Abstract
Purpose
With increasing BMI, the complexity of treating patients with obesity rises. The focus of this study is to investigate the effects of sleeve gastrectomy (SG) and Roux-en-Y gastric bypass (RYGB) on perioperative morbidity and remission of comorbidities at 3 years in patients with a BMI > 50 kg/m2.
Materials and Methods
A retrospective multicenter analysis of a prospectively maintained database was performed to enroll patients with a 3-year follow-up after SG or RYGB between 2005 and 2019 and a BMI of > 50 kg/m2 preoperatively. Patients’ BMI and comorbidity status were recorded preoperatively.
Results
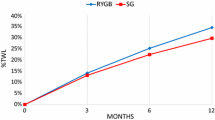
We analyzed data from 2939 patients who had at least a preoperative BMI > 50 kg/m2. A total of 1278 patients underwent RYGB surgery, and 1661 underwent SG. The distribution of sex, BMI, hypertension, reflux, and sleep apnea was significant between the two groups. Three years after surgery, the percent excess weight loss (%EWL) was 62.21% in RYGB and 55.87% in SG (p < 0.001). The change in hypertension (p < 0.001) and reflux (p < 0.001) was significantly in favor of RYGB. The change in diabetes mellitus was not significant between the two groups (p > 5%). There was a minimal difference in sleep apnea in favor of SG (p < 0.001). Mortality and overall complication rates were not significant in either group.
Conclusion
Both procedures positively affected comorbidities, BMI, and %EWL in patients with super obesity 3 years after surgery. In some categories, RYGB was better than SG. Nevertheless, the decision between the two methods remains a matter of the surgeon’s experience and the patient's general condition.
Graphical abstract

Similar content being viewed by others
References
Mensink GB, Schienkiewitz A, Haftenberger M, Lampert T, Ziese T, Scheidt-Nave C. Übergewicht und Adipositas in Deutschland: Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1) [Overweight and obesity in Germany: results of the German Health Interview and Examination Survey for Adults (DEGS1)]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56(5–6):786–94. German. https://doi.org/10.1007/s00103-012-1656-3. PMID: 23703499.
Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, Flegal KM. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016;315(21):2292–9. https://doi.org/10.1001/jama.2016.6361.PMID:27272581;PMCID:PMC6361521.
Yumuk V, Tsigos C, Fried M, Schindler K, Busetto L, Micic D, Toplak H. Obesity Management Task Force of the European Association for the study of obesity. European Guidelines for obesity management in adults. Obes Facts. 2015;8(6):402–24. https://doi.org/10.1159/000442721. Epub 2015 Dec 5. Erratum in: Obes Facts. 2016;9(1):64. PMID: 26641646; PMCID: PMC5644856.
Khaodhiar L, McCowen KC, Blackburn GL. Obesity and its comorbid conditions. Clin Cornerstone. 1999;2(3):17–31. https://doi.org/10.1016/s1098-3597(99)90002-9 (PMID: 10696282).
Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12(2):131–41. https://doi.org/10.1111/j.1467-789X.2009.00712.x (PMID: 20122135).
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. https://doi.org/10.1001/jama.2012.113905.PMID:23280227;PMCID:PMC4855514.
Major P, Matłok M, Pędziwiatr M, Migaczewski M, Budzyński P, Stanek M, Kisielewski M, Natkaniec M, Budzyński A. Quality of life after bariatric surgery. Obes Surg. 2015;25(9):1703–10. https://doi.org/10.1007/s11695-015-1601-2.PMID:25676156;PMCID:PMC4522031.
Arterburn DE, Telem DA, Kushner RF, Courcoulas AP. Benefits and risks of bariatric surgery in adults: a review. JAMA. 2020;324(9):879–87. https://doi.org/10.1001/jama.2020.12567 (PMID: 32870301).
Athyros VG, Tziomalos K, Karagiannis A, Mikhailidis DP. Cardiovascular benefits of bariatric surgery in morbidly obese patients. Obes Rev. 2011;12(7):515–24. https://doi.org/10.1111/j.1467-789X.2010.00831.x (Epub 2011 Feb 23 PMID: 21348922).
Arapis K, Macrina N, Kadouch D, Ribeiro Parenti L, Marmuse JP, Hansel B. Outcomes of Roux-en-Y gastric bypass versus sleeve gastrectomy in super-super-obese patients (BMI ≥60 kg/m2): 6-year follow-up at a single university. Surg Obes Relat Dis. 2019;15(1):23–33. https://doi.org/10.1016/j.soard.2018.09.487 (Epub 2018 Oct 11 PMID: 30454974).
Chaar ME, Lundberg P, Stoltzfus J. Thirty-day outcomes of sleeve gastrectomy versus Roux-en-Y gastric bypass: first report based on Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database. Surg Obes Relat Dis. 2018;14(5):545–51. https://doi.org/10.1016/j.soard.2018.01.011 (Epub 2018 Jan 13 PMID: 29551470).
