Abstract
The beard is a well-known cause of difficult mask ventilation due to excessive air leaks. Various techniques have been proposed to overcome this difficulty, such as applying a gel on the mask edge. Our objective was to determine whether the gel technique will improve ventilation and to assess the comfort of the provider. A randomized crossover design was conducted to assess the efficacy of gel in a bearded simulation model. Respiratory therapists (RT) were recruited by convenience sampling to hold the mask using a two-handed technique for a two-minute ventilation session. During the session, the ventilator provided a fixed Tidal Volume (TV) of 550 mL and a respiratory rate of 12 per minute, and the simulated model measured the received volumes. We compared the median TV and number of failed ventilation attempts with or without the gel. The comfort level while using the gel was assessed with constructed questions. We recruited 74 respiratory therapists working in Riyadh city. More than half of the participants had more than 5 years experience. The median tidal volume for standard mask ventilation without the gel was 283 mL [interquartile range (IQR) 224, 327], whereas that with the gel was 467 mL [451, 478], respectively (p < 0.01). The number of successful ventilations was recorded out of 24 breaths during the 2-min ventilation period for each technique; the proportion of successful ventilations increased significantly by 65% (95% CI 51–75%, p < 0.01) with the gel. In addition, only nine participants believed the technique was not comfortable, while the remaining individuals found it comfortable or natural. In our bearded simulation model, applying the gel significantly improved ventilation without negatively affecting comfort. Further studies and education are encouraged in the field of basic airway management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Noninvasive mask ventilation has been defined as the flow of oxygenated air from a positive pressure source to the patient’s lungs through a mask [1]. In all types of mask ventilation, whether manual or mechanical, a fitted mask is a fundamental factor for adequate ventilation.
Mask ventilation is considered the most important skill for airway management to improve oxygenation and carbon dioxide (CO2) clearance, reduce the work of breathing or relieve respiratory distress. There are two issues guiding the algorithms of difficult airway management: inability to intubate and inability to ventilate [2]. Ventilation is the backup plan for a difficult or failed airway, which can save the patient from serious consequences, such as hypoxic brain injury or even death [1, 3]. In addition, mask ventilation can optimize the preoxygenation condition in an apneic patient or a patient with severe respiratory failure [4, 5]. Over the last few years, there have been many publications and devices invented that focus on improving the endotracheal intubation procedure, but unfortunately, less effort has been made to improve the management of difficult ventilation.
The reported incidence of difficult mask ventilation in the anesthesia literature has ranged from 1.4–9% of the adult population [6,7,8]. However, in the emergency department, the incidence is approximately 46% of total mask ventilation attempts and probably more in the pre-hospital setting, given suboptimal situations [9]. Kheterpal et al. [8] conducted a prospective observational study in 22,660 mask ventilation attempts for adult patients during general anesthesia in the operation room, aiming to evaluate the incidence and the predictors of difficult mask ventilation. They found that (1.4%) of the patients were difficult to ventilate, and (0.16%) were impossible to ventilate. In addition, the study concluded that the only modifiable predictor of difficult mask ventilation is the beard, which can be shaved before the procedure.
The beard is a well-known independent predictor of difficult mask ventilation, as it causes excessive leaks between the hairs and the mask edge [6,7,8, 10]. In the literature, many methods have been suggested by experts to overcome this problem without shaving the beard. Gourdin et al. [11] suggested adding a viscous gel on the mask edge to impregnate between the hairs and mask, which could improve the mask seal and ventilation. Others have claimed that the gel will form a slippery interface and might impair controlling the mask during ventilation [12]. Another method suggested is to use a large-size transparent Tegaderm dressing to be applied over the face, with the outer edges extending over the beard to the neck, and then creating an opening through the mouth for ventilation [12]. An additional method has been described by Rao et al. [13], suggesting assessing the patency of the nostrils, inserting a lubricated nasal airway through the most patent nostril, using a suitable-sized toddler mask and ventilating through the nose. However, none of the previously suggested methods assessed the effectiveness in improving the ventilation.
