Abstract
Purpose
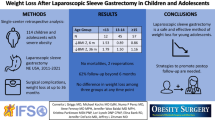
Obesity is a complex multifactorial disease. Parents with obesity could have an impact on the weight loss outcome of their children following bariatric-metabolic surgery. Therefore, we aimed to investigate the association between the weight status of the parents and the weight loss outcome in patients undergoing sleeve gastrectomy (SG).
Methods
Patients undergoing SG with ≥ 3 years of follow-up between January 2016 and June 2018 were included in this study. The patients were categorized into three groups: (1) both parents did not have obesity (non-obesity parents, NOP); (2) one parent had obesity (single-parent obesity, SPO); (3) both parents had obesity (both parents’ obesity, BPO). The main parameters for this study were the patients’ preoperative and postoperative weight and the weight of the parents.
Results
A total of 218 SG patients were included in this study (NOP, n = 116; SPO, n = 64; BPO, n = 38). There was no statistically significant difference in the preoperative assessments. The main results for the NOP vs. SPO vs. BPO were as follows; parents’ body mass index (BMI) 23.6 ± 2.5 vs. 27.9 ± 5.0 vs. 30.2 ± 3.3 kg/m2, percentage of total weight loss (%TWL) 30.2 ± 9.0 vs. 30.8 ± 10.4 vs. 23.8 ± 10.9%. The %TWL for the BPO group was significantly lower than the NOP and SPO groups (p < 0.05).
Conclusion
The patient’s weight loss outcome was significantly lower when both parents had obesity. Further controlled or prospective studies are needed to determine the best means to improve weight loss outcomes in such patients.
Graphical abstract

Similar content being viewed by others
References
González-Muniesa P, Mártinez-González MA, Hu FB, et al. Obesity. Nat Rev Dis Primers. 2017;15(3):17034.
Misra S, Bhattacharya S, Saravana Kumar S, Nandhini BD, Saminathan SC, Praveen RP. Long-term outcomes of laparoscopic sleeve gastrectomy from the Indian subcontinent. Obes Surg. 2019;29(12):4043–55.
Peterli R, Wölnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA. 2018;319(3):255–65.
Salminen P, Helmiö M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: the SLEEVEPASS randomized clinical trial. JAMA. 2018;319(3):241–54.
Fiorani C, Coles SR, Kulendran M, McGlone ER, Reddy M, Khan OA. Long-term quality of life outcomes after laparoscopic sleeve gastrectomy and Roux-en-y gastric bypass-a comparative study. Obes Surg. 2021;31(3):1376–80.
Dent R, McPherson R, Harper ME. Factors affecting weight loss variability in obesity. Metabolism. 2020;113:154388.
Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–9.
Shrewsbury VA, Steinbeck KS, Torvaldsen S, Baur LA. The role of parents in pre-adolescent and adolescent overweight and obesity treatment: a systematic review of clinical recommendations. Obes Rev. 2011;12(10):759–69.
Chen CM. Overview of obesity in Mainland China. Obes Rev. 2008;9(Suppl 1):14–21.
Chu Y, Widjaja J, Hong J, Dolo PR, Zhu X, Yao L. Effect of Sleeve Gastrectomy on Plasma Thioredoxin-Interacting Protein (TXNIP). Obes Surg. 2021;31(11):4829–35.
Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6(1):67–85.
Frayling TM, Timpson NJ, Weedon MN, et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science. 2007;316(5826):889–94.
Yang J, Loos RJ, Powell JE, et al. FTO genotype is associated with phenotypic variability of body mass index. Nature. 2012;490(7419):267–72.
Claussnitzer M, Dankel SN, Kim KH, et al. FTO obesity variant circuitry and adipocyte browning in humans. N Engl J Med. 2015;373(10):895–907.
Slotman GJ. Gastric bypass: a family affair–41 families in which multiple members underwent bariatric surgery. Surg Obes Relat Dis. 2011;7(5):592–8.
Magouliotis DE, Tasiopoulou VS, Svokos AA, Svokos KA, Sioka E, Zacharoulis D. One-anastomosis gastric bypass versus sleeve gastrectomy for morbid obesity: a systematic review and meta-analysis. Obes Surg. 2017;27(9):2479–87.
O’Brien PE, Hindle A, Brennan L, et al. Long-term outcomes after bariatric surgery: a systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-centre review of 20-year outcomes after adjustable gastric banding. Obes Surg. 2019;29(1):3–14.
Spinos D, Skarentzos K, Esagian SM, Seymour KA, Economopoulos KP. The effectiveness of single-anastomosis duodenoileal bypass with sleeve gastrectomy/one anastomosis duodenal switch (SADI-S/OADS): an updated systematic review. Obes Surg. 2021;31(4):1790–800.
Kindel T, Lomelin D, McBride C, Kothari V, Thompson J. The time to weight-loss steady state after gastric bypass predicts weight-loss success. Obes Surg. 2016;26(2):327–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this retrospective study, additional formal consent is not required.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• The weight loss outcomes of patients undergoing bariatric-metabolic surgery are associated with their parents’ weight status.
• Having at least one parent with a healthy weight status could lead to better weight loss outcomes for bariatric patients.
• Future studies need to focus on the genetics of obesity, such as whether parents with obesity have different genetic expressions than parents with healthy weight status, furthermore, whether these genes are inherited by their children.
Rights and permissions
About this article
Cite this article
Widjaja, J., Wu, W., Yao, L. et al. Association Between the Parental Weight Status and the Weight Loss Outcome in Patients After Sleeve Gastrectomy. OBES SURG 32, 868–872 (2022). https://doi.org/10.1007/s11695-021-05878-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05878-w