Abstract
Objective
Determining whether to pursue or terminate resuscitation efforts remains one of the biggest challenges of cardiopulmonary resuscitation (CPR). No ideal cut-off duration has been recommended and the association between CPR duration and survival is still unclear for out-of-hospital cardiac arrest (OHCA). The aim of this study was to assess the association between CPR duration and 30-day survival after OHCA with favorable neurological outcomes according to initial rhythm.
Methods
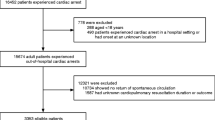
This was an observational, retrospective analysis of the French national multicentric registry on cardiac arrest, RéAC. The primary endpoint was neurologically intact 30-day survival according to initial rhythm.
Results
20,628 patients were included. For non-shockable rhythms, the dynamic probability of 30-day survival with a Cerebral Performance Category (CPC) of 1 or 2 was less than 1% after 25 min of CPR. CPR duration over 10 min was not associated with 30-day survival with CPC of 1 or 2 (adjusted OR: 1.67; CI 95% 0.95–2.94). For shockable rhythms, the dynamic probability of 30-day survival with a CPC score of 1 or 2, was less than 1% after 54 min of CPR. CPR duration of 21–25 min was still associated with 30-day survival and 30-day survival with a CPC of 1 or 2 (adjusted OR: 2.77; CI 95% 2.16–3.57 and adjusted OR: 1.82; CI 95% 1.06–3.13, respectively).
Conclusions
Survival decreased rapidly with increasing CPR duration, especially for non-shockable rhythms. Pursuing CPR after 25 min may be futile for patients presenting a non-shockable rhythm. On the other hand, shockable rhythms might benefit from prolonged CPR.


Similar content being viewed by others
Data availability
The datasets analysed during the current study are available from the corresponding author upon reasonable request.
References
Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS et al (2022) Heart disease and stroke statistics—2022 update: a report from the American heart association. Circulation. https://doi.org/10.1161/CIR.0000000000001052
Gräsner J-T, Wnent J, Herlitz J, Perkins GD, Lefering R, Tjelmeland I et al (2020) Survival after out-of-hospital cardiac arrest in Europe—results of the EuReCa two study. Resuscitation 148:218–226. https://doi.org/10.1016/j.resuscitation.2019.12.042
Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG et al (2020) Part 3: adult basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 142(16_suppl_2):S366–S468
Soar J, Böttiger BW, Carli P, Couper K, Deakin CD, Djärv T et al (2021) European resuscitation council guidelines 2021: adult advanced life support. Resuscitation 161:115–151. https://doi.org/10.1016/j.resuscitation.2021.02.010
Wyckoff MH, Singletary EM, Soar J, Olasveengen TM, Greif R, Liley HG et al (2021) International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; neonatal life support; education, implementation, and teams; first aid task forces; and the COVID-19 working group. Circulation. https://doi.org/10.1161/CIR.0000000000001017
Nordberg P, Hollenberg J, Herlitz J, Rosenqvist M, Svensson L (2009) Aspects on the increase in bystander CPR in Sweden and its association with outcome. Resuscitation 80:329–333. https://doi.org/10.1016/j.resuscitation.2008.11.013
Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF et al (2013) Association of National Initiatives to Improve Cardiac Arrest Management With Rates of Bystander Intervention and Patient Survival After Out-of-Hospital Cardiac Arrest. JAMA 310:1377. https://doi.org/10.1001/jama.2013.278483
Hasselqvist-Ax I, Riva G, Herlitz J, Rosenqvist M, Hollenberg J, Nordberg P et al (2015) Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med 372:2307–2315. https://doi.org/10.1056/NEJMoa1405796
Mentzelopoulos SD, Couper K, de Voorde PV, Druwé P, Blom M, Perkins GD et al (2021) European resuscitation council guidelines 2021: ethics of resuscitation and end of life decisions. Resuscitation 161:408–432. https://doi.org/10.1016/j.resuscitation.2021.02.017
