Abstract
Purpose
One concerning disadvantage of sleeve gastrectomy (SG) technique as a treatment for obesity is the risk of developing gastroesophageal reflux disease (GERD) or worsening its symptoms after surgery. The purpose of this study is to describe the changes in manometry and 24-h pHmetry with impedance in bariatric patients after SG.
Materials and Methods
Retrospective analysis of 225 patients who underwent SG and were subjected to manometry, 24-h phmetry, and 24-h impedance between 2006 and 2016. Patients were subdivided into groups based on the test performed: 66 patients with manometry, 60 with 24-h pHmetry and 53 with 24-h impedance. Descriptive and analytical statistics were used for analysis.
Results
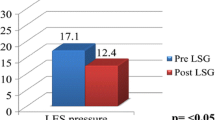
Manometry results showed a decrease in LES pressure from 12.26 ± 6.87 to 8.88 ± 6.28 mmHg in patients after surgery, de novo LES incompetence in 53.33%, worsening of symptoms in 71.4%, increase of inverted gastroesophageal gradient from 6.06% to 48.48% (p<0.05), and a rise in esophageal dysmotility from 18.19% to 37.87%. 24-h pHmetry showed an increase of DeMeester score from 16.71 ± 12.78 to 42.88 ± 32.08 after SG and 79.48% of de novo GERD. Ambulatory 24-h impedance showed an increase of pathological reflux from 47.17% to 88.67% postoperatively.
Conclusions
Laparoscopic SG is associated with a higher proportion of abnormal DeMeester score and greater incompetence of the LES in post-SG esophageal tests. Hence, SG may predispose the development of gastroesophageal reflux in the postoperative period.
Graphical abstract

Similar content being viewed by others
References
Chung Y et al. The epidemiology of obesity. Ymeta [Internet] 2018 Sept [cited 2020 Jun 13];92:p6-10. Available from: https://www.metabolismjournal.com/article/S0026-0495(18)30194-X/fulltext.
English W, Williams B. Metabolic and bariatric surgery: an effective treatment option for obesity and cardiovascular disease. Progress in Cardiovascular Diseases [Internet]. 2018 Aug [cited 2020 Jun 22];61(2):p253-269. Available from: https://www.sciencedirect.com/science/article/abs/pii/S003306201830121X?via%3Dihub.
Peterli R et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA [Internet]. 2018 [cited 2020 Jun 22];319(3):255-265. Available from: https://jamanetwork.com/journals/jama/fullarticle/2669728?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jama.2017.20897.
Chiu S et al. Effect of sleeve gastrectomy on gastroesophageal reflux disease: a systematic review. Surg Obes Relat Dis [Internet]. 2011 [cited Jun 21];7(4):510-515. Available from https://pubmed.ncbi.nlm.nih.gov/21130052/.
Moritz D et al. Reflux, sleeve dilation, and Barrett’s esophagus after laparoscopic sleeve gastrectomy: long-term follow-up. OBES SURG [Internet].2017 Jun [cited 2020 Jun 20];27(12):3092-3101. Available from https://pubmed.ncbi.nlm.nih.gov/28593484/
Navarini et al. Predictive factors of gastroesophageal reflux disease in bariatric surgery: a controlled trial comparing sleeve gastrectomy with gastric bypass. OBES SURG [Internet]. 2020 Feb [cited 2020 Jul 17];30(4):1360-1367. Available from https://pubmed.ncbi.nlm.nih.gov/32030616/.
Koppman J et al. Esophageal motility disorders in the morbidly obese population. Surg Endosc [Internet]. 2007 Feb [cited Jun 21];21:761-764. Available from https://pubmed.ncbi.nlm.nih.gov/17285388/.
Brobely Y et al. De novo gastroesophageal reflux disease after sleeve gastrectomy: role of preoperative silent reflux. Surg Endosc [Internet]. 2019 Mar [cited 2020 Jul 19];33(3):789-793. Available from https://pubmed.ncbi.nlm.nih.gov/30003346/.
