Abstract
Cardiac amyloidosis (CA) is due to extracellular myocardial deposition of misfolded proteins resulting in severe cardiac dysfunction and death. The precursors of amyloid fibrils, able of determining a relevant cardiac infiltration, are immunoglobulin-free light chains (AL amyloidosis) and transthyretin (TTR) (both wild and mutated types). The diagnosis of amyloidosis represents a challenge for the clinician given its rarity and its protean clinical presentation, thus an early diagnosis remains a cornerstone for the prognosis of these patients, also in light of the growing available treatments. There is great interest in identifying and applying biomarkers to help diagnose, inform prognosis, guide therapy, and serve as surrogate endpoints in these patients. In AL amyloidosis, biomarkers such as free light chains, natriuretic peptides and troponins are the most extensively studied and validated; they have proved useful in risk stratification, guiding treatment choice and monitoring hematological and organ response. A similar biomarker-based prognostic score is also proposed for ATTR amyloidosis, although studies are small and need to be validated for wild-type and mutant forms.
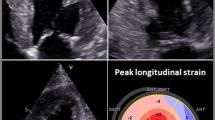
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyloidosis is a disease due to the extracellular deposition of misfolded proteins in various tissues and organs, including the heart [1]. The two main types of amyloidosis capable of inducing clinically relevant cardiac involvement are light chain (AL) amyloidosis, in which amyloid fibrils originate from light chains (LC) of circulating monoclonal immunoglobulins, and transthyretin amyloidosis (ATTR). Destabilization of the tetrameric circulating TTR may either be due to age-related changes in wild-type disease (ATTRwt) or inherited mutations in the transthyretin gene (ATTRv) transmitted through an autosomal-dominant manner. In AL amyloidosis, a small and indolent B cell clone produces a light chain (λ chain in the majority of patients) with mutations in the variable region, inducing misfolded protein with high thermodynamic instability, generating soluble amyloid oligomers and causing inappropriate aggregation [2]. The amyloid deposits, through a mass effect, induce a widespread disruption of tissue architecture and the oligomers, through their toxic effects, compromise cellular function and induce organ dysfunction (Fig. 1A). Heart, kidney, peripheral nerves, liver and soft tissues are the main target organs of AL amyloid but rare and unusual localizations in many other tissues are equally possible [3]. In ATTR, circulating TTR, during the aging process, or in the context of a mutation, loses its quaternary structure altering its native form and favoring dissociation into oligomers and monomers which then precipitate in the tissues inducing organ damage (Fig. 1B). Several reports [4, 5] described an incidence of AL amyloidosis of about 1.2 (0.8–1.6) per 100,000 person-years with a trend that remains stable across the last decades. No data are available on incidence and prevalence of ATTR amyloidosis. It is believed that the prevalence of ATTRv is approximately 50,000 patients worldwide and that cardiac involvement is present in about 80% of cases, but these data may be underestimated [6]. The most common variant worldwide of TTRv with cardiac phenotype is the Val122Ile, which occurs in 3–4% of blacks American, with unknown phenotypic penetrance [7, 8]. The Italian Registry for ATTRv estimated a prevalence of 4.3/million, with regional differences [9]. ATTRwt is typically diagnosed at 70–75 years of age, with a striking male predominance [10, 11], and a prominent cardiac clinical phenotype. The last decade has been particularly relevant for TTR-CA thanks to the introduction in the diagnostic process of the scintigraphy with bone tracer and to its validation as a non-biopsy diagnostic tool by Gilmore et al. [12]. The easy and widespread access to bone scintigraphy together with a greater awareness of the disease and the imminent availability of disease modify treatments has led to a significant increase in the diagnoses of this type of amyloidosis suggesting that the real prevalence of ATTR is likely to be higher than what has been described so far [13, 14]. The diagnostic workup of CA includes the use of non-invasive cardiac imaging methods such as echocardiography, nuclear medicine, cardiac magnetic resonance as well as the use of specific genetic tests, frequently associated with histological demonstration of fibril amyloid deposits [15, 16]. Amyloidosis is a rare, complex and multi-organ disease that requires close interdisciplinary collaboration between various specialists to effectively diagnose, treat and support patients. The internist, together with the cardiologist, is an essential part of the multidisciplinary team that manages these patients throughout their clinical course. In particular internist, to whom patients with multi-organ dysfunction are most often addressed, must be aware of this disease and must be able to recognize it promptly especially in the early clinical manifestations, when organ damage is still amenable to treatment. Early diagnosis of amyloidosis and in particular of cardiac involvement is crucial meanly because overall survival is poor once overt cardiac involvement is present [1, 17,18,19,20]. The aim of treating amyloidosis is the greatest reduction of circulating amyloidogenic precursors and stop amyloid fibrils deposition, to halt or reverse organ damage. The choice of therapy, its duration, the evaluation of its effectiveness, the quantification of organ damage and its evolution during the course of therapy are all key moments for an optimal management of these complex patients. In this setting, the use of circulating biomarkers such as natriuretic peptides and high-sensitivity troponin, together with free light chains for AL amyloidosis, can be very useful in the management of these key steps and are used in clinical trials as indicators of response to treatment and as surrogate clinical endpoints (Central Illustration). Thanks to their multidisciplinary background, internists play a pivotal role in the management of this protean disease and are the only ones able to provide these patients with continuous and attentive support during treatment and follow-up. It is, therefore, imperative that internists have knowledge and awareness of the correct use of these biomarkers and that they are able to translate them into daily clinical practice for the correct classification and management of these complex patients. In this review, we aimed to summarize the current clinical use of circulating biomarkers for the assessment of diagnosis, prognosis, risk assessment and response to therapy in patients with CA and to mention the new areas of ongoing investigation in this field.