Goto Y, Funada A, Goto Y (2016) Relationship between the duration of cardiopulmonary resuscitation and favorable neurological outcomes after out-of-hospital cardiac arrest: a prospective, nationwide, population-based cohort study. J Am Heart Assoc 5:e002819. https://doi.org/10.1161/JAHA.115.002819
Chai J, Fordyce CB, Guan M, Humphries K, Hutton J, Christenson J et al (2022) The association of duration of resuscitation and long-term survival and functional outcomes after out-of-hospital cardiac arrest. Resuscitation. https://doi.org/10.1016/j.resuscitation.2022.11.020
Matsuyama T, Ohta B, Kiyohara K, Kitamura T (2022) Cardiopulmonary resuscitation duration and favorable neurological outcome after out-of-hospital cardiac arrest: a nationwide multicenter observational study in Japan (the JAAM-OHCA registry). Crit Care Lond Engl 26:120. https://doi.org/10.1186/s13054-022-03994-2
Cheskes S, Verbeek PR, Drennan IR, McLeod SL, Turner L, Pinto R et al (2022) Defibrillation strategies for refractory ventricular fibrillation. N Engl J Med 387:1947–1956. https://doi.org/10.1056/NEJMoa2207304
Adnet F, Triba MN, Borron SW, Lapostolle F, Hubert H, Gueugniaud P-Y et al (2017) Cardiopulmonary resuscitation duration and survival in out-of-hospital cardiac arrest patients. Resuscitation 111:74–81. https://doi.org/10.1016/j.resuscitation.2016.11.024
Reynolds JC, Grunau BE, Rittenberger JC, Sawyer KN, Kurz MC, Callaway CW (2016) Association between duration of resuscitation and favorable outcome after out-of-hospital cardiac arrest: implications for prolonging or terminating resuscitation. Circulation 134:2084–2094. https://doi.org/10.1161/CIRCULATIONAHA.116.023309
Park S, Lee SW, Han KS, Lee EJ, Jang D-H, Lee SJ et al (2022) Optimal cardiopulmonary resuscitation duration for favorable neurological outcomes after out-of-hospital cardiac arrest. Scand J Trauma Resusc Emerg Med 30:5. https://doi.org/10.1186/s13049-022-00993-8
Hubert H, Tazarourte K, Wiel E, Zitouni D, Vilhelm C, Escutnaire J et al (2014) Rationale, methodology, implementation, and first results of the french out-of-hospital cardiac arrest registry. Prehosp Emerg Care 18:511–519. https://doi.org/10.3109/10903127.2014.916024
Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D et al (2015) cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American heart association, European resuscitation council, Australian and New Zealand Council on resuscitation, heart and stroke foundation of Canada, InterAmerican heart foundation, resuscitation council of Southern Africa, Resuscitation Council of Asia); and the American Heart association emergency cardiovascular care committee and the council on cardiopulmonary, critical care perioperative and resuscitation. Circulation 132:1286–1300. https://doi.org/10.1161/CIR.0000000000000144
Adnet F, Lapostolle F (2004) International EMS systems: France. Resuscitation 63:7–9. https://doi.org/10.1016/j.resuscitation.2004.04.001
Kashiura M, Hamabe Y, Akashi A, Sakurai A, Tahara Y, Yonemoto N et al (2017) Association between cardiopulmonary resuscitation duration and one-month neurological outcomes for out-of-hospital cardiac arrest: a prospective cohort study. BMC Anesthesiol 17:59. https://doi.org/10.1186/s12871-017-0351-1
Matsuyama T, Irisawa T, Yamada T, Hayakawa K, Yoshiya K, Noguchi K et al (2020) Impact of low-flow duration on favorable neurological outcomes of extracorporeal cardiopulmonary resuscitation after out-of-hospital cardiac arrest: a multicenter prospective study. Circulation 141:1031–1033. https://doi.org/10.1161/CIRCULATIONAHA.119.044285
Berdowski J, Berg RA, Tijssen JGP, Koster RW (2010) Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation 81:1479–1487. https://doi.org/10.1016/j.resuscitation.2010.08.006
Holmén J, Hollenberg J, Claesson A, Herrera MJ, Azeli Y, Herlitz J et al (2017) Survival in ventricular fibrillation with emphasis on the number of defibrillations in relation to other factors at resuscitation. Resuscitation 113:33–38. https://doi.org/10.1016/j.resuscitation.2017.01.006
