Abstract
Purpose
Bariatric endoscopic procedures are emerging as alternatives to bariatric surgical procedures. This study aimed to assess if a natural orifice transluminal endoscopic surgery (NOTES) bariatric procedure could be converted to a surgical duodenal-jejunal bypass (DJB) or sleeve gastrectomy (SG).
Materials and Methods
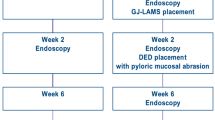
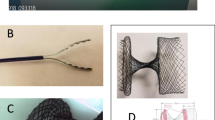
This 12-week prospective study compared 4 test pigs to 3 control (no procedures) pigs aged 3 months at baseline. The test pigs received a fully endoscopic NOTES-based bypass including measurement of the bypassed limb and creation of a gastrojejunal anastomosis (GJA) using gastrojejunal lumen-apposing metal stents (GJ-LAMS) at Week 0, placement of a duodenal exclusion device (DED) at Week 2, and randomization to DJB or SG surgery at Week 8 with subsequent 4-week follow-up. At Week 12, the pigs were sacrificed and necropsy was performed.
Results
Endoscopic procedures were technically successful. One pig did not receive a DED due to early GJ-LAMS migration leading to premature closure of the GJA. At Week 8, all 4 pigs were doing well, and the remaining 3 GJ-LAMS and 3 DEDs were uneventfully endoscopically removed. Two one-anastomosis DJB were performed, and 2 SG were performed, closing in one case the site of the previous GJA. The surgical procedures were technically feasible and uneventful during follow-up. Necropsy assessments showed no local or peritoneal inflammation or abscess and no leakage or fistula.
Conclusion
An endoscopic bariatric bypass can be transitioned to a one-anastomosis duodenal-jejunal bypass or sleeve gastrectomy, without complications.
Graphical abstract







Similar content being viewed by others
Data Availability
The data, analytic methods, and study materials for this study may be made available to other researchers in accordance with the Boston Scientific Data Sharing Policy (http://www.bostonscientific.com/en-US/data-sharing-requests.html).
References
Kalloo AN, Singh VK, Jagannath SB, et al. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114–7.
Vanbiervliet G, Bonin EA, Garces R, et al. Gastrojejunal anastomosis using a tissue-apposing stent: a safety and feasibility study in live pigs. Endoscopy. 2014;46:871–7.
Gonzalez JM, Beyer L, Garnier E, et al. Safety and clinical outcomes of endoscopic gastrojejunal anastomosis in obese Yucatan pigs with or without duodenal exclusion using new 20mm lumen-apposing metal stent: A pilot study. Clin Res Hepatol Gastroenterol. 2020;44:786–9.
Lim CH, Lee ZJ, Yeung B, et al. Natural orifice transluminal endoscopic one-anastomosis gastric bypass: a feasibility study using porcine model. Surg Endosc. 2021;35(10):5842–51. https://doi.org/10.1007/s00464-021-08547-2
Gonzalez JM, Ouazzani S, Monino L, et al. First fully endoscopic metabolic procedure with NOTES gastrojejunostomy, controlled bypass length and duodenal exclusion: a 9-month porcine study. Sci Rep. 2022;12:21.
DuCoin C, Moore RL, Provost DA. Indications and contraindications for bariatric surgery. In: Nguyen N, Brethauer S, Morton J, Ponce J, Rosenthal R, editors. The ASMBS textbook of bariatric surgery. Cham: Springer; 2020. https://doi.org/10.1007/978-3-030-27021-6_6
Major P, Stefura T, Waledziak M, et al. What makes bariatric operations difficult-results of a national survey. Medicina (Kaunas). 2019;55.
Percie du Sert N, Hurst V, Ahluwalia A, et al. The ARRIVE guidelines 2.0: updated guidelines for reporting animal research. Plos Biol. 2020;18:e3000410.
Arterburn DE, Telem DA, Kushner RF, et al. Benefits and risks of bariatric surgery in adults: a review. Jama. 2020;324:879–87.
Abu-Dayyeh BK, Sarmiento R, Rajan E, et al. Endoscopic treatments of obesity and metabolic disease: are we there yet? Rev Esp Enferm Dig. 2014;106:467–76.