Bhandari M, Ponce de Leon-Ballesteros G, Kosta S, Bhandari M, Humes T, Mathur W, Fobi M. Surgery in patients with super obesity: medium-term follow-up outcomes at a high-volume center. Obesity (Silver Spring). 2019;27(10):1591–1597. https://doi.org/10.1002/oby.22593. Epub 2019 Sep 3. PMID: 31479206.
Celio AC, Wu Q, Kasten KR, Manwaring ML, Pories WJ, Spaniolas K. Comparative effectiveness of Roux-en-Y gastric bypass and sleeve gastrectomy in super obese patients. Surg Endosc. 2017;31(1):317–23. https://doi.org/10.1007/s00464-016-4974-y (Epub 2016 Jun 10 PMID: 27287899).
Stephens DJ, Saunders JK, Belsley S, Trivedi A, Ewing DR, Iannace V, Capella RF, Wasielewski A, Moran S, Schmidt HJ, Ballantyne GH. Short-term outcomes for super-super obese (BMI > or =60 kg/m2) patients undergoing weight loss surgery at a high-volume bariatric surgery center: laparoscopic adjustable gastric banding, laparoscopic gastric bypass, and open tubular gastric bypass. Surg Obes Relat Dis. 2008;4(3):408–15. https://doi.org/10.1016/j.soard.2007.10.013. Epub 2008 Feb 1. PMID: 18243060.
Wilkinson KH, Helm M, Lak K, Higgins RM, Gould JC, Kindel TL. The risk of post-operative complications in super-super obesity compared to super obesity in accredited bariatric surgery centers. Obes Surg. 2019;29(9):2964–71. https://doi.org/10.1007/s11695-019-03942-0 (PMID: 31134478).
Mehaffey JH, LaPar DJ, Turrentine FE, Miller MS, Hallowell PT, Schirmer BD. Outcomes of laparoscopic Roux-en-Y gastric bypass in super-super-obese patients. Surg Obes Relat Dis. 2015;11(4):814–9. https://doi.org/10.1016/j.soard.2014.11.027. Epub 2014 Dec 8. PMID: 25980328.
Nasser H, Ivanics T, Leonard-Murali S, Shakaroun D, Genaw J. Perioperative outcomes of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy in super-obese and super-super-obese patients: a national database analysis. Surg Obes Relat Dis. 2019;15(10):1696–703. https://doi.org/10.1016/j.soard.2019.07.026 (Epub 2019 Aug 10 PMID: 31530452).
Elbahrawy A, Bougie A, Loiselle SE, Demyttenaere S, Court O, Andalib A. Medium to long-term outcomes of bariatric surgery in older adults with super obesity. Surg Obes Relat Dis. 2018;14(4):470–6. https://doi.org/10.1016/j.soard.2017.11.008 (Epub 2017 Nov 10 PMID: 29249586).
Øvrebø B, Strømmen M, Kulseng B, Martins C. Bariatric surgery versus lifestyle interventions for severe obesity: 5-year changes in body weight, risk factors and comorbidities. Clin Obes. 2017;7(3):183–90. https://doi.org/10.1111/cob.12190 (Epub 2017 Mar 20 PMID: 28320081).
Uno K, Seki Y, Kasama K, Wakamatsu K, Umezawa A, Yanaga K, Kurokawa Y. A Comparison of the bariatric procedures that are performed in the treatment of super morbid obesity. Obes Surg. 2017;27(10):2537–45. https://doi.org/10.1007/s11695-017-2685-7.Erratum.In:ObesSurg.2018Dec3; (PMID: 28451928).
Bettencourt-Silva R, Neves JS, Pedro J, Guerreiro V, Ferreira MJ, Salazar D, Souteiro P, Magalhães D, Oliveira SC, Queirós J, Belo S, Varela A, Freitas P; AMTCO Group, Carvalho D. Comparative effectiveness of different bariatric procedures in super morbid obesity. Obes Surg. 2019;29(1):281–291. https://doi.org/10.1007/s11695-018-3519-y. PMID: 30251091.
Wang Y, Song YH, Chen J, Zhao R, Xia L, Cui YP, Rao ZY, Zhou Y, Wu XT. Roux-en-Y gastric bypass versus sleeve gastrectomy for super super obese and super obese: systematic review and meta-analysis of weight results, comorbidity resolution. Obes Surg. 2019;29(6):1954–64. https://doi.org/10.1007/s11695-019-03817-4 (PMID: 30953336).
Lopes EC, Heineck I, Athaydes G, Meinhardt NG, Souto KE, Stein AT. Is bariatric surgery effective in reducing comorbidities and drug costs? A systematic review and meta-analysis. Obes Surg. 2015;25(9):1741–9. https://doi.org/10.1007/s11695-015-1777-5 (PMID: 26112137).
