: www.kwfkankerbestrijding.nl/sck). 2011.
Hewitt M, Greenfield S, Stovall E. From cancer patient to cancer survivor: lost in transition. Washington, DC: National Academies Press; 2006.
Salz T, Oeffinger KC, McCabe MS, Layne TM, Bach PB. Survivorship care plans in research and practice. CA Cancer J Clin. 2012;62:101–17.
Baravelli C, Krishnasamy M, Pezaro C, Schofield P, Lotfi-Jam K, Rogers M, et al. The views of bowel cancer survivors and health care professionals regarding survivorship care plans and post treatment follow up. J Cancer Surviv. 2009;3:99–108.
Hewitt ME, Bamundo A, Day R, Harvey C. Perspectives on post-treatment cancer care: qualitative research with survivors, nurses, and physicians. J Clin Oncol. 2007;25:2270–3.
Watson EK, Sugden EM, Rose PW. Views of primary care physicians and oncologists on cancer follow-up initiatives in primary care: an online survey. J Cancer Surviv. 2010;4:159–66.
Kantsiper M, McDonald EL, Geller G, Shockney L, Snyder C, Wolff AC. Transitioning to breast cancer survivorship: perspectives of patients, cancer specialists, and primary care providers. J Gen Intern Med. 2009;24:S459–66.
Brennan ME, Butow P, Spillane J, Boyle FM. Survivorship care after breast cancer: follow-up practices of Australian health professionals and attitudes to a survivorship care plan. Asia Pac J Clin Onc. 2010;6:116–25.
Birken SA, Mayer DK, Weiner BJ. Survivorship care plans: prevalence and barriers to use. J Cancer Educ. 2013;28:290–6.
Campbell MK, Tessaro I, Gellin M, Valle CG, Golden S, Kaye L, et al. Adult cancer survivorship care: experiences from the LIVESTRONG centers of excellence network. J Cancer Surviv. 2011;5:271–82.
Ganz PA. Quality of care and cancer survivorship: the challenge of implementing the institute of medicine recommendations. J Oncol Pract. 2009;5:101–5.
Stricker CT, Jacobs LA, Risendal B, Jones A, Panzer S, Ganz PA, et al. Survivorship care planning after the institute of medicine recommendations: how are we faring? J Cancer Surviv. 2011;5:358–70.
Faul LA, Rivers B, Shibata D, Townsend I, Carbrera P, Quin GP, et al. Survivorship care planning in colorectal cancer: feedback from survivors and providers. J Psychosoc Oncol. 2012;30:198–216.
Horning SJ. Follow-up of adult cancer survivors: new paradigms for survivorship care planning. Hematol Oncol Clin North Am. 2008;22:201–10.
Earle CC. Long term care planning for cancer survivors: a health services research agenda. J Cancer Surviv. 2007;1:64–74.
Horowitz ME, Fordis M, Krause S, McKellar J, Poplack DG. Passport for care: implementing the survivorship care plan. J Oncol Pract. 2009;5:110–2.
Hill-Kayser CE, Vachani C, Hampshire MK, Jacob LA, Metz JM. An internet tool for creation of cancer survivorship care plans for survivors and health care providers: design, implementation, use, and user satisfaction. J Med Internet Res. 2009;11:e39.
van de Poll-Franse LV, Nicolaije KAH, Vos MC, Pijnenborg JM, Boll D, Husson O, et al. The impact of a cancer Survivorship Care Plan on gynecological cancer patient and health care provider reported outcomes (ROGY Care): study protocol for a pragmatic cluster randomized controlled trial. Trials. 2011;12:256.
Ganz PA, Hahn EE. Implementing a survivorship care plan for patients with breast cancer. J Clin Oncol. 2008;26:759–67.
Tuinman MA, Gazendam-Donofrio SM, Hoekstra-Weebers JEHM. Screening and referral for psychosocial distress in oncologic practice: use of the Distress Thermometer. Cancer. 2008;113:870–8.
Earle CC. Failing to plan is planning to fail: improving the quality of care with survivorship care plans. J Clin Oncol. 2006;24:5112–6.
Hahn EE, Ganz PA. Survivorship programs and care plans in practice: variations on a theme. J Oncol Pract. 2011;7:70–5.
Stricker CT, Jacobs LA, Palmer SC. Survivorship care plans: an argument for evidence over common sense. J Clin Oncol. 2012;30:1392–3.
Grunfeld E, Julian A, Pond G, Maunsell E, Coyle D, Folkes A, et al. Evaluating survivorship care plans: results of a randomized, clinical trial of patients with breast cancer. J Clin Oncol. 2011;29:4755–62.
Brothers BM, Easley A, Salani R, Andersen BL. Do survivorship care plans impact patients’ evaluations of care? A randomized evaluation with gynecologic oncology patients. Gynecol Oncol. 2013;129:554–8.