All the previously described methods seem to be feasible in controlled situations such in the operation room, but in an emergency situation or in the prehospital setting, a simple and quick method with readily available types of equipment is needed. In terms of feasibility and applicability, we believe that the most appropriate technique is the gel technique. Therefore, this study aimed to assess the efficacy of gel methods in improving mask ventilation in a manikin with a beard. The secondary outcome of interest is to compare the provider comfort during ventilation with or without the gel.
Methods
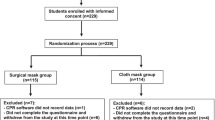
This study was conducted in the simulation center at Prince Sultan Collage for Emergency Medical Services. Invitations were made to respiratory therapists (RTs) working in Riyadh city to visit the center. The invitations were sent through social media for RTs in Riyadh. The targeted number of participants was 50 based on similar studies on ventilation with similar context [14, 15]. In addition, the objective of the study was another reason for choosing this number, as 50 was seen as a sufficient number to assess the efficiency of the proposed method. Respiratory therapists were chosen since they were accustomed to handle basic airway management. In addition, they are the benchmark for other health care professionals when it comes to ventilation. The eligibility criteria were current work experience and a position as an RT clinically working in Riyadh city. Seventy-five participants joined the study; one was excluded since he worked in administrative duty (Fig. 1).
Mask ventilation is a complex process that can be affected by many confounders, including patient-related factors, healthcare provider experience, hand technique and equipment factors [1, 16]. To reduce these sources of potential bias, the mask ventilation operation was standardized: the same mechanical ventilator machine was used, with constant sitting, and the same manikin that can measure the delivered tidal volumes was used for all trials. In addition, the same equipment and techniques were standardized for controlling the mask. We glued the inner surface of the artificial beard to the mannequin to prevent movement and leakage beneath the beard.
The three most important characteristics of the mannequin we used are as follows. First, the manikin’s skin and face should be similar to the softness and the smoothness of normal skin. Secondly, the manikin’s lungs should resemble normal lungs in maintaining elasticity during expansion without leaks or sudden obstructions in flow. Finally, the manikin should measure the received volumes correctly. We used intubation with ventilating through and mechanical ventilation to check the elasticity and accuracy of the measurement and found that the most suitable manikin in our simulation center is the RespiTrainer Advance unit, which is manufactured by IngMar Medical. The unit has feedback training system software that records all aspects of ventilation.
The study followed a randomized crossover design. The procedure was initiated by RTs signing a consent form and then completing a constructed questionnaire that gathered information from the participants about demographics and previous experience. Then, the participants held the masks using the two-handed technique with which they were comfortable: either the double C-E technique, in which each index and thumb finger form a C-shape over the mask, while the remaining fingers lift the mandible bilaterally; or the V-E technique, in which the thumbs and thenar eminence are placed over each side of the mask while the remaining fingers lift the mandible, the ventilator provided a fixed volume..
Randomly, the participants started with or without the gel for 2 min, followed by a rest for 2 min, and then the alternate strategy. Ultrasound gel (water-soluble) was applied by the investigator on the edge of the mask as illustrated (Fig. 2). The ventilator (Zoll Eagle II Ventilator) was programmed in continuous mandatory ventilation mode to deliver a fixed TV of 550 mL at a rate of 12 breaths per minute, and the manikin measured the TV. The investigator entered the data recorded by the manikin’s feedback training system software, such as the recorded mean TV and the number of inadequate TVs (TV < 300 mL). The participants were blinded to the recorded measures, and the alarm system of the ventilator was muted. After finishing the ventilation sessions, a second questionnaire to assess the comfort was completed by the participant, using a five-point Likert scale.
Outcome parameters
Manikin-based studies that aimed to evaluate the ventilation have used different methods to assess the efficacy of ventilation [1, 16]. We believe volume measurements are physiologically related to ventilation and easier to interpret than pressure measurements. Because each measurement method has some limitations, we used two methods for the assessment. The first was the overall median value of measured TV for the two-minute session. The second method was a breath-by-breath analysis in which each ventilatory cycle was measured and analyzed independently to detect the number of inadequate TVs delivered over the session. Inadequate TV was defined as less than 300 mL [16].