Praveen P et al. Gastroesophageal reflux-related physiologic changes after sleeve gastrectomy and Roux-en-Y gastric bypass: a prospective comparative study. Surg Obes Relat Dis [Internet]. 2019 Aug [cited 2020 Jun 17]; 15(8):1261-1269. Available from https://pubmed.ncbi.nlm.nih.gov/31279562/.
Gemici E et al. Outcomes of laparoscopic sleeve gastrectomy by means of esophageal manometry and pH-metry, before and after surgery. Wideochir Inne Tech Maloinwazyjne [Internet]. 2020 Mar [cited 2020 Jul 28];15(1):129-135. Available from https://pubmed.ncbi.nlm.nih.gov/32117496/.
Oor J et al. Laparoscopic sleeve gastrectomy and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Surg [Internet]. 2016 Jan [cited 2020 Jun 21];211(1):250-67. Available from https://pubmed.ncbi.nlm.nih.gov/26341463/.
Chern T et al. High-resolution impedance manometry and 24-hour multichannel intraluminal impedance with pH testing before and after sleeve gastrectomy: de novo reflux in a prospective series. Surg Obes Relat Dis [Internet]. 2021 [cited 2022 Feb 13];329-337. Available from https://pubmed.ncbi.nlm.nih.gov/33153961/.
Yehoshua R et al. Laparoscopic sleeve gastrectomy-volume and pressure assessment. Obes Surg [Internet]. 2008 Sep [cited 2020 Jun 18];18(9):1083-1088. Available from https://pubmed.ncbi.nlm.nih.gov/18535864/.
Rebecchi et al. Gastroesophageal reflux disease and laparoscopic sleeve gastrectomy: a physiopathologie evaluation. Ann Surg [Internet]. 2014 [cited 2022 Feb 13]; 260(5): 909-14;discussion 914-5. Available from https://pubmed.ncbi.nlm.nih.gov/25379861/.
Castagneto-Gissey L et al. Sleeve gastrectomy and gastroesophageal reflux: a comprehensive endoscopic and pH-manometric prospective study. Surg Obes Relat Dis [Internet]. 2020 Nov [cited 2022 Feb 13];16(11):1629-1637. Available from https://pubmed.ncbi.nlm.nih.gov/32847760/.
Matar R et al. Esophagitis after bariatric surgery: large cross-sectional assessment of an endoscopic database. Obes Surg [Internet]. 2020 Jan [cited 2022 Feb 13]; 30(1): 161-168. Available from https://pubmed.ncbi.nlm.nih.gov/31584148/.
El-Hadi M et al. The effect of bariatric surgery on gastroesophageal reflux disease. Can J Surg [Internet]. 2014 Apr [cited 2020 Jun 21];57(2):139-144. Available from https://pubmed.ncbi.nlm.nih.gov/24666452/.
Kheirvari M et al. The advantages and disadvantages of sleeve gastrectomy; clinical laboratory to bedside review. Heliyon [Internet]. 2020 Feb [cited 2020 Jul 26];6(2):3-10. Available from https://www.sciencedirect.com/science/article/pii/S2405844020303418.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Consent to Participate
Informed consent does not apply.
Ethics Approval
For this type of study formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• After SG there is an increase of LES incompetence from 31.82% to 63.64%.
• Mean DeMeester score increased from 16.71 ± 12.78 to 42.88 ± 32.08 after SG.
• In this cohort, 79.48% developed de novo gastroesophageal reflux in 24-h phmetry.
• There was an increase of pathological impedance from 47.17% to 88.67% after SG.
Rights and permissions
About this article
Cite this article
Poggi, L., Bernui, G.M., Romani, D.A. et al. Persistent and De Novo GERD After Sleeve Gastrectomy: Manometric and pH-Impedance Study Findings. OBES SURG 33, 87–93 (2023). https://doi.org/10.1007/s11695-022-06126-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06126-5