Pathophysiology of amyloid disease. A In AL amyloidosis, a small and indolent B cell clone overproduces a monoclonal light chain (λ in the majority of patients) with mutations in the variable region, which misfolds generating soluble amyloid oligomers and causing inappropriate aggregation into amyloid fibrils. The amyloid deposits, through the mass effect, induce a widespread disruption of tissue architecture and the oligomers, through their toxic effects, compromise cellular function and induce dysfunction in target organs. B Transthyretin is a homotetramer that circulates in the blood in equilibrium between the form bound to its ligands and the free form. Under physiological conditions, the TTR tetramer is relatively stable and the misfolding capacity is relatively low. Due to multiple mechanisms, largely unknown, the tetramer tends to separate into monomers that misfolds producing unstable, toxic intermediates, prone to aggregation with amyloid fibrils tissue deposition. During this amyloidogenic process, the native, soluble and stable TTR molecules, or FLC, are transformed into unstable and toxic intermediates and finally into very stable insoluble fibrils that are extremely resistant to degradation by tissue elimination systems. Central illustration: FLC free light chains, AL light chain amyloidosis, ATTR transthyretin amyloidosis, NT-proBNP N-terminal pro-brain natriuretic peptide, BNP brain natriuretic peptide, ST2 soluble suppression of tumorigenicity 2, GDF-15 growth differentiation factor-15, eGFR estimated glomerular filtration rate, TTRc circulating transthyretin, ATTR TTR amyloidosis. Green bars are myocardial amyloid fibrils deposit impairing heart function (Color figure online)
Circulating biomarkers for diagnosis of amyloidosis
AL amyloidosis
Biomarkers for diagnosis of AL amyloidosis
By definition, all patients with AL amyloidosis are characterized by the presence of free LCs (FLC) produced by a small B cell malignant clone, most often from bone marrow plasma cells [2]. In healthy subjects, plasma cells physiologically produce LCs in excess that do not bind to heavy chains to form a complete immunoglobulin (Ig) molecule, so that a small quantities of FLCs are present in the serum of normal subjects. In AL amyloidosis, the malignant B clone produces an excess of either intact Ig or FLCs of a single type (κ or λ) called monoclonal component (MC). In AL amyloidosis, amyloidogenic monoclonal FLCs are both the marker of the underlying clonal disease and the main pathogenic agent of tissue damage. Prior to the introduction of the FLC assay, the quantification of the amyloid protein precursor was inaccurate and derived from the amount of circulating intact serum monoclonal Ig, the amount of light chains in the urine and the number of plasma cells in the bone marrow [21]. Due to the small clone, in amyloidosis, the FLC production may be very small and may not reach concentrations high enough to be detected by serum protein electrophoresis (sPEP) or by serum and urinary immunofixation (sIFE and uIFE) [22]. Furthermore, unlike multiple myeloma, fewer than half of patients with AL have detectable circulating intact monoclonal Ig, and in many others, the concentration of monoclonal Ig is as low as accurate quantification is not possible. Since demonstrating the presence of a circulating MC is a cornerstone of the diagnosis of AL amyloidosis, the inability with these assays to detect a small MC can result in a misdiagnosis. The use of the serum FLC assay, combined with sIFE and uIFE, can detect the underlying monoclonal gammopathy, with a propensity to amyloid, in approximately 96–98% of patients with AL [23, 24]. Omitting any of these tests may result in the inability to diagnose underlying plasma cell dyscrasia and thus delay or miss the diagnosis of AL amyloidosis. If all tests are negative, AL amyloidosis is unlikely and further evaluation is not indicated unless the clinical index of suspicion is very high. The commercially available antibodies, used to measure FLCs, recognize, with high specificity, the LC epitopes that are exposed only when the LC are unbound. The Freelite (The Binding Site Ltd, Birmingham, UK) assay utilizes highly specific polyclonal sheep antibodies, while the N-Latex (Siemens Healthcare Diagnostics, Marburg, Germany) assay is based on monoclonal antibodies. Although the N-Latex and Freelite™ assays present several differences, they have similar diagnostic sensitivity and prognostic performance, but the between-assay agreement is modest [25]. In normal subjects, the kidney is the major site of FLCs’ catabolism with a serum half-life depending on their molecular weight. Monomeric k FLCs are cleared in 2–4 h, while dimeric λ FLCs in 3–6 h. Thus, in a patient with advanced kidney disease, the decline in glomerular filtration rate results in increased serum FLC concentrations. Due to the different kidney catabolism on κ and λ FLCs, the reference range for FLC κ/λ at Freelite assay has proven to be inappropriate to reveal an underlying amyloidogenic FLC, especially in patient with λ clones. A wider reference range, for FLCs κ/λ ratio with Freelite, has been recommended in patients with advanced kidney disease (0.37–3.1 instead of 0.26–1.65) [26].
Biomarkers for assessment of cardiac involvement in AL amyloidosis
Determination of cardiac involvement in systemic AL amyloidosis is of vital importance and is crucial for staging, determining prognosis and tailoring treatment. NT-proBNP is a highly sensitive, although not specific, marker of cardiac involvement in patients with extracardiac biopsy-proven AL amyloidosis. NT-proBNP values below the 97.5 percentile for normal subjects virtually excludes significant AL cardiac involvement and may obviate the use of imaging tests such as echocardiography or MRI in patients with low clinical suspicion of CA [27]. Increased NT-proBNP levels have been observed in AL amyloidosis with preclinical cardiac involvement, even in patients with apparently normal echocardiographic findings [28]. This feature seems related to a direct toxic effect of LCs on myocardial cells, that is independent of infiltrative damage. Amyloidogenic LCs from patients with cardiac AL amyloidosis may induce mitogen-activated protein kinase (MAPK) p38 signaling, which, in addition to mediating cardiomyocyte dysfunction and cell death, can also induce BNP transcription, supporting a possible link between the cardio toxic effects of LCs and increased natriuretic peptides release [29, 30]. Consequently, NT-proBNP could be considered a useful screening tool for detecting an underlying preclinical CA in some at-risk populations such as patients with MGUS and an abnormal FLC ratio [31]. Since most patients with AL amyloidosis at onset show high levels of NT-proBNP and/or albuminuria, evaluation of these two parameters in patients with MGUS and abnormal FLC ratio at each follow-up visit, may lead to a preclinical diagnosis of AL amyloidosis, with significant benefits in terms of treatment efficacy and overall survival [32]. The amyloidosis consensus statement defines cardiac involvement, in the presence of extracardiac biopsy-proven systemic amyloidosis, as the presence of a mean left ventricular (LV) end-diastolic wall thickness ≥ 12 mm on echocardiography in the absence of other possible causes, or an NT-proBNP > 332 pg/mL in the absence of atrial fibrillation or renal failure. In a pivotal study on patients with AL amyloidosis [33], Palladini et al. demonstrated that NT-proBNP retained a good diagnostic accuracy for cardiac involvement even in case of reduced glomerular filtration rate (GFR), using a higher NT-proBNP cutoffs (332 pg/mL, 543 pg/mL and 2642 pg/mL for patients with GFR ≥ 60, 60–15 and < 15 mL/min/1.73 m2, respectively) [34]. As BNP is less cleared by kidney, higher diagnostic cutoffs have been suggested only for patients with GFR < 15 mL/min/1.73 m2 (221 pg/mL instead of 73–78 pg/mL) [34].
ATTR amyloidosis
Biomarkers for assessment of cardiac involvement in ATTR amyloidosis
The diagnostic role of circulating biomarkers and, in particular, of natriuretic peptides and troponins in diagnosis of ATTR CA has not been evaluated so far. In general, NT-proBNP levels are significantly lower in ATTR-CA than in AL-CA amyloidosis and in ATTRv-CA than in ATTRwt, despite similar LV mass and renal function [35]. This discrepancy could be due to a lower cytotoxicity of TTR amyloid fibrils and a slower amyloid deposition process in ATTR [35]. Cardiac biomarkers evaluation is also recommended in pre-symptomatic TTRv carriers with predominant cardiac phenotype mutation, starting 10 years before the predicted age of onset of symptomatic disease. In case of abnormal values, even in the absence of symptoms suggestive of cardiac involvement, it is recommended to carry out a series of diagnostic investigations, first, a bone tracer scintigraphy to reach a definitive and early diagnosis [36].
