Abstract
Purpose
Cardiovascular diseases (CVD) are one of the leading causes of mortality in obese patients. In this study, we investigated the effects of laparoscopic sleeve gastrectomy (LSG) operation on carotid intima-media thickness (CIMT), epicardial fat thickness (EFT), and serum endocan levels, which are independent predictors of subclinical atherosclerosis.
Materials and Methods
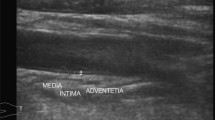
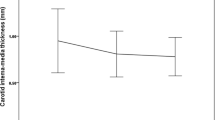
A total of 47 patients (35 females and 12 males) with a mean age of 38 ± 10.48 with standard indications for LSG were prospectively included in the study. Mean CIMT values with B-mode duplex ultrasound, EFT measurements with standard transthoracic 2D echocardiography, and serum endocan levels were measured before the operation and 6 months after the operation. Delta (Δ) values were obtained by subtracting sixth month values from baseline values.
Results
Body mass index (BMI) decreased significantly from an average of 47.31 ± 6.10 to 37.25 ± 5.61 kg/m2 in the sixth month after LSG (p < 0.001). EFT, CIMT, and serum endocan values decreased significantly in the sixth month after surgery (0.67 ± 0.15 vs. 0.60 ± 0.14 mm, p < 0.001; 1.07 ± 0.05 vs. 1.00 ± 0.14 mm, p < 0.001; and 89.18 ± 66.22 vs. 37.74 ± 15.37, p < 0.001, respectively). There were mild-moderate positive relationships between Δ-BMI and the values of EFT and CIMT (r = 0.386, p = 0.007 and r = 0.314, p = 0.024, respectively). We also found weak linear relationships between Δ-BMI and Δ-endocan (r = 0.267, p = 0.036), and between Δ-EFT and Δ-CIMT (r: 0.221; p: 0.046).
Conclusion
LSG can lead to reduction in the risk of cardiovascular disease by providing improvements in CIMT, EFT, and serum endocan values, which reflect early structural atherosclerotic changes in patients with severe obesity.

Similar content being viewed by others
References
Rosenthal RJ, Panel ISGE. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of> 12,000 cases. Surg Obes Relat Dis. 2012;8(1):8–19.
Fried M, Yumuk V, Oppert J, et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014;24(1):42–55.
Kasliwal RR, Kaushik M, Grewal HK, et al. Carotid ultrasound for cardiovascular risk prediction: from intima-media thickness to carotid plaques. J Indian Acad Echocardiogr Cardiovasc Imaging. 2017;1(1):39.
Nagy E, Jermendy AL, Merkely B, et al. Clinical importance of epicardial adipose tissue. Arch Med Sci. 2017;13(4):864–74.
Rosito GA, Massaro JM, Hoffmann U, et al. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation. 2008;117(5):605–13.
Tam WC, Hsieh MH, Yeh JS. Echocardiographic measurement of epicardial fat thickness. Acta Cardiol Sin. 2019;35(5):546–7.
Qiu C-R, Fu Q, Sui J, et al. Serum endothelial cell–specific molecule 1 (endocan) levels in patients with acute myocardial infarction and its clinical significance: a pilot study. Angiology. 2017;68(4):354–9.
Zhao T, Kecheng Y, Zhao X, et al. The higher serum endocan levels may be a risk factor for the onset of cardiovascular disease: a meta-analysis. Medicine (Baltimore). 2018;97(49):e13407.
Pfetsch V, Sanin V, Jaensch A, et al. Increased plasma concentrations of soluble ST2 independently predict mortality but not cardiovascular events in stable coronary heart disease patients: 13-year follow-up of the KAROLA study. Cardiovasc Drugs Ther. 2017;31(2):167–77.
Turk-Adawi K, Sarrafzadegan N, Fadhil I, et al. Cardiovascular disease in the Eastern Mediterranean region: epidemiology and risk factor burden. Nat Rev Cardiol. 2018;15(2):106–19.
Fried M, Yumuk V, Oppert J, et al. International Federation for Surgery of obesity and metabolic disorders-European chapter (IFSO-EC); European Association for the Study of obesity (EASO); European Association for the Study of Obesity Obesity Management Task Force (EASO OMTF). Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014;24(1):42–55.
Iacobellis G, Willens HJ. Echocardiographic epicardial fat: a review of research and clinical applications. J Am Soc Echocardiogr. 2009;22(12):1311–9.
Yacoub S, Hays S, Bolton D, Ponce S, Strauss M, Sarban V. Performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American Society of Echocardiography. 2019.
Hajar R. Risk factors for coronary artery disease: historical perspectives. Heart Views. 2017;18(3):109–14.