Statistical analysis
The Shapiro–Wilk test was used to examine data distribution. As the data of the main outcome did not meet the assumption of normality (p < 0.004 for mask without gel, p < 0.001 for mask with gel), we used a nonparametric Wilcoxon signed-rank test to determine the statistical significance. Subgroup analysis was conducted for sex, height and years of experience. Subsequently, in the subgroup analysis comparing two independent samples, we used the Mann–Whitney U test. Significance was set as a p value < 0.05. StataCorp 2017 (Stata Statistical Software Release 15, College Station, TX, StataCorp, LLC) was used to perform all the analyses.
Results
Seventy-four respiratory therapists (42 male, 32 female) randomly performed ventilation on our simulated bearded model using a face mask with gel and a face mask without gel (Table 1).
More than half of the participants had been working as respiratory therapists for more than 5 years, and the majority were working in the intensive care unit (ICU) (Table 1).
Before using gel, participants’ previous knowledge about the use of gel to smooth patients’ beards was assessed by a self-completed questionnaire; approximately 97% of the participants had no previous knowledge of the technique.
Applying gel around the BVM mask on a bearded manikin resulted in a significantly higher median tidal volume compared to face mask ventilation without gel in a two-minute period, with a total of 24 breaths (283 mL [IQR 224, 327], 467 [451, 478], respectively) (p value of < 0.05) (Table 2).
When stratified by years of experience, the median tidal volume did not change significantly after applying gel between participants with more than 5 years of experience and participants with less than or equal to 5 years of experience (p value = 0.736). However, in both groups, the ventilated median tidal volume was higher with gel than without gel (Table 2).
Without the gel, males achieved a significantly higher median tidal volume than females (p value = 0.007); however, with gel, the achieved median tidal volume was almost equal between males and females (467 mL [IQR 446, 477], 468 [IQR 457, 484], respectively). Moreover, the difference between medians was not significantly different between males and females (p value = 0.292) (Fig. 3 a, b).
Without the gel, participants ≤ 165 cm (cm) in height achieved a median tidal volume of 262 mL [IQR 199, 326], and for participants > 165 cm in height, the median tidal volume was 308 mL [IQR 240, 338] (Table 2). However, with the gel, the difference in median tidal volume stratified by height decreased, as the median for participants ≤ 165 cm in height was 467 mL [IQR 454, 483], and that for participants > 165 cm in height was 469 mL [IQR 446, 477].
The numbers of successful ventilations were recorded out of 24 breaths during the 2-min ventilation period for each technique; the proportion of successful ventilations increased significantly by 65% (95% CI 51–75%) (p < 0.001) with the gel.
Participants answered questions about the comfort level of ventilation with the gel on the bearded manikin compared to ventilation without gel. Forty-four of the participants believed that it was comfortable or very comfortable to use gel on bearded patients, whereas nine participants believed it was not comfortable, and twenty-three responses were “natural” (Fig. 4).
Discussion
To the best of our knowledge, this is the first study aimed to assess a technique to improving difficult ventilation in bearded patients. Our study included seventy-four respiratory therapists, more than half of them had more than 5 years experience who we believe can be considered the benchmark for basic airway management or ventilation. The median tidal volume for standard mask ventilation without the gel was 283 mL, whereas that with the gel was 467 mL, (p < 0.01). Our study revealed that applying gel on the edge of the facemask significantly improved both the TV and the number of successful ventilations.
The questionnaire completed by the participants revealed that most RTs did not have any previous knowledge about utilizing gel with bearded patients. Only six participants reported that adding the gel was not comfortable during the ventilation, while the majority of them found it comfortable.
In our present study, the results showed that the use of mask ventilation in this simulated beard model resulted in inadequate ventilation due to excessive air leakage. Without the gel, the median TV received was 284 mL with the ventilator set to provide 550 mL, indicating a greater than 50% leak. This is consistent with other studies that named beards as a cause of excessive leakage [6,7,8, 10]. Moreover, in prolonged ventilation situations, using a face mask may be strenuous and can also be associated with a higher amount of leakage [17].