Biomarkers for staging and prognosis
AL amyloidosis
The prognosis of patients with AL amyloidosis is largely based on the presence and extent of cardiac dysfunction. Several studies have revealed that both NT-proBNP and troponins have prognostic predicting value in AL patients. In 2004, Dispenzieri et al. [37] proposed and validated a prognostic risk staging based on NT-proBNP and cardiac troponin. They identified, in newly diagnosed AL patients, three stages associated to different incremental mortality risks. For this staging system, the threshold values for the NT-proBNP were 332 pg/mL, and 0.035 mg/L for cTnT (or 0.1 mg/L for cTn I) with stage I characterized by both biomarkers below the threshold, stage II with one biomarker above the threshold and stage III with both the biomarkers above the thresholds. Stage I, II and III were associated with significantly reduced median survivals of 102, 23 and 9 months, respectively. Wechalekar et al. [38], analyzing the outcomes response to chemotherapy in a large cohort of patients classified as stage III, identified an additionally ultra-high risk population characterized by NT-proBNP concentrations > 8500 pg/mL and troponin T > 0.035 mg/L (Table 2) associated with a systolic blood pressure lower than 100 mmHg. In this group of patients, indicated as stage IIIB, the median of OS (Overall Survival) was only 3 months. Indeed, Mayo stage IIIB patients have a very dismal outcome characterized by early deaths, due to severe and irreversible cardiac dysfunction. This staging system has been accepted for prognosis in clinical practice and indicated as Mayo2004/European. Accurate identification of such patients is important because treatment in this group is particularly challenging. Based on the demonstration that difference > 180 mg/L between involved and uninvolved FLCs, (dFLC) is an independent prognostic factor in AL amyloidosis, in 2012, the Mayo2004 staging system was revised and expanded including the clonal dFLCs [39]. This new Mayo2012 staging system sets different cutoff thresholds values for NT-proBNP > 1,800 pg/mL and for cTnT > 0.025 ng/mL (Table 2). This brought stages from I to IV with a median overall survival of 94.1, 40.3, 14, and 5.8 months, respectively (p < 0.001). The Mayo2012 system has been also validated using high-sensitivity cTnT (Roche Diagnostics by ELECSYS 2010 automated analyzer) with a cutoff > mg/L. The 99th percentile upper reference limit of this assay was greater than 14 ng/L for hs-cTnT with a limit of detection of 5 ng/L and a 10% coefficient of variation value of 13 ng/L [40]. The predicting value of all these three staging systems was confirmed by Dittirch et al. [41] even in patients with renal failure (50 mL/min/1.73 m2) and atrial fibrillation, two conditions commonly affecting cardiac biomarkers serum levels. A prognostic staging system was also determined using BNP (instead NT-proBNP) threshold values of 81 pg/mL and maintaining the same cutoff for TnI (< 0.1 mg/L) as in Mayo 2004 [42] (Table 1). Furthermore, Abdallah et al. [43] have recently demonstrated in more than 1,000 patients with AL amyloidosis that all the current staging systems retain prognostic value when used for re-stratify prognosis at 3 and 6 months from first-line treatment initiation. They have also showed that migration to a worse disease stage predicts decreased survival, whereas improvement in disease stage predicts longer survival in the subset of patients with advanced-stage at diagnosis Autologous stem cell transplantation (ASCT) is a well-recognized treatment with excellent outcomes in selected patients with AL amyloidosis. Although the eligibility criteria for ASCT varied across centers, there is a consensus to exclude patients aged > 70 years, significant involvement of more than two organs, including heart, significantly decreased renal function and low systolic blood pressure [44,45,46]. Concerning cardiac biomarkers, several studies [45, 46] suggest that patients with serum troponin T level above 0.06 ng/mL and/or NT-proBNP levels above 5000 pg/mL should be excluded from ASCT, due to higher transplant-related mortality rates.
ATTR amyloidosis
Biomarkers and risk stratification of ATTR CA
Prognostic stratification in ATTR amyloidosis remains challenging, due to the frequently delayed diagnosis, different progression in cardiac infiltration due to the specific amyloid precursor (wild-type or mutated TTR), to the intrinsic mutation phenotype, whit its geographical distribution, to the endemic/non-endemic aggregation, gender and parental heritability [47,48,49]. However, the presence and the extent of cardiac involvement are by far the main prognostic factors, regardless of the specific amyloid precursor. The recent availability of effective therapeutic approaches for ATTR generated the need for effective tools to assess patient prognosis, helping clinicians in daily practice and researchers in further studies developing. Biomarker-based prognostic staging systems have been developed for ATTR-CA, following the model adopted for AL amyloidosis. Two different staging systems have been proposed: in 2016, Grogan et al. [50] demonstrated that in a cohort of wtATTR-CA patients, NT-proBNP (cutoff 3000 pg/mL) and hsTnT (cutoff 0.05 ng/mL) plasma values were able to stratify the risk for death similarly as previously observed in AL patients. Gillmore et al. in 2017 demonstrated the prognostic performance of combining NT-proBNP (cutoff 3000 pg/mL) and estimated glomerular filtration rate (eGFR cutoff 45 mL/min/1.73 m2) in both wt- and hATTR-CA patients [51] (Table 2). The comparison of the two staging systems in a population of 172 ATTR CA patients (133 with ATTRwt and 42 with ATTRv-CA), showed that only 70% of patients were classified by the two different staging systems in the same stage with a kappa value of 0.541 [52]. Most of the discordances were observed for stages 2 and 3. The Gillmore staging allows for better stratification of patients in three subgroups with significantly different survival and risk for all-cause mortality. The same holds true for the Hazard Ratio analysis, while no statistically significant difference was detected between stages 1 and 2 in the overall population, according to the modified Grogan staging system. The combination of NT-proBNP and eGFR seems to lead to a better discrimination of patient prognosis than the combination of NT-proBNP and troponin, possibly as an expression of a type 2 cardiorenal syndrome, frequently observed in ATTR CA patients; therefore, it could be the chosen staging system in clinical practice. This stage has been indicated as National Amyloidosis Centre (NAC) transthyretin amyloidosis stage. Recently, Cheng et al. [53] reported that diuretic dose and NYHA functional class are independent predictors of mortality in ATTR-CA in addition to Grogan and Gilmore risk scores. Testing these risk scores in 309 patients with ATTR-CA (66.0% with ATTRwt and 34.0% with ATTRv), they showed that adding diuretic dose as categories (0 mg/kg; > 0 to 0.5 mg/kg; > 0.5 to 1 mg/kg; and > 1 to 2 mg/kg) improves the area under the curve of the Grogan risk score from 0.693 to 0.767 and the Gillmore risk score from 0.711 to 0.787, preserving calibration in both cases. Adding NYHA functional class, the area under the curve further improved to 0.798 and 0.816, respectively. Given that diuretic dose and NYHA functional class are easily obtainable information, they suggested that these variables should be considered in the clinical setting to better stratify the patients risk.
