Abstract
Purpose
Extreme obesity has been associated with cognitive deficits across the lifespan and may be a risk factor for dementia in later life. However, the relationship between obesity and domain-specific cognitive deficits is complicated by a body of literature that often fails to adequately account for medical and psychiatric conditions frequently co-occurring with extreme obesity.
Materials and Methods
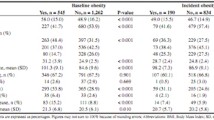
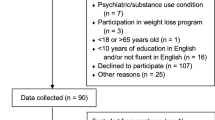
The present study included a cross-sectional evaluation of adults with extreme obesity (n=117) compared to lean control (n=46) participants on a brief cognitive battery using the NIH Toolbox and Rey Auditory Verbal Learning Test. Specifically, this study evaluated measures of executive functioning, attention, processing speed, learning, and memory while accounting for many common obesity-related medical and psychiatric comorbidities with known cognitive effects.
Results
Results revealed group differences with lower performances on measures of executive functioning, processing speed, and learning (ps<0.01) for participants with obesity. Reduced executive functioning was associated with abdominal obesity and medication use (ps<0.01) and together contributed significantly to overall modeling of cognition in individuals with obesity.
Conclusion
Individuals with extreme obesity in this sample showed lower cognitive performance on measures of executive functioning, processing speed, and learning compared to lean controls. Abdominal obesity was associated with executive functioning deficits independent of many common medical and psychiatric factors.

Similar content being viewed by others
References
Bischof GN, Park DC. Obesity and aging: consequences for cognition, brain structure, and brain function. Psychosom Med. 2015;77:697–709.
Smith E, Hay P, Campbell L, et al. A review of the association between obesity and cognitive function across the lifespan: implications for novel approaches to prevention and treatment: Obesity and cognitive function across lifespan. Obes Rev. 2011;12:740–55.
Prickett C, Brennan L, Stolwyk R. Examining the relationship between obesity and cognitive function: a systematic literature review. Obes Res Clin Pract. 2015;9:93–113.
Gunstad J, Lhotsky A, Wendell CR, et al. Longitudinal examination of obesity and cognitive function: results from the Baltimore longitudinal study of aging. Neuroepidemiology. 2010;34:222–9.
Elias MF, Elias PK, Sullivan LM, et al. Lower cognitive function in the presence of obesity and hypertension: the Framingham heart study. Int J Obes Relat Metab Disord. 2003;27:260–8.
Elias MF, Elias PK, Sullivan LM, et al. Obesity, diabetes and cognitive deficit: the Framingham Heart Study. Neurobiol Aging. 2005;26:11–6.
Gunstad J, Sanborn V, Hawkins M. Cognitive dysfunction is a risk factor for overeating and obesity. Am Psychol. 2020;75:219–34.
Cournot M, Marquie JC, Ansiau D, et al. Relation between body mass index and cognitive function in healthy middle-aged men and women. Neurology. 2006;67:1208–14.
Nguyen JCD, Killcross AS, Jenkins TA. Obesity and cognitive decline: role of inflammation and vascular changes. Front Neurosci. 2014;8:1–9.
Spyridaki EC, Avgoustinaki PD, Margioris AN. Obesity, inflammation and cognition. Curr Opin Behav Sci. 2016;9:169–75.
Solas M, Milagro FI, Ramírez MJ, et al. Inflammation and gut-brain axis link obesity to cognitive dysfunction: plausible pharmacological interventions. Curr Opin Pharmacol. 2017;37:87–92.
Galioto R, Alosco ML, Spitznagel MB, et al. Glucose regulation and cognitive function after bariatric surgery. J Clin Exp Neuropsychol. 2015;37:402–13.
