Abstract
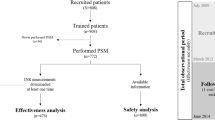
Over the last years, direct oral anticoagulants (DOACs) have radically changed and simplified the therapeutic approach and management of patients on anticoagulant therapy. For these patients, international guidelines recommend to set up a regular follow-up (every 1–6 months) to re-enforce education, to ensure adequate adherence and persistence to treatment. In real-life setting, the application of the suggested follow-up regimens and incidence rates of thrombotic and bleeding complications related to the intensity of follow-up strategies has not been described. We conducted a multicentre, retrospective study at 4 Italian Thrombosis Centres to describe follow-up strategies of patients on DOACs treatment and to assess the incidence of bleeding and thrombotic complications. We enrolled 534 patients, with median follow-up 24 months: 52.1% had < 3 visits/year (group 1), while 47.9% required ≥ 3 visits/year (group 2). Mean age and gender were similar between the 2 groups, while severe anaemia (4.4% and 1.2%, p 0.03) and creatinine clearance < 50 mL/min were more common in group 2 (26.8% and 17.8%, p 0.02). The incidence of thromboembolic events was 3.9% in group 2 and 1.1% in group 1 (p 0.03). Major bleeding rates were non-significantly higher in group 2, whereas non-major bleeding rates occurred significantly more frequently in group 2 (26.6% and 18.7%, respectively, p 0.03). A tailored follow-up program is of critical importance to correctly manage patients on DOACs. A less intense follow-up management is feasible and safe for a substantial proportion of patients, provided they are carefully identified at specialized centres.
Similar content being viewed by others
References
Kearon C, Akl EA, Ornelas J et al (2016) Antithrombotic therapy for VTE disease. Chest guideline and expert panel report. Chest 149:315–352
Kirchhof P, Benussi S, Kotecha D et al (2016) 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur J Cardiothorac Surg 50(5):e1–e88
Steffel J, Verhamme P, Potpara TS, Albaladejo P et al (2018) The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J 39(16):1330–1393
Witt DM, Nieuwlaat R, Clark NP et al (2018) American Society of Hematology 2018 guidelines for management of venous thromboembolism: optimal management of anticoagulation therapy. Blood Adv 2(22):3257–3291
Prisco D, Ageno W, Becattini C et al (2017) Italian intersociety consensus on DOAC use in internal medicine. Intern Emerg Med 12(3):387–406
Parretti D, Grilli P, Bastiani F et al (2018) Documento di consensus SIMG-FCSA sulle corrette procedure di anticoagulazione. https://www.simg.it/Riviste/rivista_simg/2018/03_2018/completa.pdf
Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis (2005) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 3(4):692–694
Reinecke H, Brand E, Mesters R et al (2009) Dilemmas in the management of atrial fibrillation in chronic kidney disease. J Am Soc Nephrol 20:705–711
Rattazzi M, Villalta S, De Lucchi L et al (2017) Chronic kidney disease is associated with increased risk of venous thromboembolism recurrence. Thromb Res 160:32–37
Prisco D, Cenci C, Silvestri E et al (2015) Novel oral anticoagulants in atrial fibrillation: which novel oral anticoagulant for which patient? J Cardiovasc Med (Hagerstown) 16(7):512–519
Yamashita Y, Morimoto T, Amano H et al (2019) COMMAND VTE Registry Investigators. Influence of baseline anemia on long-term clinical outcomes in patients with venous thromboembolism: from the COMMAND VTE registry. J Thromb Thrombolysis 47(3):444–453
Hung SH, Lin HC, Chung SD (2015) Association between venous thromboembolism and iron-deficiency anemia: a population-based study. Blood Coagul Fibrinolysis 26(4):368–372
Lip GY, Nieuwlaat R, Pisters R et al (2010) Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro heart survey on atrial fibrillation. Chest 137:263–272
Cushman M (2007) Epidemiology and risk factors for venous thrombosis. Semin Hematol 44(2):62–69
Fang MC, Go AS, Hylek EM et al (2006) Age and the risk of warfarin-associated hemorrhage: the anticoagulation and risk factors in atrial fibrillation study. J Am Geriatr Soc 54(8):1231–1236
Fohtung RB, Novak E, Rich MW (2017) Effect of new oral anticoagulants on prescribing practices for atrial fibrillation in older adults. J Am Geriatr Soc 65:2405–2412
Sharma M, Cornelius VR, Patel JP et al (2015) Efficacy and harms of direct oral anticoagulants in the elderly for stroke prevention in atrial fibrillation and secondary prevention of venous thromboembolism: systematic review and meta-analysis. Circulation 132(3):194–204
Huisman MV, Rothman KJ, Paquette M et al (2017) GLORIA-AF investigators. The changing landscape for stroke prevention in AF: findings from the GLORIA-AF registry phase 2. J Am Coll Cardiol 69:777–785
Barnes GD, Lucas E, Alexander GC et al (2015) National trends in ambulatory oral anticoagulant use. Am J Med 128:1300–1305
Valencia D, Spoutz P, Stoppi J et al (2019) Impact of a direct oral anticoagulant population management tool on anticoagulation therapy monitoring in clinical practice. Ann Pharmacother 53(8):806–811
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Walter Ageno received honoraria from Boehringer Ingelheim, Bayer Pharmaceuticals, BMS-Pfizer, Daiichi-Sankyo, Portola, Aspen, Sanofi and research support from Bayer Pharmaceuticals, outside the submitted work. The authors report no other conflicts of interest in this work.
Statement of human and animal rights
The study is consistent with the principles of the Declaration of Helsinki of clinical research involving human subjects.
Informed consent
Due to the retrospective nature of the study, an informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fantoni, C., Bertù, L., Galliazzo, S. et al. Follow-up management of patients receiving direct oral anticoagulants. Intern Emerg Med 16, 571–580 (2021). https://doi.org/10.1007/s11739-020-02433-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-020-02433-w