Abstract
Purpose
This study aimed to evaluate the efficacy of sleeve gastrectomy (SG) on patients with obesity and polycystic ovary syndrome (PCOS).
Materials and Methods
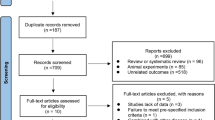
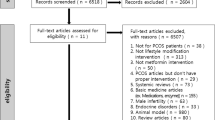
We searched PubMed, Embase, Cochrane Library, and Web of Science to identify relevant studies published prior to December 2, 2022. Meta-analysis was performed on menstrual irregularity, total testosterone, sex hormone-binding globulin (SHBG), anti-Mullerian hormone (AMH), glucolipid metabolism indicators, and body mass index (BMI) following SG.
Results
Six studies and 218 patients were included in the meta-analysis. Following SG, menstrual irregularity significantly decreased (odds ratio [OR] 0.03; 95% confidence intervals [CIs], 0.00–0.24; P=0.001). Additionally, SG can lower total testosterone levels (MD −0.73; 95% CIs −0.86–0.60; P< 0.0001), as well as BMI (MD −11.59; 95% CIs −13.10–10.08; P<0.0001). A significant increase was observed in the levels of SHBG and high-density lipoprotein (HDL) after SG. In addition to reducing fasting blood glucose, insulin, triglycerides (TG), and low-density lipoprotein levels, SG significantly reduced low-density lipoprotein levels as well.
Conclusions
Following SG, we firstly demonstrated significant improvements in menstrual irregularity, testosterone and SHGB levels, glycolipid metabolism indicators, and BMI. Therefore, SG may be considered as a new option for the clinical treatment of patients with obesity and PCOS.
Graphical Abstract







Similar content being viewed by others
References
Jebeile H, Kelly AS, O'malley G, et al. Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022;10(5):351–65.
Piché ME, Tchernof A, Després JP. Obesity phenotypes, diabetes, and cardiovascular diseases. Circ Res. 2020;126(11):1477–500.
Escobar-Morreale HF. Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat Rev Endocrinol. 2018;14(5):270–84.
Huddleston HG, Dokras A. Diagnosis and treatment of polycystic ovary syndrome. JAMA. 2022;327(3):274–5.
Durmus U, Duran C, Ecirli S. Visceral adiposity index levels in overweight and/or obese, and non-obese patients with polycystic ovary syndrome and its relationship with metabolic and inflammatory parameters. J Endocrinol Invest. 2017;40(5):487–97.
Glueck CJ, Goldenberg N. Characteristics of obesity in polycystic ovary syndrome: Etiology, treatment, and genetics. Metabolism. 2019;92:108–20.
Tian Z, Zhang YC, Wang Y, et al. Effects of bariatric surgery on patients with obesity and polycystic ovary syndrome: a meta-analysis. Surg Obes Relat Dis. 2021;17(8):1399–408.
Salminen P, Grönroos S, Helmiö M, et al. Effect of laparoscopic sleeve gastrectomy vs roux-en-y gastric bypass on weight loss, comorbidities, and reflux at 10 years in adult patients with obesity: the SLEEVEPASS randomized clinical trial. JAMA Surg. 2022;157(8):656–66.
Li YJ, Han Y, He B. Effects of bariatric surgery on obese polycystic ovary syndrome: a systematic review and meta-analysis. Surg Obes Relat Dis. 2019;15(6):942–50.
Skubleny D, Switzer NJ, Gill RS, et al. The impact of bariatric surgery on polycystic ovary syndrome: a systematic review and meta-analysis. Obes Surg. 2016;26(1):169–76.
Chang SH, Stoll CR, Song J, et al. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003-2012. JAMA Surg. 2014;149(3):275–87.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Yeung KTD, Penney N, Ashrafian L, et al. Does sleeve gastrectomy expose the distal esophagus to severe reflux?: A systematic review and meta-analysis. Ann Surg. 2020;271(2):257–65.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Wang K, Jiang Q, Zhi Y, et al. Contrasting sleeve gastrectomy with lifestyle modification therapy in the treatment of polycystic ovary syndrome. J Laparoendosc Adv Surg Tech A. 2015;25(6):493–8.