Circulating biomarkers for assessment of response to therapy
AL amyloidosis
Assessment of hematological response to therapy
Unlike multiple myeloma, organ failure and mortality in AL are directly due to the harmful effects of misfolded monoclonal LCs rather than the proliferation of monoclonal bone marrow plasma cells. Therefore, the immediate goal of AL amyloidosis treatment is to significantly and rapidly reduce the production of amyloidogenic FLCs to reduce organ damage. The greater (and faster) reduction in the FLC, the greater the possibility of improving the function of the affected organs and consequently survival. The possibility of quantifying FLCs represented a cornerstone in the management of this disease and allowed to evaluate and monitor the therapeutic response after chemotherapy. In 2012, in a large population of patients with AL amyloidosis, Palladini et al., using the Freelite assay, [54] identified the prognostic relevance of different criteria for predicting the hematologic response to treatment. They defined four levels of hematologic response categories: complete response (CR; negative serum and urine IFX and normal FLC ratio), very good partial response (VGPR; difference between involved and uninvolved FLCs [dFLC] < 40 mg/L), partial response (PR; dFLC decrease > 50%), and no response (NR). Changes in FLCs strongly predicted survival as early after few course of treatment (Table 3A). In AL amyloidosis, the quickly and profound reductions of the amyloid LCs burden (such as in VGPR or CR) are closely correlated with survival and are associated with the greatest chance of functional improvement of infiltrated organ. Thus, a VGPR should be the minimal goal of therapy in these patients. However, a high percentage of patients with AL are still diagnosed with too advanced cardiac dysfunction, which may not be improved even with an effective chemotherapy. Due to assay inaccuracy, patients with a dFLC less than the threshold of 50 mg/L are not evaluable for hematological response and are excluded from clinical trials. However, these patients with low FLC levels at baseline are not uncommon in AL amyloidosis, ranging from 13 to 19% of all patients [55, 56]. This population shows a high rate of renal involvement, but low rate of liver and cardiac involvement, which translate in a better clinical outcome [57]. In these patients, normalization of iFLC levels or decrease in dFLC < 10 mg/L (baseline at least 20 mg/L) were predictive of better overall survival and may be used for detecting hematological response [57]. Recently, the 2012 response criteria were updated by International Society of Amyloidosis (ISA) that propose that the previous response criteria be expanded to define complete hematological response as the absence of amyloidogenic light chains (either free or part of a complete immunoglobulin) described as negative serum and urine immunofixation and either a FLC ratio within the reference range or an abnormal FLC ratio as long as the uninvolved-FLC concentration is greater than involved-FLC concentration [58]. The meaning of this clarification is that an abnormal FLC ratio does not preclude the achievement of CR when the concentration of uninvolved, non-amyloidogenic, FLC is greater than that of the involved, amyloidogenic, FLC. This is particularly relevant today when highly effective anti-plasma cell therapies are available that can cause profound reductions in both-involved-FLC and uninvolved-FLC, possibly resulting in an inverted FLC ratio favoring non-amyloidogenic FLC. It is important to remind that current response criteria are validated using the Freelite assay and cannot be automatically applied to the N latex FLC method. In patients who achieved a VGPR or better response, a stringent clinical and biochemical surveillance should be started including a bimonthly assessment of serum FLC levels. In most patients, organ damage progression is frequently preceded by FLC increases, which can be subtle and should not be underestimated. However, there is no consensus on when and at which dFLC threshold, suggestive of relapse, the treatment should be started.
Assessment of organ damage response to therapy
In 2012, ISA validated the cardiac, renal and liver criteria for organ response as reported in Table 3B. Criteria for cardiac response is based exclusively on circulating NT-proBNP: a ≥ 30% and ≥ 300 pg/mL reduction in NT-proBNP starting from a baseline NT-proBNP ≥ 650 pg/mL has been defined as appropriate cardiac response, while a ≥ 300 pg/mL and ≥ 30% increase in NT-proBNP identified cardiac progression [54]. Cardiac response criteria to treatment and related survival rate were also validated using the BNP [59]. Since then, several studies have demonstrated that such biomarker-based cardiac response predicts survival regardless of the treatment regimen [60,61,62,63,64]. The NT-proBNP and BNP variation at 6 months from treatment (both ASCT or chemotherapy) predicts disease progression and are associated with better survival expectations [54, 59]. Data on troponin and its usefulness to monitor cardiac response to chemotherapy in AL are less well established. Palladini et al. in 2010 [65] demonstrated that > 75% increase in hs-cTnT from baseline values after chemotherapy, is an independent negative prognostic factor in AL amyloidosis. In AL amyloidosis, markers of hematological and other organs response should be monitored in parallel and frequently during chemotherapy, knowing that hematological response rarely goes hand to hand to organ response that usually may delay by several months [66]. Particular attention must be paid to the interpretation of the cardiac response in patients treated with immunomodulatory drugs (Thalidomide, Lenalidomide and Pomalidomide) due to their direct cardio toxic effect or fluid retention which directly increase NT-proBNP levels [67]. After ASCT, the clinical and biomarkers response should be frequently assessed, at least every 3 months and every 1 to 2 months after non-transplantation therapies, to allow a rapid switch to rescue therapy in patients who do not achieve an appropriate response. Recently, Sidana and Milani [68], respectively, validated, in two large independent cohorts of patients with AL amyloidosis, a model for early assessment of treatment benefit at 6 months, integrating both hematologic (HR) and organ response (OR) assessment (Table 3C). In this multi-marker strategy (CHOR model), they assigned four different scores to HR: 0 = complete response (CR), 1 = very good partial response (VGPR), 2 = partial response (PR), 3 = no response (NR) or progression; while OR was classified as follow: 0 = all organ (heart, kidney, liver) response (AOR), 1 = mixed organ response (MOR), described as response in at least one organ and 2 = no organ response (NOR). A composite HR/OR (CHOR) model was developed using incremental scoring from 0 to 5 based on hazard ratio, starting from score 0 (complete OR and HR) to score 5 (OR = 2 and HR = 3). Patients were then divided into two groups: CHOR group 1 (scores 0–3) and CHOR group 2 (scores 4–5). In both the two large independent cohorts, patients CHOR group 1 showed significant better OS (p 0.001) than patients CHOR group 2, median OS in group 1 and group 2 were, respectively, not reached vs 34 months, p < 0.001 in the Mayo cohort and 87 vs 23 months, p < 0.001 in the Pavia cohort. With this model, overall survival in both cohorts showed greater predictive power than hematological response or organ response assessed separately.
