Abstract
Background
Bariatric surgery has been increasingly becoming popular due to the advancements in minimally invasive approaches and techniques. The aim of this study was to compare the long-term outcomes and clinical relevance of laparoscopic sleeve gastrectomy (LSG) and laparoscopic greater curvature plication (LGCP) in a matched controlled single-bariatric centre study.
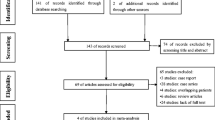
Methods
We collected data from 163 patients who underwent either LSG or LGCP over a period of at least 5 years. The outcome parameters included body mass index (BMI) changes, causes of revision surgery, endoscopic findings and effects on obesity-related comorbidities.
Results
A total of 79 patients underwent LGCP, while 84 underwent LSG for morbid obesity. At the fifth year of follow-up, a BMI of < 30 was achieved in 1% of patients who underwent LGCP (n = 1) compared with more than 80% of patients who underwent LSG (n = 70). Revision was mainly due to gastroesophageal reflux disease (GERD) or bile reflux in the LSG group and due to weight gain in the LGCP group. LSG was superior in improvements in comorbidities. The most observed endoscopic finding was GERD (grade a, b) in the LSG group and unfolding of part of or the whole stomach in the LGCP group. Early minor postoperative complications occurred at a significantly lower frequency in the LSG group.
Conclusions
LGCP has a higher rate of complications, a much less durable effect on weight loss, a higher rate of revision surgery and a higher cost burden to the health care system than LSG.
Graphical abstract




Similar content being viewed by others
References
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
DeMaria EJ. Bariatric surgery for morbid obesity. N Engl J Med. 2007;356:2176–83.
Tsigos C, Hainer V, Basdevant A, Finer N, Fried M, Mathus-Vliegen E, Micic D, Maislos M, Roman G, Schutz Y, Toplak H, Zahorska-Markiewicz B, Obesity Management Task Force of the European Association for the Study of Obesity. Management of obesity in adults: European clinical practice guidelines. Obes Facts. 2008;1:106–16.
Brody F. Minimally invasive surgery for morbid obesity. Clev Clinic J Med. 2004;71:289–98.
Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ. Colditz GA The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003–2012. JAMA Surg. 2014;149:275–87.
Ye Q, Chen Y, Zhan X, et al. Comparison of laparoscopic sleeve gastrectomy and laparoscopic greater curvature plication regarding efficacy and safety: a meta-analysis. Obes Surg. 2017;27(5):1358–64.
Talebpour M, Sadid D, Talepour A, Sharifi A, Davari FV. Comparison of short-term effectiveness and postoperative complications: laparoscopic gastric plication vs laparoscopic sleeve gastrectomy. Obes. 2018;28(4):996–1001.
Talebpour M. Amoli BS Laparoscopic total gastric vertical plication in morbid obesity. J Laparoend Adv Surg Tech. 2007;17:793–8.
Niazi M, Maleki AR. Talebpour M Short-term outcomes of laparoscopic gastric plication in morbidly obese patients: importance of postoperative follow-up. Obes Surg. 2013;23:87–92.
Guo S, Fraser MW. Propensity score analysis: statistical methods and applications. 2nd ed. Thousand Oaks: Sage Publications Inc; 2015.
Hubbard AE, Ahern J, Fleischer NL, Van der Laan M, Lippman SA, Jewell N, Bruckner T, Satariano WA. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighbourhood risk factors and health. Epidemiology. 2010;21:467–74.
Masters GN. A Rasch model for partial credit scoring. Psychometrika. 1982;47:149–74.
IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk: IBM Corp.
Stevenson M, Sergeant E with contributions from Telmo Nunes, Cord Heuer, Jonathon Marshall, Javier Sanchez, Ron Thornton, Jeno Reiczigel, Jim Robison-Cox, Paola Sebastiani, Peter Solymos, Kazuki Yoshida, Geoff Jones, Sarah Pirikahu, Simon Firestone, Ryan Kyle, Johann Popp, Mathew Jay and Charles Reynard. (2021). epiR: tools for the analysis of epidemiological data. R package version 2.0.19. https://CRAN.R-project.org/package=epiR.
H. Wickham. ggplot2: elegant graphics for data analysis. Springer-Verlag New York, 2016. https://ggplot2.tidyverse.org.
R Core Team (2021). R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.
Brethauer SA, Kim J, el Chaar M, Papasavas P, Eisenberg D, Rogers A, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11:489–506.
Barrichello S, Minata MK, Garcia Ruiz de Gordejuela A, et al. Laparoscopic greater curvature plication and laparoscopic sleeve gastrectomy treatments for obesity: systematic review and metaanalysis of short- and mid-term results. Obes Surg. 2018;28(10):3199–212.
Perivoliotis K, Sioka E, Katsogridaki G, et al. Laparoscopic gastric plication versus laparoscopic sleeve gastrectomy: an up-to-date systematic review and meta-analysis. J Obes. 2018;2018:3617458.
Skrekas G, Antiochos K. Stafyla VK Laparoscopic gastric greater curvature plication: results and complications in a series of 135 patients. Obes Surg. 2011;21:1657–63.