Baptista V, Wassef W. Bariatric procedures: an update on techniques, outcomes and complications. Curr Opin Gastroenterol. 2013;29(6):684–93. https://doi.org/10.1097/MOG.0b013e3283651af2 (PMID: 24100715).
Vinciguerra F, Baratta R, Farina MG, Tita P, Padova G, Vigneri R, Frittitta L. Very severely obese patients have a high prevalence of type 2 diabetes mellitus and cardiovascular disease. Acta Diabetol. 2013;50(3):443–9. https://doi.org/10.1007/s00592-013-0460-3 (Epub 2013 Feb 28 PMID: 23447004).
Rajan R, Sam-Aan M, Kosai NR, Shuhaili MA, Chee TS, Venkateswaran A, Mahawar K. Early outcome of bariatric surgery for the treatment of type 2 diabetes mellitus in super-obese Malaysian population. J Minim Access Surg. 2020;16(1):47–53. https://doi.org/10.4103/jmas.JMAS_219_18. PMID: 30618425; PMCID: PMC6945344.
Thereaux J, Corigliano N, Poitou C, Oppert JM, Czernichow S, Bouillot JL. Comparison of results after one year between sleeve gastrectomy and gastric bypass in patients with BMI ≥ 50 kg/m2. Surg Obes Relat Dis. 2015;11(4):785–90. https://doi.org/10.1016/j.soard.2014.11.022. Epub 2014 Dec 4. PMID: 25771441.
Yaghoubian A, Tolan A, Stabile BE, Kaji AH, Belzberg G, Mun E, Zane R. Laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy achieve comparable weight loss at 1 year. Am Surg. 2012;78(12):1325–8 (PMID: 23265120).
Onyewu SC, Ogundimu OO, Ortega G, Bauer ES, Emenari CC, Molyneaux ND, Layne SA, Changoor NR, Tapscott D, Tran DD, Fullum TM. Bariatric surgery outcomes in black patients with super morbid obesity: a 1-year postoperative review. Am J Surg. 2017;213(1):64–8. https://doi.org/10.1016/j.amjsurg.2016.05.010 (Epub 2016 Jun 16 PMID: 27816202).
Hidalgo M, Vilallonga R, Ruiz de Godejuela AG, Rodríguez-Luna MR, Balibrea JM, Roriz-Silva R, González O, Caubet E, Ciudin A, Armengol M, Fort JM. Effectiveness of laparoscopic sleeve gastrectomy in super-obese and non-super-obese patients. Surg Laparosc Endosc Percutan Tech. 2020;30(5):403–409. https://doi.org/10.1097/SLE.0000000000000801. PMID: 32427745.
Kowalewski PK, Olszewski R, Walędziak MS, Janik MR, Kwiatkowski A, Gałązka-Świderek N, Cichoń K, Brągoszewski J, Paśnik K. Long-term outcomes of laparoscopic sleeve gastrectomy-a single-center, retrospective study. Obes Surg. 2018;28(1):130–4. https://doi.org/10.1007/s11695-017-2795-2.PMID:28707172;PMCID:PMC5735208.
Del Genio G, Limongelli P, Del Genio F, Motta G, Docimo L, Testa D. Sleeve gastrectomy improves obstructive sleep apnea syndrome (OSAS): 5 year longitudinal study. Surg Obes Relat Dis. 2016;12(1):70–4. https://doi.org/10.1016/j.soard.2015.02.020 (Epub 2015 Mar 3 PMID: 25862184).
Amin R, Simakajornboon N, Szczesniak R, Inge T. Early improvement in obstructive sleep apnea and increase in orexin levels after bariatric surgery in adolescents and young adults. Surg Obes Relat Dis. 2017;13(1):95–100. https://doi.org/10.1016/j.soard.2016.05.023. Epub 2016 May 30. PMID: 27720196; PMCID: PMC5130623.
Samuel N, Jalal Q, Gupta A, Mazari F, Vasas P, Balachandra S. Mid-term bariatric surgery outcomes for obese patients: does weight matter? Ann R Coll Surg Engl. 2020;102(1):54–61. https://doi.org/10.1308/rcsann.2019.0100. Epub 2019 Sep 6. PMID: 31891669; PMCID: PMC6937615.
Acknowledgements
We would like to thank Mr. Hukauf for his contributions to the statistical analysis of our data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
For this type of study formal consent is not required. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• No significant difference was found between SG and RYGB in terms of perioperative and postoperative complications.
• SG and RYGB can be considered adequate bariatric procedures in patients with super obesity
• The impact on comorbidities was different between SG and RYGB.
Rights and permissions
About this article
Cite this article
Thaher, O., Tallak, W., Hukauf, M. et al. Outcome of Sleeve Gastrectomy Versus Roux-en-Y Gastric Bypass for Patients with Super Obesity (Body Mass Index > 50 kg/m2). OBES SURG 32, 1546–1555 (2022). https://doi.org/10.1007/s11695-022-05965-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-05965-6