ATTR amyloidosis
In the last years, the treatment of ATTR-CA is shifting from standard heart failure therapies and organ transplant to disease-modifying treatments [69]. Currently, there are two key approaches to disease-modifying therapy in ATTR: stabilizing the TTR tetramer thus reducing its amyloidogenicity and/or suppression of TTR production with gene silencing therapies. RNA silencing therapies include Patisiran, a ribonucleic acid interference agent, and Inotersen, an antisense oligonucleotide inhibitor [70]. Although many of these treatments are currently reserved for ATTRv patients with neurological phenotype, there is a need to evaluate the potential role of biomarkers in the assessment of cardiac response to therapy and as prognostic markers even in ATTR patients with cardiac involvement. However, the criteria defined to assess cardiac response to therapy in ATTR have not been validated so far [70]. Serum TTR is secreted by the liver and it functions as secondary carrier of thyroxine and binding partner retinol-binding protein-4 (RBP4). In ATTR, the misfolding of TTR initially involves a dissociation of the tetramer into a monomer and the formation of partially misfolded monomeric intermediates which are amyloidogenic and which subsequently self-assemble into amyloid fibrils via soluble aggregation. Mutations in the TTR gene capable of reducing tetramer stability are associated with decreased circulating levels likely due to increased tissue deposition of TTR derived fibrils [71, 72], while in subjects with Thr119Met, a TTR super-stabilizing and protective mutations, the levels are increased [73]. Notably, the treatment with AG-10, a selective TTR stabilizer which acts by mimicking the stabilizing effects of the Thr119Met variant, increases the TTR serum levels both in ATTRv and ATTR wt suggesting that an increase of TTR plasma level could be considered as a surrogate end point of effective stabilization [74]. On the other hand, gene silencers have the opposite effect on circulating TTR levels, with the rationale of a TTR amyloid substrate reduction. In the Apollo study, patients receiving Patisiran had a persistent 81% reduction of TTR circulating levels with clinical improvement of neuropathy and quality of life [75], indicative that, in this case, the rate of TTR reduction may be used as a useful biomarker candidate for clinical response to Patisiran. Similar results, in term of reduction of TTR levels, were reported in patients receiving Inotersen in the NEURO TTR study [76]. Recently, Law et al. [77] reported that change in NT-proBNP concentration, during the first year of follow-up, is a powerful independent predictor of mortality in a large cohort of patients with untreated wtATTR-CM. The authors emphasize that the prognostic relevance of the NT-proBNP changing was independent of NAC ATTR stage, troponin T, age, NYHA class, 6MWT distance, presence of atrial fibrillation and interventricular septal thickness at echocardiography.
Novel biomarkers for CA
Preliminary studies suggest that growth differentiation factor-15 (GDF-15) [78], soluble suppression of tumorigenicity 2 (ST2) [79], hepatocyte growth factor [80], mid-regional pro-adrenomedullin [81], and von Willebrand factor [82] may be useful to improve risk stratification in patients with AL amyloidosis, both in conjunction or substitution to the existing Mayo staging systems but, apart GDF-15 and ST2, they remain in early stages of clinical investigation and merit further clinical evaluation. Among the “omics” science, the transcriptomics explore the complete set of RNA transcripts from DNA in a cell or tissue. The transcriptome includes ribosomal, messenger, transfer RNA, other non-coding RNA and micro RNA (miRNA). Analysis of circulating miRNAs in amyloidosis is in their beginning but appears to show promising results. Weng et al. reported that several miRNAs are dysregulated and expressed at increased levels in bone marrow plasma cell from AL patients and that miRNA-16 is reduced in patients responsive to anti-plasma cell chemotherapy, but not in patients who had persistent disease [83]. Fishov et al. found that ten distinct miRNAs were significantly differently expressed in bone marrow samples from newly diagnosed AL amyloidosis patients compared to MM patients, and that many other miRNAs differed significantly among AL, MM patients and healthy controls, suggesting that these different patterns of miRNAs expression among the three groups, could be used to better understand the pathogenesis of the disease and predict the risk of progression to AL amyloidosis among patients with known plasma cell dyscrasia [84]. Circulating miRNAs have been also explored in patients with ATTRv and ATTRwt cardiomyopathy. Derda et al. in an array profiling experiments found 10 candidates being deregulated in TTR amyloidosis. Among them, the miR-339-3p was found up-regulated only in ATTRwt, but not in patients with heart failure of other origin or with ATTRv, supporting miR-339-3p as a potential candidate biomarker for ATTRwt [85]. Vita et al., exploring the miRNAs expression profile in a group of patients with ATTRv and neurological phenotype compared to those of patients whit Charcot Marie Toot disease and healthy controls, found a profound dysregulation in the expression of several miRNAs with some up-regulated and other down-regulated as a function of different stages of amyloid polyneuropathy. In particular, the serum level of miR-150-5p has been shown to discriminate well the symptomatic stage 1–2 compared to the asymptomatic stage 0 [86]. Although the study of miRNAs in amyloidosis is promising, it should nevertheless be emphasized that a strong evidence on their role as a specific biomarkers for diagnosis, risk stratification and treatment guidance currently has yet to be validated.
Conclusion
In AL amyloidosis, biomarkers such as FLCs, natriuretic peptides and troponins are the most extensively studied and validated; they have proved useful to risk stratification, to guide treatment choice and to monitor hematological and organ response. Unlike AL, the role of circulating biomarkers (natriuretic peptides, TTR, RPB4) in the diagnosis and management of TTR-CA is much less defined and validated. The availability of disease-modifying agents highlights the need for new markers capable of addressing correct clinical management and more accurate prognostic stratification. In particular, markers are welcome to define the minimum disease threshold to justify the starting new treatments and to exclude patients with degrees of infiltration so advanced that they do not come any benefit from therapy or to identify “responders” and “non-responders” to a specific disease-modifying agent. Currently, no single or groups of biomarkers appear to possess these properties. A multiple biomarkers’ approach probably could offer better possibilities in the management of these patients, above all in the management of response to therapy.