Bhandari S, Ganguly I, Bhandari M, et al. Effect of sleeve gastrectomy bariatric surgery-induced weight loss on serum AMH levels in reproductive aged women. Gynecol Endocrinol. 2016;32(10):799–802.
Abiad F, Khalife D, Safadi B, et al. The effect of bariatric surgery on inflammatory markers in women with polycystic ovarian syndrome. Diabetes Metab Syndr. 2018;12(6):999–1005.
Dai J, Li YY, Zhang XE, et al. Early improvement in obese patients with polycystic ovary syndrome after metabolic surgery may be independent of the benefits of weight loss. Int J Clin Exp Med. 2021;14(4):1768–75.
Cai M, Gao J, Du L, et al. The changes in body composition in obese patients with polycystic ovary syndrome after laparoscopic sleeve gastrectomy: a 12-month follow-up. Obes Surg. 2021;31(9):4055–63.
Hu L, Ma L, Xia X, et al. Efficacy of bariatric surgery in the treatment of women with obesity and polycystic ovary syndrome. J Clin Endocrinol Metab. 2022;107(8):e3217–29.
Hess DS, Hess DW. Biliopancreatic diversion with a duodenal switch. Obes Surg. 1998;8(3):267–82.
Clinical Issues Committee of American Society for Metabolic and Bariatric Surgery. Sleeve gastrectomy as a bariatric procedure. Surg Obes Relat Dis. 2007;3(6):573–76.
Pasquali R, Zanotti L, Fanelli F, et al. Defining hyperandrogenism in women with polycystic ovary syndrome: a challenging perspective. J Clin Endocrinol Metab. 2016;101(5):2013–22.
Moolhuijsen LME, Visser JA. Anti-Müllerian hormone and ovarian reserve: update on assessing ovarian function. J Clin Endocrinol Metab. 2020;105(11):3361–73.
Escobar-Morreale HF, San Millán JL. Abdominal adiposity and the polycystic ovary syndrome. Trends Endocrinol Metab. 2007;18(7):266–72.
Joham AE, Norman RJ, Stener-Victorin E, et al. Polycystic ovary syndrome. Lancet Diabetes Endocrinol. 2022;10(9):668–80.
Moran LJ, Misso ML, Wild RA, et al. Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2010;16(4):347–63.
De Groot PC, Dekkers OM, Romijn JA, et al. PCOS, coronary heart disease, stroke and the influence of obesity: a systematic review and meta-analysis. Hum Reprod Update. 2011;17(4):495–500.
Durlinger AL, Visser JA, Themmen AP. Regulation of ovarian function: the role of anti-Müllerian hormone. Reproduction. 2002;124(5):601–9.
Di Clemente N, Racine C, Pierre A, et al. Anti-Müllerian hormone in female reproduction. Endocr Rev. 2021;42(6):753–82.
Anderson JW, Konz EC, Frederich RC, et al. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. 2001;74(5):579–84.
Climaco K, Ahnfeldt E. Laparoscopic vertical sleeve gastrectomy. Surg Clin North Am. 2021;101(2):177–88.
Arterburn DE, Telem DA, Kushner RF, et al. Benefits and risks of bariatric surgery in adults: a review. JAMA. 2020;324(9):879–87.
Funding
This work was supported by the Wisdom Accumulation and Talent Cultivation Project of the Third Xiangya Hospital of Central South University (YX202102).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Informed Consent
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
1. We firstly performed a meta-analysis to evaluate the efficacy of sleeve gastrectomy on patients with obesity and PCOS;
2. Sleeve gastrectomy significantly improved the prevalence of menstrual irregularity, total testosterone level, glycolipid metabolism indicators, and body mass index in obese PCOS patients;
3. Sleeve gastrectomy may be considered as a new option for clinical practice in obese PCOS patients.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luo, P., Su, Z., Li, P. et al. Effects of Sleeve Gastrectomy on Patients with Obesity and Polycystic Ovary Syndrome: a Meta-analysis. OBES SURG 33, 2335–2341 (2023). https://doi.org/10.1007/s11695-023-06617-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06617-z