Wang FG, Yan WM, Yan M, et al. Outcomes of Mini vs Roux-en-Y gastric bypass: A meta-analysis and systematic review. Int J Surg. 2018;56:7–14.
Aleman R, Lo Menzo E, Szomstein S, et al. Efficiency and risks of one-anastomosis gastric bypass. Ann Transl Med. 2020;8:S7.
Solouki A, Kermansaravi M, Davarpanah Jazi AH, et al. One-anastomosis gastric bypass as an alternative procedure of choice in morbidly obese patients. J Res Med Sci. 2018;23:84.
Kermansaravi M, Shahmiri SS, DavarpanahJazi AH, et al. One anastomosis/mini-gastric bypass (OAGB/MGB) as revisional surgery following primary restrictive bariatric procedures: a systematic review and meta-analysis. Obes Surg. 2021;31:370–83.
Pucher PH, Lord AC, Sodergren MH, et al. Reversal to normal anatomy after failed gastric bypass: systematic review of indications, techniques, and outcomes. Surg Obes Relat Dis. 2016;12:1351–6.
Ozsoy Z, Demir E. Which bariatric procedure is the most popular in the world? A bibliometric comparison Obes Surg. 2018;28:2339–52.
Livingston EH, Langert J. The impact of age and Medicare status on bariatric surgical outcomes. Arch Surg. 2006;141:1115–20 (discussion 1121).
Ponce de Leon-Ballesteros G, Sanchez-Aguilar HA, Velazquez-Fernandez D, et al. Roux-en-Y gastric bypass in patients >60 years of age: morbidity and short-term outcomes. Obes Surg. 2020;30:5033–40.
Prasad J, Vogels E, Dove JT, et al. Is age a real or perceived discriminator for bariatric surgery? A long-term analysis of bariatric surgery in the elderly. Surg Obes Relat Dis. 2019;15:725–31.
Hammond JB, Webb CJ, Pulivarthi V, et al. Is there an upper age limit for bariatric surgery? Laparoscopic gastric bypass outcomes in septuagenarians. Obes Surg. 2020;30:2482–6.
Ryou M, McQuaid KR, Thompson CC, et al. ASGE EndoVators summit: defining the role and value of endoscopic therapies in obesity management. Surg Obes Relat Dis. 2017;13:1805–16.
Acknowledgements
The authors acknowledge the contributions of Joe Gorman, BFA (professional medical illustrator), and Boston Scientific Corporation employees Edmund McMullen, MMath (statistical analysis), and Margaret Gourlay, MD, MPH (writing assistance).
Funding
Funding was provided by the Boston Scientific Corporation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All applicable institutional and/or national guidelines for the care and use of animals were followed.
Consent to Participate
Informed Consent does not apply.
Conflict of Interest
The authors disclose the following: Jean-Michel Gonzalez and Marc Barthet report funding from Boston Scientific Corporation for research. Nicolas Cauche and Cecilia Delattre are full-time employees of the Brussels Medical Device Center, which received a cooperative engineering grant from Boston Scientific Corporation. Joyce A. Peetermans, Ornela Gjata, and Agostina Santoro-Schulte are full-time employees of Boston Scientific Corporation. Pauline Duconseil, Sohaib Ouazzani, and Stephane Berdah have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
Few eligible patients undergo bariatric surgery.Endoscopic alternatives with potential for conversion to bariatric surgery are needed.
In the current study, a natural orifice transluminal endoscopic surgery (NOTES)-based endoscopic bypass procedure was successfully converted to a one-anastomosis duodenal-jejunal bypass or sleeve gastrectomy in a growing porcine model.
A NOTES bypass procedure appears as a complementary technique to bariatric surgery allowing adaptive management from incisionless to more invasive surgical procedures.
Rights and permissions
About this article
Cite this article
Gonzalez, JM., Duconseil, P., Ouazzani, S. et al. Feasibility of Conversion of a New Bariatric Fully Endoscopic Bypass Procedure to Bariatric Surgery: a Porcine Pilot Study. OBES SURG 32, 2280–2288 (2022). https://doi.org/10.1007/s11695-022-06065-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06065-1