References
Perfetto F, Cappelli F, Bergesio F, Ciuti G, Porciani MC et al (2013) Cardiac amyloidosis: the heart of the matter. Intern Emerg Med 8:191–203
Merlini G, Stone MJ (2006) Dangerous small B-cell clones. Blood 108(8):2520–2530
Perfetto F, Casagrande S, Barilaro A, Di Gioia M, Santi R, Allinovi M, Romoli S, Boschi A, Desideri I, Taborchi G, Ungar A, Cappelli F (2021) Progressive and atypical neurological symptoms in refractory systemic AL amyloidosis. Intern Emerg Med 16(7):1927–1933. https://doi.org/10.1007/s11739-020-02489-8 (Epub 2020 Sep 14)
Kyle RA, Larson DR, Kurtin PJ, Kumar S, Cerhan JR, Therneau TM, Rajkumar SV, Vachon CM, Dispenzieri A (2019) Incidence of AL amyloidosis in Olmsted County, Minnesota, 1990 through 2015. Mayo Clin Proc 94(3):465–471. https://doi.org/10.1016/j.mayocp.2018.08.041 (Epub 2019 Jan 31)
Zampieri M, Cappelli F, Allinovi M, Olivotto I, Antonioli E, Tassetti L, Zocchi C, Andrei V, Di Mario C, Nozzoli C, Curciarello G, Ciciani AM, Bergesio F, Vannucchi AM, Perfetto F (2021) Incidence of light chain amyloidosis in Florence metropolitan area, Italy: a population-based study. Amyloid 10:1–2. https://doi.org/10.1080/13506129.2021.1898365
Hawkins PN, Ando Y, Dispenzeri A, Gonzalez-Duarte A, Adams D, Suhr OB (2015) Evolving landscape in the management of transthyretin amyloidosis. Ann Med 47:625–638. https://doi.org/10.3109/07853890.2015.1068949
Jacobson DR, Pastore R, Pool S, Malendowicz S, Kane I, Shivji A, Embury SH, Ballas SK, Buxbaum JN (1996) Revised transthyretin Ile 122 allele frequency in African-Americans. Hum Genet 98:236–238. https://doi.org/10.1007/s004390050199
Quarta CC, Buxbaum JN, Shah AM, Falk RH, Claggett B, Kitzman DW, Mosley TH, Butler KR, Boerwinkle E, Solomon SD (2015) The amyloidogenic V122I transthyretin variant in elderly black Americans. N Engl J Med 372:21–29. https://doi.org/10.1056/NEJMoa1404852
Russo M, Obici L, Bartolomei I, Cappelli F, Luigetti M, Fenu S, Cavallaro T, Chiappini MG, Gemelli C, Pradotto LG, Manganelli F, Leonardi L, My F, Sampaolo S, Briani C, Gentile L, Stancanelli C, Di Buduo E, Pacciolla P, Salvi F, Casagrande S, Bisogni G, Calabrese D, Vanoli F, Di Iorio G, Antonini G, Santoro L, Mauro A, Grandis M, Di Girolamo M, Fabrizi GM, Pareyson D, Sabatelli M, Perfetto F, Rapezzi C, Merlini G, Mazzeo A, Vita G (2020) ATTRv amyloidosis Italian Registry: clinical and epidemiological data. Amyloid 27(4):259–265. https://doi.org/10.1080/13506129.2020.1794807 (Epub 2020 Jul 22)
Gagliardi C, Perfetto F, Lorenzini M et al (2018) Phenotypic profile of Ile68Leu transthyretin amyloidosis: an underdiagnosed cause of heart failure. Eur J Heart Fail 20(10):1417–1425
Pinney JH, Whelan CJ, Petrie A et al (2013) Senile systemic amyloidosis: clinical features at presentation and outcome. J Am Heart Assoc 2:e000098
Gillmore JD, Maurer MS, Falk RH et al (2016) Non biopsy diagnosis of cardiac transthyretin amyloidosis. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.116.021612
Gonzalez-Lopez E, Gallego-Delgado M, Guzzo-Merello G et al (2015) Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur Heart J 36:2585–2594
Mohamed-Salem L, Santos-Mateo JJ, Sanchez-Serna J et al (2018) Prevalence of wild type ATTR assessed as myocardial uptake in bone scan in the elderly population. Int J Cardiol 270:192–196
Garcia-Pavia P, Rapezzi C, Adler Y, Arad M, Basso C, Brucato A, Burazor I, Caforio ALP, Damy T, Eriksson U, Fontana M, Gillmore JD, Gonzalez-Lopez E, Grogan M, Heymans S, Imazio M, Kindermann I, Kristen AV, Maurer MS, Merlini G, Pantazis A, Pankuweit S, Rigopoulos AG, Linhart A (2021) Diagnosis and treatment of cardiac amyloidosis. A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur J Heart Fail 23(4):512–526. https://doi.org/10.1002/ejhf.2140 (Epub 2021 Apr 7)
Hasib Sidiqi M, Gertz MA (2021) Immunoglobulin light chain amyloidosis diagnosis and treatment algorithm 2021. Blood Cancer J 11(5):90. https://doi.org/10.1038/s41408-021-00483-7
Oerlemans MIFJ, Rutten KHG, Minnema MC, Raymakers RAP, Asselbergs FW, de Jonge N (2019) Cardiac amyloidosis: the need for early diagnosis. Neth Heart J 27(11):525–536. https://doi.org/10.1007/s12471-019-1299-1
Fumagalli C, Zampieri M, Perfetto F, Zocchi C, Maurizi M (2021) Tassetti L et al Early diagnosis and outcome in patients with wild-type transthyretin cardiac amyloidosis. Mayo Clin Proc. https://doi.org/10.1016/j.mayocp.2021.04.021
Porcari A, Merlo M, Rapezzi C, Sinagra G (2020) Transthyretin amyloid cardiomyopathy: an uncharted territory awaiting discovery. Eur J Intern Med 82:7–15. https://doi.org/10.1016/j.ejim.2020.09.025 (Epub 2020 Oct 5)
Terré A, Deshayes S, Savey L, Grateau G, Georgin-Lavialle S (2020) Cause of death and risk factors for mortality in AA amyloidosis: a French retrospective study. Eur J Intern Med 82:130–132. https://doi.org/10.1016/j.ejim.2020.08.012 (Epub 2020 Aug 14)
Gertz MA, Kyle RA, Greipp PR (1991) Response rates and survival in primary systemic amyloidosis. Blood 77:257–262
Kyle RA, Gertz MA (1995) Primary systemic amyloidosis: clinical and laboratory features in 474 cases. Semin Hematol 32:45–59
Katzmann JA (2009) Screening panels for monoclonal gammopathies: time to change. Clin Biochem Rev 30:105–111
Palladini G, Russo P, Bosoni T, Verga L, Sarais G et al (2009) Identification of amyloidogenic light chains requires the combination of serum-free light chain assay with immunofixation of serum and urine. Clin Chem 55:499–504
Palladini G, Jaccard A, Milani P, Lavergne D, Foli A et al (2017) Circulating free light chain measurement in the diagnosis, prognostic assessment and evaluation of response of AL amyloidosis: comparison of Freelite and N latex FLC assays. Clin Chem Lab Med 26:1734–1743
Hutchison CA, Plant T, Drayson M, Cockwell P, Kountouri M et al (2008) Serum free light chain measurement aids the diagnosis of myeloma in patients with severe renal failure. BMC Nephrol 9:11
Palladini G, Campana C, Klersy C, Balduini A, Vadacca G et al (2003) Serum N-terminal pro-brain natriuretic peptide is a sensitive marker of myocardial dysfunction in AL amyloidosis. Circulation 107:2440–2445. https://doi.org/10.1161/01.CIR.0000068314.02595.B2 (Epub 2003 Apr 28)
Wechalekar AD, Gillmore JD, Wassef N, Lachmann HJ, Whelan C, Hawkins PN (2011) Abnormal N-terminal fragment of brain natriuretic peptide in patients with light chain amyloidosis without cardiac involvement at presentation is a risk factor for development of cardiac amyloidosis. Haematologica 96:1079–1080
Ma KK, Ogawa T, de Bold AJ (2004) Selective upregulation of cardiac brain natriuretic peptide at the transcriptional and translational levels by pro-inflammatory cytokines and by conditioned medium derived from mixed lymphocyte reactions via p38 MAP kinase. J Mol Cell Cardiol 36:505–513
