Abstract
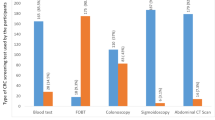
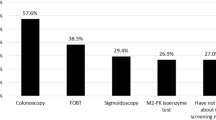
Screening and early diagnosis of cancer represent relatively recent tools in the long-lasting battle against tumors. If the American public opinion manifests its enthusiasm towards screening, the attitude of European is less well known. The purpose of the present study was to assess the level of knowledge and awareness of cancer screening (with particular emphasis on colorectal neoplasms) among middle-aged individuals. The study group consisted of 945 healthy individuals (489 men, 456 women, average age 57 ± 12.4 years) who were asked to answer a series of questions about cancer screening and surveillance through a questionnaire presented by trained residents. Each interview lasted 20–30 min. Middle-aged Italians of both sexes seem to be aware of the fact that cancer is a frequent disease; moreover, many of the interviewed subjects believe almost all neoplasms are incurable. Diet, style of life, other environmental factors and familial factors are fully appreciated as relevant risk factors. The exact meaning of prevention was clear to less than half of the subjects. When various cancer sites were analyzed, the existence of preventive measures was well known for breast, cervical and prostate tumors, but their role was less clear for colorectal cancer. Only a fraction of the interviewed individuals were willing to undergo screening; the main reasons for refusal were lack of usefulness and fear of results. Among various tests, ultrasound and endoscopy were usually carried out in the presence of symptoms. Finally, multivariate analysis showed that the two factors significantly associated with the decision to undergo screening procedures were increasing age and level of education. The results of the study suggest that middle-aged Italian individuals, predominantly from Northern regions, have a correct perception of some aspects (frequency, risk factors) of cancer biology, whereas the knowledge of other aspects (outcome, prevention) remains poor or approximate. It follows that one of the main objectives of the Political Class should be to obtain a better education of overage individuals about cancer and the many problems related to this common disease.








Similar content being viewed by others
References
Crocetti E, AIRT working group. Epidemiologia & prevenzione (2006) Rivista dell’associazione Italiana di Epidemiologia.
Piñeros M, Hernàndez G, Bray F (2004) Increasing mortality rates of common malignancies in Colombia. Cancer 101:2285–2292
Doll R, Boreham J (2005) Recent trends in cancer mortality in the UK. Br J Cancer 92:1329–1335
Thoburn KK, German RR, Lewis M, Nichols PJ, Ahmed F, Jackson-Thompson J (2006) Descriptive epidemiology of colorectal cancer in the United States, 1998–2001. Cancer 107:11003–11111
Abou-Zeid AA, Khafagy W, Marzouk DM, Alaa A, Mostafa I, Ela MA (2002) Colorectal cancer in Egypt. Dis Colon Rectum 45:1255–1260
Weitz J, Koch M, Debus J, Höhler T, Galle PR, Büchler MW (2005) Colorectal cancer. Lancet 365:153–165
Arnold CN, Goel A, Blum HE, Boland CR (2005) Molecular pathogenesis of colorectal cancer: implications for molecular diagnosis. Cancer 104:2035–2047
Winawer S, Fletcher R, Rex D et al (2003) Colorectal cancer screening and surveillance: clinical guidelines and rationale—update based on new evidence. Gastroenterology 124:544–560
Boolchand V, Olds G, Singh J, Singh P, Chak A, Cooper GS (2006) Colorectal screening after polypectomy: a national survey study of primary care physicians. Ann Intern Med 145:654–659
Sawaya GF, Brown AD, Washington AE, Gaber AM (2001) Current approaches to cervical-cancer screening. N Engl J Med 344:1603–1607
Törnberg S, Kemetli L, Lynge E et al (2006) Breast cancer incidence and mortality in Nordic capitals, 1970–1998. Trends related to mammography screening programmers. Acta Oncol 45:528–535
Thompsons IM, Pauler DK, Goodman PJ et al (2004) Prevalence of prostate cancer among men with a prostate-specific antigen level ≤4.0 ng per milliliter. N Engl J Med 2350:2239–2246
Anderson WF, Guyton KZ, Hiatt RA, Vernon SW, Levin B, Hawk E (2002) Colorectal cancer screening for a person at average risk. J Natl Cancer Inst 94:1126–1133