The characteristics of participants showed some impact on the results. Without gel, the females and participants shorter than or equal to 165 cm delivered less effective ventilation. This finding is consistent with previous studies that reported that shorter operators or females may provide lower TV during ventilation [18]. However, after adding the gel, both groups achieved successful ventilation, regardless of their physical characteristics. This could be an indicator that using the gel can minimize the variation in the delivered tidal volume, which may be caused by the operator’s characteristics [14].
Occasionally, the health care provider might try to overcome leakages by forcefully bagging the patient. If this technique is effective, it may harm the patient by causing barotrauma, or the air can insufflate the stomach. Moreover, this technique might cause fatigue for the provider and decrease the operator’s ability to feel resistance or lung compliance during the ventilation. The efficacy and the simplicity of the gel technique make it easily applicable in all emergency cases, whether inside or outside the hospital. Furthermore, the gel by decreasing the air leak might reduce the spread of contagious infection [19]. However, further investigations are required to confirm the hypothesis. We recommend adding the gel to all difficult mask ventilations of bearded patients. We encourage further investigation on the gel technique with real patients or in fresh cadaver studies. In addition, we recommend enriching the teaching of the basic airway courses and the undergraduate curriculum by adding the techniques that improve the difficult mask ventilation of specific groups of patients, such as bearded, edentulous, and obese patients. We suggest that manufacturer’s incorporate a special facemask material that improves the seal for bearded patients.
In conclusion, in our bearded simulation model, applying the gel significantly improved ventilation without negatively affecting the provider comfort. Moreover, adding the gel could minimize the ventilation variation caused by differences in the operators’ characteristics. Further studies and education are encouraged in the field of basic airway management.
Data availability
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
- RT:
-
Respiratory therapists
- TV:
-
Tidal volume
- mL:
-
Milliliter
- IQR:
-
Interquartile range
- CI:
-
Confidence interval
- BVM:
-
Bag valve mask
- CO2 :
-
Carbon dioxide
- ICU:
-
Intensive care unit
- Cm:
-
Centimeter
References
Saddawi-Konefka D, Hung SL, Kacmarek RM, Jiang Y (2015) Optimizing mask ventilation: literature review and development of a conceptual framework. Respir Care 60(12):1834–1840. https://doi.org/10.4187/respcare.04183
Apfelbaum JL, Hagberg CA, Caplan RA et al (2013) Practice guidelines for management of the difficult airway: an updated report by the American society of anesthesiologists task force on management of the difficult airway. Anesthesiology 118(2):251–270. https://doi.org/10.1097/ALN.0b013e31827773b2
Hagberg CA, Connis RT (2016) Difficult airway society 2015 guidelines for the management of unanticipated difficult intubation in adults: not just another algorithm. Br J Anaesth 116(2):309. https://doi.org/10.1093/bja/aev460
Mort TC (2005) Preoxygenation in critically ill patients requiring emergency tracheal intubation. Crit Care Med 33(11):2672–2675. https://doi.org/10.1097/01.ccm.0000187131.67594.9e
Ramkumar V, Dinesh E, Shetty SR et al (2016) All India difficult airway association 2016 guidelines for the management of unanticipated difficult tracheal intubation in obstetrics. Indian J Anaesth 60(12):899–905. https://doi.org/10.4103/0019-5049.195482
Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, Coriat P, Riou B (2000) Prediction of difficult mask ventilation. Anesthesiology 92(5):1229–1236. https://doi.org/10.1097/00000542-200005000-00009
Cattano D, Killoran PV, Cai C, Katsiampoura AD, Corso RM, Hagberg CA (2014) Difficult mask ventilation in general surgical population: observation of risk factors and predictors. F1000Res 3:204. https://doi.org/10.12688/f1000research.5131.1
Kheterpal S, Han R, Tremper KK, Shanks A, Tait AR, O’Reilly M, Ludwig TA (2006) Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology 105(5):885–891. https://doi.org/10.1097/00000542-200611000-00007