Bubu OM, Andrade AG, Umasabor-Bubu OQ, et al. Obstructive sleep apnea, cognition and Alzheimer’s disease: a systematic review integrating three decades of multidisciplinary research. Sleep Med Rev. 2020;50:101250.
della Monica C, Johnsen S, Atzori G, et al. Rapid eye movement sleep, sleep continuity and slow wave sleep as predictors of cognition, mood, and subjective sleep quality in healthy men and women, aged 20–84 years. Front Psych. 2018;9:255.
Ng SK, Urquhart DM, Fitzgerald PB, et al. The relationship between structural and functional brain changes and altered emotion and cognition in chronic low back pain: a systematic review of MRI and fMRI studies. Clin J Pain. 2018;34:237–61.
Shenal BV, Harrison DW, Demaree HA. The neuropsychology of depression: a literature review and preliminary model. Neuropsychol Rev. 2003;13:33–42.
Sarwer DB, Heinberg LJ. A review of the psychosocial aspects of clinically severe obesity and bariatric surgery. Am Psychol. 2020;75:252–64.
Marek RJ, Ben-Porath YS, Windover A, Tarescavage AM, Merrell J, Ashton K, et al. Assessing psychosocial functioning of bariatric surgery candidates with the Minnesota Multiphasic Personality Inventory-2 Restructured Form (MMPI-2-RF). Obes Surg. 2013;10.
Suzuki J, Haimovici F, Chang G. Alcohol use disorders after bariatric surgery. Obes Surg. 2012;22:201–7.
Votruba K, Marshall D, Finks J, et al. Neuropsychological factors and bariatric surgery: a review. Curr Psychiatry Rep. 2014;16:448.
Callaghan BC, Reynolds EL, Banerjee M, et al. The prevalence and determinants of cognitive deficits and traditional diabetic complications in the severely obese. Diabetes Care. 2020;43:683–90.
American Diabetes Association. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. American Diabetes Association; 2003;26:s5–20.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi J-C, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care Lippincott Williams & Wilkins; 2005;43:1130–9.
Babor TF, Higgins-Biddle JC, Saunders JB, et al. The Alcohol Use Disorders Identification Test. Geneva: World Health Organization; 2001.
de Meneses-Gaya C. Alcohol Use Disorders Identification Test (AUDIT): an updated systematic review of psychometric properties. [Internet]. Psychol. Neurosci. Brazil: Pontifícia Universidade Católica do Rio de Janeiro; 20111003 [cited 2021 Jan 14]. p. 83. Available from: /fulltext/2011-13717-012.html
Ben-Porath YS, Tellegen A. MMPI-2-RF, Minnesota Multiphasic Personality Inventory-2 Restructured Form: manual for administration, scoring and interpretation. Minneapolis, MN: University of Minnesota Press : Distributed by NCS Pearson; 2011.
Tellegen A, Ben-Porath YS. Minnesota Multiphasic Persoality Inventory-2 Restructured Form: technical manual. Minneapolis, MN: University of Minnesota Press : Distributed by NCS Pearson; 2008.
Morgan CM, Borges MBF, Jorge MR. Questionnaire of Eating and Weight Patterns - Revised: an instrument to assess binge eating disorder. Rev Abpapal. 1998;20:130–9.
Parker K, Brennan L. Measurement of disordered eating in bariatric surgery candidates: a systematic review of the literature. Obes Res Clin Pract. 2015;9:12–25.
Schrepf A, Phan V, Clemens JQ, et al. ICD-10 codes for the study of chronic overlapping pain conditions in administrative databases. J Pain. 2020;21:59–70.
Weintraub S, Dikmen SS, Heaton RK, et al. Cognition assessment using the NIH Toolbox. Neurology. 2013;80:S54–64.
Rey A. L’ examen clinique en psychologie. Paris: Presses universitaires de France; 1964.
McMinn MR, Wiens AN, Crossen JR. Rey auditory-verbal learning test: development of norms for healthy young adults. Clin Neuropsychol. 1988;2:67–87.