Acknowledgments
The authors would like to thank all patients and oncology providers for their participation in the study. Special thanks go to the research assistants, in particular Mrs. E. de Winter, who helped to collect the data for this study. In addition, we would like to acknowledge Dr. M. van Bommel, who was willing to function as an independent advisor and to answer patients’ questions. We would like to thank the following hospitals and institutions for their cooperation: Amphia Hospital, Breda and Oosterhout; Catharina Hospital, Eindhoven; Elkerliek Hospital, Helmond; Jeroen Bosch Hospital,’s-Hertogenbosch; Institute Verbeeten, Tilburg; Maastricht University Medical Center, Maastricht; Maxima Medical Center, Eindhoven and Veldhoven; Orbis Medical Center, Sittard; St. Anna Hospital, Geldrop and Eindhoven; St. Elisabeth Hospital, Tilburg; St. Jans Hospital, Weert; TweeSteden Hospital, Tilburg and Waalwijk; and VieCuri Hospital, Venlo and Venray. The ROGY Care trial is supported with grant no. UVT 2010-4743 from the Dutch Cancer Society. Prof. Dr. Lonneke van de Poll-Franse is supported by a Cancer Research Award from the Dutch Cancer Society (#UVT-2009-4349).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Questionnaires oncology providers
-
1.
In which hospital are you employed? (CG + IG; BI + AI): OPEN ENDED
-
2.
What is your profession? (CG + IG; BI + AI): Gynecologist/GO/(Oncology) nurse/Nurse practitioner/Other, namely…
-
3.
Gender (CG + IG; BI + AI): Male/Female
-
4.
Age (CG + IG; BI + AI): … years
-
5.
How do you currently provide information to your patients? More than one answer possible (CG + IG; BI + AI): SCP1/Verbally/Brochure Dutch Cancer Society/Other brochure/Referral to website/CD-ROM/Other, namely…
-
6.
How satisfied are you with the information you currently provide to your patients? (CG + IG; BI + AI) : Not at all (1)–Very much (10)
-
7.
How do you currently screen for psychosocial distress? More than one answer possible (CG + IG; BI + AI): Screening instrument, namely…/I do not screen for psychosocial distress/Other, namely…
-
8.
How long does an average consultation take you currently? (CG + IG; BI + AI): … minutes
-
9.
Do you expect to need more time for your consultations because of the SCP? (IG; BI): No/Yes, approximately … minutes more time
-
10.
To what extent do you expect the SCP to affect the patient positively? (IG; BI): Not at all (1)–Very much (10)
-
11.
How motivated are you to start using the SCP? (IG; BI): Not at all (1)–Very much (10)
-
12.
Were you a provider of SCPs in your hospital? (IG; AI): Yes, always (continue with question 13)/Yes, most of the time (continue with question 13)/Yes, sometimes (continue with question 13)/No (continue with question 28)
-
13.
What do you think about the amount of information in the SCP? (IG; AI): Much too little (1)–Much too much (10)
-
14.
Did you miss information in the SCP? (IG; AI): No/Yes, namely…
-
15.
Would you prefer not to have certain information in the SCP? (IG; AI): No/Yes, namely…
-
16.
To what extent do you think the SCP affects the patient positively? (IG; AI): Not at all (1)–Very much (10)
-
17.
How did you provide the SCP to patients? More than one answer possible (IG; AI): Personally, on paper/Sent by mail/As PDF by e-mail/Other, namely…
-
18.
How extensively did you discuss the SCP with patients? (IG; AI): Not at all (1)–Very extensively (10)
-
19.
Do you feel that you use more/less time for your consultation because of the SCP? (IG; AI): No, stayed the same/Yes, approximately … minutes more time/Yes, approximately … minutes less time
-
20.
To what extent did you succeed in providing an SCP to all eligible patients? (IG; AI): Not at all (1)–Very well (10)
-
21.
To what extent did the SCP contribute positively to the communication between yourself and the patient? (IG; AI): Not at all (1)–Very much (10)
-
22.
To what extent did you succeed in providing an SCP to all involved Primary Care Physicians? (IG; AI): Not at all (1)–Very well (10)
-
23.
To what extent did the SCP contribute positively to the communication between yourself and the involved Primary Care Physicians? (IG; AI): Not at all (1)–Very much (10)
-
24.
How satisfied are you in general with the use of the SCP? (IG; AI): Not at all (1)–Very much (10)
-
25.
Did you encounter practical problems in the use of the SCP? (IG; AI): No (continue with question 27)/Yes (continue with question 26)
-
26.
Which practical problems did you encounter in the use of the SCP? More than one answer possible (IG; AI): ROGY was not always completed in time/The “SCP button” in ROGY did not always work/There was not always an appropriate moment to discuss the SCP with the patient/Other, namely…
-
27.
Do you have any suggestions for improvements of the SCP? (IG; AI): open-ended
-
28.
How motivated are you to use/keep using the SCP in the future? (IG; AI): Not at all (1)–Very much (10)
-
29.
Who do you think should provide the SCP to the patient? (IG; AI): Gynecologist–GO/(Oncology) nurse–nurse practitioner/Primary Care Physician/Other, namely…
-
30.
Do you have any comments? (CG + IG; BI + AI): OPEN ENDED
Note: CG Control Group; IG Intervention Group; BI Before Inclusion; AI After Inclusion. 1Only for the intervention group after inclusion
Rights and permissions
About this article
Cite this article
Nicolaije, K.A.H., Ezendam, N.P.M., Vos, M.C. et al. Oncology providers’ evaluation of the use of an automatically generated cancer survivorship care plan: longitudinal results from the ROGY Care trial. J Cancer Surviv 8, 248–259 (2014). https://doi.org/10.1007/s11764-013-0327-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-013-0327-1