Lee S, Chien D, Huang M, Huang C, Shih S, Wu K, Ku H, Chang W (2017) Patient-specific factors associated with difficult mask ventilation in the emergency department. Int J Gerontol 11(4):263–266. https://doi.org/10.1016/j.ijge.2017.02.004
Kheterpal S, Healy D, Aziz MF et al (2013) Incidence, predictors, and outcome of difficult mask ventilation combined with difficult laryngoscopy: a report from the multicenter perioperative outcomes group. Anesthesiology 119(6):1360–1369. https://doi.org/10.1097/aln.0000435832.39353.20
Gourdin MJ, Dransart CJ, Ducombs O, Dubois PE (2005) Improved face mask ventilation in the bearded patient. Eur J Anaesthesiol 22(11):894. https://doi.org/10.1017/s0265021505251505
Sinha AC, Purohit M, Singh PM, Goudra BG (2013) Difficult mask ventilation: tegaderm for sealing a patient’s fate! J Clin Anesth 25(8):679–680. https://doi.org/10.1016/j.jclinane.2013.07.009
Rao V, Kosik E, Ganta R, Windrix C (2011) Mask ventilation in edentulous and bearded patients. Anesth Analg 112(6):1513–1514. https://doi.org/10.1213/ANE.0b013e318215d34c
Lim JS, Cho YC, Kwon OY, Chung SP, Yu K, Kim SW (2012) Precise minute ventilation delivery using a bag-valve mask and audible feedback. Am J Emerg Med 30(7):1068–1071. https://doi.org/10.1016/j.ajem.2011.07.003
Marjanovic N, Le Floch S, Jaffrelot M, L’Her E (2014) Evaluation of manual and automatic manually triggered ventilation performance and ergonomics using a simulation model. Respir Care 59(5):735–742. https://doi.org/10.4187/respcare.02557
Khoury A, De Luca A, Sall FS, Pazart L, Capellier G (2015) Performance of manual ventilation: how to define its efficiency in bench studies? A review of the literature. Anaesthesia 70(8):985–992. https://doi.org/10.1111/anae.13097
Kurola J, Harve H, Kettunen T, Laakso JP, Gorski J, Paakkonen H, Silfvast T (2004) Airway management in cardiac arrest–comparison of the laryngeal tube, tracheal intubation and bag-valve mask ventilation in emergency medical training. Resuscitation 61(2):149–153. https://doi.org/10.1016/j.resuscitation.2004.01.014
Na JU, Han SK, Choi PC, Cho JH, Shin DH (2013) Influence of face mask design on bag-valve-mask ventilation performance: a randomized simulation study. Acta Anaesthesiol Scand 57(9):1186–1192. https://doi.org/10.1111/aas.12169
Brewster DJ, Chrimes N, Do TB et al (2020) Consensus statement: safe airway society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. Med J Aust 212(10):472–481. https://doi.org/10.5694/mja2.50598
Acknowledgements
The authors gratefully acknowledge all the personnel who helped in the data collection: Hatem Altalhi, Mustafa Alhumaidan and Turki Alharbi. We would like to thank the Simulation Unit at Prince Sultan College of EMS for their cooperation and for providing us with their equipment despite their busy teaching schedules. The authors extend their appreciation to the Deanship of Scientific Research at King Saud University for supporting this work through research group no.RG-1441-518.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SMA was involved in conceptualization; MZA, MAA and SA were involved in data curation; AM and RNA were involved in formal analysis; AMM was involved in funding acquisition; SMA, RNA MZA and MAA were involved in investigation; SMA, AM and RNA were involved in methodology; SMA was involved in project administration; SMA, MZA, MAA, SA and AMM were contributed to resources; SMA was involved in supervision; AM was involved in validation; AM and RNA were involved in writing—original draft; AMM was involved in writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Statement of human and animal rights
Ethical approval was provided by the institutional Review Board (IRB) and the ethical research committee at King Saud University hospital (research project number 19/0886/IRB).
Informed consent
Every participant has signed a consent form to be a part of the study.
Consent for publication
Consent for publication has been obtained from the participants based on King Saud University consent form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Althunayyan, S.M., Mubarak, A.M., Alotaibi, R.N. et al. Using gel for difficult mask ventilation on the bearded patients: a simulation-based study. Intern Emerg Med 16, 1043–1049 (2021). https://doi.org/10.1007/s11739-020-02547-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-020-02547-1