Shi J, Guan J, Jiang B et al (2010) Amyloidogenic light chains induce cardiomyocyte contractile dysfunction and apoptosis via a non-canonical p38alpha MAPK pathway. Proc Natl Acad Sci USA 107(9):4188–4193
Merlini G, Palladini G (2012) Differential diagnosis of monoclonal gammopathy of undetermined significance. Hematol Am Soc Hematol Educ Program 2012:595–603
Palladini G, Basset M, Milani P, Varettoni M et al (2017) Biomarker- based screening of organ dysfunction in patients with MGUS allows early diagnosis of AL amyloidosis. Blood 130:1760
Gertz MA, Comenzo R, Falk RH, Fermand JP, Hazenberg BP et al (2005) Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18–22 April 2004. Am J Hematol 79:319–328
Palladini G, Foli A, Milani P, Russo P, Albertini R, Lavatelli F, Obici L, Perlini S, Moratti R, Merlini G (2012) Best use of cardiac biomarkers in patients with AL amyloidosis and renal failure. Am J Hematol 87:465–471
Perfetto F, Bergesio F, Grifoni E, Fabbri A, Ciuti G et al (2016) Different NT-proBNP circulating levels for different types of cardiac amyloidosis. J Cardiovasc Med 17:810–817
Grandis M, Obici L, Luigetti M, Briani C, Benedicenti F et al (2020) Recommendations for pre-symptomatic genetic testing for hereditary transthyretin amyloidosis in the era of effective therapy: a multicenter Italian consensus. Orphanet J Rare Dis 15:348
Dispenzieri A, Gertz MA, Kyle RA et al (2004) Serum cardiac troponins and N-terminal pro-brain natriuretic peptide: a staging system for primary systemic amyloidosis. J Clin Oncol 22:3751–3757
Wechalekar AD, Schonland SO, Kastritis E, Gillmore JD, Dimopoulos MA et al (2013) A European collaborative study of treatment outcomes in 346 patients with cardiac stage III AL amyloidosis. Blood 121:3420–3427
Kumar S, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK et al (2012) Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J Clin Oncol 30:989–995
Kumar SK, Gertz MA, Dispenzieri A (2019) Validation of Mayo Clinic staging system for light chain amyloidosis with high-sensitivity troponin. J Clin Oncol 37:171–173
Dittrich T, Benner A, Kimmich C, Siepen FAD, Veelken K et al (2019) Performance analysis of AL amyloidosis cardiac biomarker staging systems with special focus on renal failure and atrial arrhythmia. Haematologica 104:1451–1459
Lilleness B, Ruberg FL, Mussinelli R, Doros G, Sanchorawala V (2019) Development and validation of a survival staging system incorporating BNP in patients with light chain amyloidosis. Blood 133:215–223
Abdallah N, Dispenzieri A, Muchtar E, Buadi FK, Kapoor P et al (2021) Prognostic restaging after treatment initiation in patients with AL amyloidosis. Blood Adv 5:1029–3601
Barosi G, Boccadoro M, Cavo M, Corradini P, Marchetti M, Massaia M, Merlini G, Tosi P, Tura S; Italian Society of Hematology; Italian Society of Experimental Hematology; Italian Group for Bone Marrow Transplantation (2004) Management of multiple myeloma and related-disorders: guidelines from the Italian Society of Hematology (SIE), Italian Society of Experimental Hematology (SIES) and Italian Group for Bone Marrow Transplantation (GTMO). Haematologica 89:717–741
Gertz M, Lacy M, Dispenzieri A, Hayman S, Kumar S et al (2008) Troponin T level as an exclusion criterion for stem cell transplantation in light-chain amyloidosis. Leuk Lymphoma 49:36–41
Gertz MA, Lacy MQ, Dispenzieri A, Kumar SK, Dingli D et al (2013) Refinement in patient selection to reduce treatment-related mortality from autologous stem cell transplantation in amyloidosis. Bone Marrow Transpl 48:557–561
Maurer MS, Elliott P, Comenzo R, Semigran M, Rapezzi C (2017) Addressing common questions encountered in the diagnosis and management of cardiac amyloidosis. Circulation 135:1357–1377. https://doi.org/10.1161/CIRCULATIONAHA.116.024438
Bartolini S, Baldasseroni S, Fattirolli F, Silverii MV, Piccioli L, Perfettop F, Marchionni N, Di Mario C, Martone R, Taborchi G, Morini S, Vignini E, Cappelli F (2021) Poor right ventricular function is associated with impaired exercise capacity and ventilatory efficiency in transthyretin cardiac amyloid patients. Intern Emerg Med 16(3):653–660. https://doi.org/10.1007/s11739-020-02474-1 (Epub 2020 Sep 12)
Gospodinova M, Sarafov S, Chamova T, Kirov A, Todorov T, Nakov R, Todorova A, Denchev S, Tournev I (2020) Cardiac involvement, morbidity and mortality in hereditary transthyretin amyloidosis because of p.Glu89Gln mutation. J Cardiovasc Med (Hagerstown) 21(9):688–695. https://doi.org/10.2459/JCM.0000000000001036
Grogan M, Scott CG, Kyle RA, Zeldenrust SR, Gertz MA et al (2016) Natural history of wild-type transthyretin cardiac amyloidosis and risk stratification using a novel staging system. J Am Coll Cardiol 68:1014–1020
Gillmore JD, Damy T, Fontana M, Hutchinson M, Lachmann HJ et al (2017) A new staging system for cardiac transthyretin amyloidosis. Eur Heart J 39:2799–2806
Cappelli F, Martone R, Gabriele M, Taborchi G, Morini S et al (2020) Biomarkers and prediction of prognosis in transthyretin-related cardiac amyloidosis: direct comparison of two staging systems. Can J Cardiol 36:424–431
Cheng RK, Levy WC, Vasbinder A, Teruya S, De Los SJ et al (2020) Diuretic dose and NYHA functional class are independent predictors of mortality in patients with transthyretin cardiac amyloidosis. JACC CardioOncol 2:414–424
Palladini G, Dispenzieri A, Gertz MA, Kumar S, Wechalekar A et al (2012) New criteria for response to treatment in immunoglobulin light chain amyloidosis based on free light chain measurement and cardiac biomarkers: impact on survival outcomes. J Clin Oncol 30:4541–4549
Dittrich T, Bochtler T, Kimmich C, Becker N, Jauch A et al (2017) AL amyloidosis patients with low amyloidogenic free light chain levels at first diagnosis have an excellent prognosis. Blood 130:632–642
Sidana S, Tandon N, Dispenzieri A, Gertz MA, Buadi FK et al (2018) Clinical presentation and outcomes in light chain amyloidosis patients with non-evaluable serum free light chains. Leukemia 32:729–735
Milani P, Basset M, Russo F, Foli A, Merlini G (2017) Patients with light chain (AL) amyloidosis and low free light chain burden have distinct clinical features and outcome. Blood 130:625–631
Palladini G, Schönland SO, Sanchorawala V, Kumar S, Wechalekar A, Hegenbart U, Milani P, Ando Y, Westermark P, Dispenzieri A, Merlini G (2021) Clarification on the definition of complete haematologic response in light-chain (AL) amyloidosis. Amyloid 28(1):1–2. https://doi.org/10.1080/13506129.2020.1868810 (Epub 2021 Jan 7)
Lilleness B, Doros G, Ruberg FL, Sanchorawala V (2020) Establishment of brain natriuretic peptide-based criteria for evaluating cardiac response to treatment in light chain (AL) amyloidosis. Br J Haematol 188:424–427127
Palladini G, Milani P, Merlini G (2020) Management of AL amyloidosis in 2020. Blood 136:2620–2627. https://doi.org/10.1182/blood.2020006913