Yannopoulos D, Bartos J, Raveendran G, Walser E, Connett J, Murray TA et al (2020) Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. The Lancet 396:1807–1816. https://doi.org/10.1016/S0140-6736(20)32338-2
Chouihed T, Kimmoun A, Lauvray A, Laithier F-X, Jaeger D, Lemoine S et al (2018) Improving patient selection for refractory out of hospital cardiac arrest treated with extracorporeal life support. Shock 49:24–28. https://doi.org/10.1097/SHK.0000000000000941
Abrams D, MacLaren G, Lorusso R, Price S, Yannopoulos D, Vercaemst L et al (2021) Extracorporeal cardiopulmonary resuscitation in adults: evidence and implications. Intensive Care Med. https://doi.org/10.1007/s00134-021-06514-y
Wengenmayer T, Rombach S, Ramshorn F, Biever P, Bode C, Duerschmied D et al (2017) Influence of low-flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR). Crit Care Lond Engl 21:157. https://doi.org/10.1186/s13054-017-1744-8
Bartos JA, Grunau B, Carlson C, Duval S, Ripeckyj A, Kalra R et al (2020) Improved survival with extracorporeal cardiopulmonary resuscitation despite progressive metabolic derangement associated with prolonged resuscitation. Circulation 141:877–886. https://doi.org/10.1161/CIRCULATIONAHA.119.042173
Schneiderman LJ (2011) Defining medical futility and improving medical care. J Bioethical Inq 8:123–131. https://doi.org/10.1007/s11673-011-9293-3
Kuschner CE, Becker LB (2019) Recent advances in personalizing cardiac arrest resuscitation. F1000 Res 8:915. https://doi.org/10.12688/f1000research.17554.1
Ebell MH, Vellinga A, Masterson S, Yun P (2019) Meta-analysis of the accuracy of termination of resuscitation rules for out-of-hospital cardiac arrest. Emerg Med J EMJ 36:479–484. https://doi.org/10.1136/emermed-2018-207833
Conseil français de réanimation cardiopulmonaire (2009) Guidelines for indications for the use of extracorporeal life support in refractory cardiac arrest. Ann Fr Anesth Réanimation 28:187–190. https://doi.org/10.1016/j.annfar.2008.12.026
Abrahamowicz AA, Counts CR, Danielson KR, Bulger NE, Maynard C, Carlbom DJ et al (2022) The association between arterial-end-tidal carbon dioxide difference and outcomes after out-of-hospital cardiac arrest. Resuscitation 181:3–9. https://doi.org/10.1016/j.resuscitation.2022.09.019
Behrends M, Niemann CU, Larson MD (2012) Infrared pupillometry to detect the light reflex during cardiopulmonary resuscitation: a case series. Resuscitation 83:1223–1228. https://doi.org/10.1016/j.resuscitation.2012.05.013
Parnia S, Yang J, Nguyen R, Ahn A, Zhu J, Inigo-Santiago L et al (2016) Cerebral oximetry during cardiac arrest: a multicenter study of neurologic outcomes and survival. Crit Care Med 44:1663–1674. https://doi.org/10.1097/CCM.0000000000001723
Acknowledgements
The French National Cardiac Arrest Registry (RéAC) was supported by the French Society of Emergency Medicine (SFMU), the Fédération Française de Cardiologie, the University of Lille and the Institute of Health Engineering of Lille. We thank all of the prehospital emergency medical service units involved in the French National Out-of-Hospital Cardiac Arrest Registry (RéAC).
Funding
This study received no specific funding.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study’s conception and design. Methodology: DJ, ML, VC, GD, HH, TC. Formal analysis and investigation: ML, VC, HH. Writing—original draft preparation: DJ, ML. Writing—review and editing: All authors. Supervision: GD, DY, HH, TC.
Corresponding author
Ethics declarations
Conflict of interest
Demetri Yannopoulos received grants from the Leona M and Harry B Helmsley Charitable Trust.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jaeger, D., Lafrance, M., Canon, V. et al. Association between cardiopulmonary resuscitation duration and survival after out-of-hospital cardiac arrest according: a first nationwide study in France. Intern Emerg Med 19, 547–556 (2024). https://doi.org/10.1007/s11739-023-03449-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-023-03449-8