Coskun H, Cipe G, Bozkurt S, Bektasoglu HK, Hasbahceci M. Muslumanoglu M Laparoscopic sleeve gastrectomy in management of weight regain after failed laparoscopic plication. Int J Surg Case Rep. 2013;4:872–4.
Dolezalova-Kormanova K, Buchwald JN, Skochova D, et al. Five-year outcomes: laparoscopic greater curvature plication for treatment of morbid obesity. Obes Surg. 2017;27(11):2818–28.
Atlas H, Yazbek T, Garneau PY, et al. Is there a future for laparoscopic gastric greater curvature plication (LGGCP)? A review of 44 patients. Obes Surg. 2013;23(9):1397–403.
Talebpour M, Motamedi SM, Talebpour A, et al. Twelve year experience of laparoscopic gastric plication in morbid obesity: development of the technique and patient outcomes. Ann Surg Innov Res. 2012;6(1):7.
Catheline JM, Fysekidis M. Bachner I et al Five-year results of sleeve gastrectomy. J Visc Surg. 2013;150:307–12.
Sheppard CE, Sadowski DC. de Gara CJ et al Rates of reflux before and after laparoscopic sleeve gastrectomy for severe obesity. Obes Surg. 2015;25:763–8.
Oor JE, Roks DJ. Ünlü Ç et al Laparoscopic sleeve gastrectomy and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Surg. 2016;211(1):250–67.
Yeung KTD, Penney N, Ashrafan L, et al. Does sleeve gastrectomy expose the distal oesophagus to severe reflux? A systematic review and meta-analysis. Ann Surg. 2019;271:257.
Pilone V, Tramontano S, Renzulli M, et al. Gastroesophageal refux after sleeve gastrectomy: new onset and effect on symptoms on a prospective evaluation. Obes Surg. 2019. https://doi.org/10.1007/s11695-019-04046-5.
Rebecchi F, Allaix ME, Giaccone C, Ugliono E, Scozzari G, Morino M. Gastroesophageal refux disease and laparoscopic sleeve gastrectomy: a physiopathologic evaluation. Ann Surg. 2014;260:909–14.
Bashar J, Qumsiyeh Y, Ponniah SA, Friedman J, Ayzengart A, Draganov PV, et al. Barrett’s esophagus after sleeve gastrectomy: a systematic review and meta-analysis. Gastrointest Endosc. 2021;93(2):343–52.
De Angelis F, Avallone M, Albanese A, et al. Re-sleeve gastrectomy 4 years later: is it still an effective revisional option? Obes Surg. 2018;28(11):3714–6.
Boru CE, Greco F, Giustacchini P, et al. Short-term outcomes of sleeve gastrectomy conversion to R-Y gastric bypass: multi-center retrospective study. Langenbeck Arch Surg. 2018;403(4):473–9.
Guan B, Chong TH, Peng J, Chen Y, Wang C, Yang J. Mid-long-term revisional surgery after sleeve gastrectomy: a systematic review and meta-analysis. Obes Surg. 2019;29:1965–75.
Neagoe RM, Timofte D, Muresan M, et al. Laparoscopic gastric plication vs laparoscopic sleeve gastrectomy - a single center, prospective and case-control study. Chirurgia (Bucur). 2019;114(6):769–78.
Zerrweck C, Rodriguez JG, Aramburo E, et al. Revisional surgery following laparoscopic gastric plication. Obes Surg. 2017;27(1):38–43.
Suarez DF, Gangemi A. How Bad Is “Bad”? A cost consideration and review of laparoscopic gastric plication versus laparoscopic sleeve gastrectomy. Obes Surg. 2021;31(1):307–16.
Shen D, Ye H, Wang Y, et al. Comparison of short-term outcomes between laparoscopic greater curvature plication and laparoscopic sleeve gastrectomy. Surg Endosc. 2013;27(8):2768–74.
Abdelbaki TN, Sharaan M, Abdel-Baki NA, Katri K. Laparoscopic gastric greater curvature plication versus laparoscopic sleeve gastrectomy: early outcome in 140 patients. Surg Obes Relat Dis. 2014;10(6):1141–6.
Juodeikis Ž, Brimas G. Long-term results after sleeve gastrectomy: a systematic review. Surg Obes Relat Dis. 2017;13(4):693–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• LSG resulted in significant changes in terms of long-term BMI loss and fewer minor postoperative complications than LGCP.
• LGCP resulted in a significantly higher incidence of weight regain and the need for revisional surgery than LSG.
• The most commonly observed endoscopic finding was gastroesophageal reflux disease (GERD), grades a and b in the LSG group and the unfolding of part of or the whole stomach in the LGCP group.
Rights and permissions
About this article
Cite this article
Ibrahim, M., Hany, M., Zidan, A. et al. Laparoscopic Sleeve Gastrectomy Versus Laparoscopic Greater Curvature Plication: a Long-Term Follow-up Study on the Complications, Body Mass Index Changes, Endoscopic Findings and Causes of Revision. OBES SURG 31, 5275–5285 (2021). https://doi.org/10.1007/s11695-021-05683-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05683-5