Palladini G, Barassi A, Klersy C, Pacciolla R, Milani P et al (2016) The combination of high-sensitivity cardiactroponin T (hs-cTnT) at presentation and changes in N-terminal natriuretic peptide typeB (NT-proBNP) after chemotherapy best predicts survival in AL amyloidosis. Blood 116:3426–3431
Palladini G, Lavatelli F, Russo P, Perlini S, Perfetti V et al (2006) Circulating amyloidogenic free light chains and serum N-terminal natriuretic peptide type B decrease simultaneously in association with improvement of survival in AL. Blood 107:3854–3858
Kastritis E, Roussou M, Gavriatopoulou M, Migkou M, Kalapanida D et al (2015) Long-term outcomes of primary systemic light chain (AL) amyloidosis in patients treated upfront with bortezomib or lenalidomide and the importance of risk adapted strategies. Am J Hematol 90:E60–E65
Palladini G, Kastritis E, Maurer MS, Zonder J, Minnema MC et al (2020) Daratumumab plus CyBorD for patients with newly diagnosed AL amyloidosis: safety run-in results of ANDROMEDA. Blood 136:71–80
Palladini G, Barassi A, Klersy C, Pacciolla R, Milani P et al (2010) The combination of high-sensitivity cardiac troponin T (hs-cTnT) at presentation and changes in N-terminal natriuretic peptide type B (NT-proBNP) after chemotherapy best predicts survival in AL amyloidosis. Blood 116:3426–3430
Kaufman GP, Dispenzieri A, Gertz MA, Lacy MQ, Buadi FK et al (2015) Kinetics of organ response and survival following normalization of the serum free light chain ratio in AL amyloidosis. Am J Hematol 90:181–186
Dispenzieri A, Dingli D, Kumar SK, Rajkumar SV, Lacy MQ et al (2010) Discordance between serum cardiac biomarker and immunoglobulin-free light-chain response in patients with immunoglobulin light-chain amyloidosis treated with immune modulatory drugs. Am J Hematol 85:757–759
Sidana S, Milani P, Binder M, Basset M, Tandon N et al (2020) A validated composite organ and hematologic response model for early assessment of treatment outcomes in light chain amyloidosis. Blood Cancer J 10:41. https://doi.org/10.1038/s41408-020-0306-5
Ciliberti G, Urbinati A, Barbarossa A, Stronati G, Silenzi M, Principi S, Falanga U, Capucci A, Casella M, Dello Russo A, Guerra F (2021) Compassionate drug use for patients with transthyretin amyloid cardiomyopathy. J Cardiovasc Med (Hagerstown) 22(10):792–794. https://doi.org/10.2459/JCM.0000000000001192
Emdin M, Aimo A, Rapezzi C, Fontana M, Perfetto F, Seferovic PM, Barison A, Castiglione V, Vergano G, Giannoni A et al (2019) Treatment of cardiac transthyretin amyloidosis: an update. Eur Heart J 40:3699–3706
Buxbaum J, Anan I, Suhr O (2010) Serum transthyretin levels in Swedish TTR V30M carriers. Amyloid 17:83–85. https://doi.org/10.3109/13506129.2010.483118
Skinner M, Connors LH, Rubinow A, Libbey C, Sipe JD et al (1985) Lowered prealbumin levels in patients with familial amyloid polyneuropathy(FAP) and their non-affected but at risk relatives. Am J Med Sci 289:17–21
Coelho T, Chorão R, Sousa A, Alves A, Torres MF et al (1996) Compound heterozygotes of transthyretin Met30 and transthyretin Met119 are protected from the devastating effects of familial amyloid polyneuropathy. J Neuromusc Disord 6:S20
Judge DP, Heitner SB, Falk RH, Maurer MS, Shah SJ et al (2019) Transthyretin stabilization by AG10 in symptomatic transthyretin amyloid cardiomyopathy. J Am Coll Cardiol 74:285–295
Adams D, Gonzalez-Duarte A, O’Riordan WD, Yang CC, Ueda M et al (2018) Patisiran, an RNAi therapeutic, for hereditary transthyretin amyloidosis. N Engl J Med 379:11–21
Benson MD, Waddington-Cruz M, Berk JL, Polydefkis M, Dyck PJ, Wang AK et al (2018) Inotersen treatment for patients with hereditary transthyretin amyloidosis. N Engl J Med 379(1):22–31
Law S, Petrie A, Chacko L, Cohen OC, Ravichandran S, Gilbertson JA, Rowczenio D, Wechalekar AD, Martinez-Naharro A, Lachmann HJ, Whelan CJ, Hutt DF, Hawkins PN, Fontana M, Gillmore JD (2021) Change in N-terminal pro-B-type natriuretic peptide at 1 year predicts mortality in wild-type transthyretin amyloid cardiomyopathy. Heart. https://doi.org/10.1136/heartjnl-2021-319063(Epub ahead of print)
Kastritis E, Papassotiriou I, Merlini G, Milani P, Terpos E et al (2018) Growth differentiation factor-15 is a new biomarker for survival and renal outcomes in light chain amyloidosis. Blood 131:1568–1575
Dispenzieri A, Gertz MA, Saenger A, Kumar SK, Lacy MQ et al (2015) Soluble suppression of tumorigenicity 2 (sST2), but not galactin-3, adds to prognostication in patients with systemic AL amyloidosis independent of NT-proBNP and troponin T. Am J Hematol 90:524–528
Zhang KW, Miao J, Mitchell JD, Alvarez-Cardona J, Tomasek K et al (2020) Plasma hepatocyte growth factor for diagnosis and prognosis in light chain and transthyretin cardiac amyloidosis. JACC Cardio Oncol 2:56–66
Palladini G, Barassi A, Perlini S, Milani P, Foli A et al (2011) Midregional proadrenomedullin (MR-proADM) is a powerful predictor of early death in AL amyloidosis. Amyloid 18:216–221
Kastritis E, Papassotiriou I, Terpos E, Roussou M, Gavriatopoulou M et al (2016) Clinical and prognostic significance of serum levels of von Willebrand factor and ADAMTS-13 antigens in AL amyloidosis. Blood 128:405–409
Weng L, Spencer BH, SoohHoo PT, Connors LH, O’Hara CJ, Seldin DC (2011) Dysregulation of miRNAs in AL amyloidosis. Amyloid 18:128–135
Fishov H, Muchtar E, Salmon-Divon M, Dispenzieri A, Shpilberg O, Hershkovitz-Rokah O (2020) The role of MicroRNA in the pathogenesis of AL amyloidosis. In: XVII International symposium on amyloidosis Tarragona Spain 14th–18th September 2020, PM026, pp 105–106
Derda AA, Pfanne A, Bär C, Schimmel K, Kennel PJ et al (2018) Blood-based microRNA profiling in patients with cardiac amyloidosis. PLoS ONE 13(10):e0204235. https://doi.org/10.1371/journal.pone.0204235
Vita GL, Aguennouz M, Polito F, Oteri R, Russo M, Gentile L et al (2020) Circulating microRNAs profile in patients with transthyretin variant amyloidosis frontiers in molecular. Neuroscience 13:102–111. https://doi.org/10.3389/fnmol.2020.00102
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no conflict of interest.
Human and animal rights statement and Informed consent
The manuscript is not a clinical study, but an up to date review aimed to summarize the current clinical use of circulating biomarkers for the management of cardiac amyloidosis, collecting and discussing the current literature on this topic. Thus, the authors have not directly involved humans and/or animals in the drafting of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Perfetto, F., Zampieri, M., Fumagalli, C. et al. Circulating biomarkers in diagnosis and management of cardiac amyloidosis: a review for internist. Intern Emerg Med 17, 957–969 (2022). https://doi.org/10.1007/s11739-022-02958-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-022-02958-2