Wilkinson GS, Robertson GJ. WRAT 4: wide range achievement test professional manual. Lutz: Psychological Assessment Resources, Inc.; 2006.
Manly JJ, Jacobs DM, Touradji P, et al. Reading level attenuates differences in neuropsychological test performance between African American and White elders. J Int Neuropsychol Soc. 2002;8:341–8.
Rothman KJ. No adjustments are needed for multiple comparisons. Epidimiology. 1990;1:43–6.
Feise RJ. Do multiple outcome measures require p-value adjustment? BMC Med Res Methodol. 2002;2:8.
Wang C, Chan JSY, Ren L, et al. Obesity reduces cognitive and motor functions across the lifespan. Neural Plast. 2016;2016:1–13.
Marek RJ, Ben-Porath YS, van Dulmen MHM, et al. Using the presurgical psychological evaluation to predict 5-year weight loss outcomes in bariatric surgery patients. Surg Obes Relat Dis. 2017;13:514–21.
Suciu BD, Micluţia IV. Clinical quest for associated cognitive impairment in major depressed patients. Psychiatr Q. 2020;91:749–59.
Lupien SJ, Maheu F, Tu M, et al. The effects of stress and stress hormones on human cognition: implications for the field of brain and cognition. Brain Cogn. 2007;65:209–37.
Hall PA. Executive-control processes in high-calorie food consumption. Curr Dir Psychol Sci. SAGE Publications Inc.; 2016;25:91–8.
Spitznagel MB, Garcia S, Miller LA, et al. Cognitive function predicts weight loss after bariatric surgery. Surg Obes Relat Dis. 2013;9:453–9.
Verbeken S, Braet C, Goossens L, et al. Executive function training with game elements for obese children: a novel treatment to enhance self-regulatory abilities for weight-control. Behav Res Ther. 2013;51:290–9.
Cuevas HE, Stuifbergen AK, Ward C. Participant perspectives of cognitive rehabilitation for type 2 diabetes: expectations and impact. J Aging Res. 2018;2018:1–9.
Miller LA, Crosby RD, Galioto R, Strain G, Devlin MJ, Wing R, et al. Bariatric surgery patients exhibit improved memory function 12 months postoperatively. Obes Surg. 2013;9.
Spitznagel MB, Alosco M, Strain G, et al. Cognitive function predicts 24-month weight loss success after bariatric surgery. Surg Obes Relat Dis. 2013;9:765–70.
Spitznagel MB, Alosco M, Galioto R, Strain G, Devlin M, Sysko R, et al. The role of cognitive function in postoperative weight loss outcomes: 36-month follow-up. Obes Surg. 2014;7.
Alosco ML, Galioto R, Spitznagel MB, et al. Cognitive function after bariatric surgery: evidence for improvement 3 years after surgery. Am J Surg. 2014;207:870–6.
Pedditizi E, Peters R, Beckett N. The risk of overweight/obesity in mid-life and late life for the development of dementia: a systematic review and meta-analysis of longitudinal studies. Age Ageing. Oxford Academic; 2016;45:14–21.
Napoli N, Shah K, Waters DL, et al. Effect of weight loss, exercise, or both on cognition and quality of life in obese older adults. Am J Clin Nutr. 2014;100:189–98.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval and Informed Consent Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Competing Interests
Dr. Callaghan consults for DynaMed, performs medical legal consultations including consultations for the Vaccine Injury Compensation Program, and receives research support from the American Academy of Neurology (AAN). Dr. Callaghan is funded by a NIH NIDDK R-01 award (DK115687). Dr. Reynolds is supported by NIH T32 (NS0007222). The authors declare no additional competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mulhauser, K., Reynolds, E.L., Callaghan, B.C. et al. Executive Functioning in Extreme Obesity: Contributions from Metabolic Status, Medical Comorbidities, and Psychiatric Factors. OBES SURG 31, 2669–2681 (2021). https://doi.org/10.1007/s11695-021-05319-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05319-8