Hosmer DW, Lemeshow S (1989) Applied logistic regression. Wiley & Sons, New York
Kolata G (1985) Debate over colon cancer screening. Science 229:636–637
Eddy DM (2004) Breast cancer screening in women younger than 50 years of age: what’s next? Ann Intern Med 127:1035–1036
Elmore JG, Barton MB, Moceri VM, Polk S, Arena PJ, Fletcher SW (1998) Ten-years risk of false positive screening mammograms and clinical breast examinations. N Engl J Med 338:1089–1096
Smith-Bindman R, Chu PW, Miglioretti DL et al (2003) Comparison of screening mammography in the United States and the United Kingdom. JAMA 290:2129–2137
La Vecchia C (2002) Fecal occult blood screening for colorectal cancer: open issues. Ann Oncol 13:31–34
Pignone M (2004) Screening for colorectal cancer: good, but not perfect. Gastroenterology 127:989–990
Johansson JE, Andrèn O, Andersson SO et al (2004) Natural history of early, localized prostate cancer. JAMA 291:2713–2719
Cannistra SA, Niloff J (1996) Cancer of the uterine cervix. N Engl J Med 334:1030–1038
Moayyedi P, Achkar E (2006) Does fecal occult blood testing really reduce mortality? A reanalysis of systematic review data. Am J Gastroenterol 101:380–384
Hakama M, Hoff G, Kronborg O, Påhlman L (2005) Screening for colorectal cancer. Acta Oncol 44:425–439
Jørgensen OD, Kronborg O, Fenger C, Rasmussen M (2007) Influence of long-term colonoscopic surveillance on incidence of colorectal cancer and death from the disease in patients with precursors (adenomas). Acta Oncol 46:355–360
Fisher DA, Jeffreys A, Coffman CJ, Fasanella K (2006) Barriers to full colon evaluation for a positive fecal occult blood test. Cancer Epidemiol Biomarkers Prev 15:1232–1235
Fisher DA, Judd L, Sanford E et al (2005) Inappropriate colorectal cancer screening: findings and implications. Am J Gastroenterol 100:2526–2530
Moja L, Moschetti I, Liberati A, Gensini GF, Gusinu R (2007) Systematic reviews highlight the complex balance between good and harm from screening studies. Intern Emerg Med 2:57–59
Schwartz LM, Woloshin S, Fowler FJ, Welch HG (2006) Enthusiasm for cancer screening in the United States. JAMA 291:71–78
Walsh JM, Terdiman JP (2003) Colorectal cancer screening. JAMA 289:1297–1302
Seeff LC, Nadel MR, Klabunde CN et al (2004) Patterns and predictors of colorectal cancer test use in the adult US population. Cancer 100:2093–2103
Yeazel MW, Church TR, Jones RM et al (2004) Colorectal cancer screening adherence in a general population. Cancer Epidemiol Biomarkers Prev 13:654–657
Bressler B, Lo C, Amar J, Whittaker S, Chaun H, Halparin L, Enns R (2004) Prospective evaluation of screening colonoscopy: who is being screened? Gastrointest Endosc 60:921–926
Zapka JG, Lemon SC, Puleo E, Estabrook B, Luckmann R, Erban S (2004) Patient education for colon cancer screening: a randomized trial of video mailed before a physical examination. Ann Intern Med 141:683–692
Zapka JG, Lemon SC, Puleo E, Estabrook B, Luckmann R, Erban S (2006) Promoting culturally appropriate colorectal cancer screening through a health educator. Cancer 107:959–966
Lowenfels AB (2002) Fecal occult blood testing as a screening procedure for colorectal cancer. Ann Oncol 13:40–43
Subramanian S, Amonkar MM, Hunt TL (2005) Use of colonoscopy for colorectal cancer screening: evidence from the 2000 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev 14:409–416
Cohen LB, Wecsler JS, Gaetano JN et al (2006) Endoscopic sedation in the United States: results from a nationwide survey. Am J Gastroenterol 101:967–974
Acknowledgments
Thanks are due to Consiglio Nazionale della Ricerca (CNR), The Italian Association for Cancer Research (AIRC), The Italian Ministry of Education (Grants COFIN-PRIN), The Region Emilia-Romagna (Screening Project) and The Lega Italiana Lotta Tumori (LILT), for generous support during the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Domati, F., Travlos, E., Cirilli, C. et al. Attitude of the Italian general population towards prevention and screening of the most common tumors, with special emphasis on colorectal malignancies. Intern Emerg Med 4, 213–220 (2009). https://doi.org/10.1007/s11739-008-0184-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-008-0184-5