Kelly AS, Ryder JR, Marlatt KL, et al. Changes in inflammation, oxidative stress and adipokines following bariatric surgery among adolescents with severe obesity. Int J Obes. 2016;40(2):275–80.
Koliaki C, Liatis S, Kokkinos A. Obesity and cardiovascular disease: revisiting an old relationship. Metabolism. 2019;92:98–107.
Alexopoulos N, McLean DS, Janik M, et al. Epicardial adipose tissue and coronary artery plaque characteristics. Atherosclerosis. 2010;210(1):150–4.
Erdoğan T, Durakoğlugil ME, Çetin M, et al. Epicardial adipose tissue predicts carotid intima-media thickness independently of body mass index and waist circumference. Acta Cardiol Sin. 2019;35(1):32–41.
Nelson MR, Mookadam F, Thota V, et al. Epicardial fat: an additional measurement for subclinical atherosclerosis and cardiovascular risk stratification? J Am Soc Echocardiogr. 2011;24(3):339–45.
Tachibana M, Miyoshi T, Osawa K, et al. Measurement of epicardial fat thickness by transthoracic echocardiography for predicting high-risk coronary artery plaques. Heart Vessel. 2016;31(11):1758–66.
Nerlekar N, Brown AJ, Muthalaly RG, et al. Association of epicardial adipose tissue and high-risk plaque characteristics: a systematic review and meta-analysis. J Am Heart Assoc. 2017;6(8):e006379.
Sengul C, Cevik C, Ozveren O, et al. Echocardiographic epicardial fat thickness is associated with carotid intima-media thickness in patients with metabolic syndrome. Echocardiography (Mount Kisco, NY). 2011;28(8):853–8.
González N, Moreno-Villegas Z, González-Bris A, et al. Regulation of visceral and epicardial adipose tissue for preventing cardiovascular injuries associated to obesity and diabetes. Cardiovasc Diabetol. 2017;16(1):44.
Rubio-Guerra AF, Benítez-Maldonado DR, Lozano-Nuevo JJ, et al. Correlation between epicardial fat thickness and biochemical markers of metabolic risk. Med Clín (English Edition). 2018;151(6):236–8.
Erkan AF, Tanindi A, Kocaman SA, et al. Epicardial adipose tissue thickness is an independent predictor of critical and complex coronary artery disease by Gensini and syntax scores. Tex Heart Inst J. 2016;43(1):29–37.
Yamashita K, Yamamoto MH, Igawa W, et al. Association of epicardial adipose tissue volume and total coronary plaque burden in patients with coronary artery disease. Int Heart J. 2018;59(6):1219–26.
Iacobellis G. Epicardial fat: a new cardiovascular therapeutic target. Curr Opin Pharmacol. 2016;27:13–8.
Altin C, Erol V, Aydin E, et al. Impact of weight loss on epicardial fat and carotid intima media thickness after laparoscopic sleeve gastrectomy: a prospective study. Nutr Metab Cardiovasc Dis. 2018;28(5):501–9.
Natale F, Tedesco MA, Mocerino R, et al. Visceral adiposity and arterial stiffness: echocardiographic epicardial fat thickness reflects, better than waist circumference, carotid arterial stiffness in a large population of hypertensives. Eur J Echocardiogr. 2009;10(4):549–55.
Sengul C, Cevik C, Ozveren O, et al. Echocardiographic epicardial fat thickness is associated with carotid intima-media thickness in patients with metabolic syndrome. Echocardiography. 2011;28(8):853–8.
Nezu T, Hosomi N, Aoki S, et al. Carotid intima-media thickness for atherosclerosis. J Atheroscler Thromb. 2015;31989
Jonker FH, Van Houten VA, Wijngaarden LH, et al. Age-related effects of bariatric surgery on early atherosclerosis and cardiovascular risk reduction. Obes Surg. 2018;28(4):1040–6.
Domienik-Karłowicz J, Dzikowska-Diduch O, Lisik W, Chmura A, Pruszczyk P. Common carotid intima-media thickness assessment in morbidly obese patients undergoing bariatric surgery Ocena grubości kompleksu błona środkowa–błona wewnętrzna tętnicy szyjnej wspólnej u pacjentów z otyłością olbrzymią poddawanych operacjom bariatrycznym
Lambert G, de Oliveira Lima MM, Felici A, et al. Early regression of carotid intima-media thickness after bariatric surgery and its relation to serum leptin reduction. Obes Surg. 2018;28(1):226–33.
Tromba L, Tartaglia F, Carbotta S, et al. The role of sleeve gastrectomy in reducing cardiovascular risk. Obes Surg. 2017;27(5):1145–51.
Menon P, Kocher ON, Aird WC. Endothelial cell specific molecule-1 (ESM-1), a novel secreted proteoglycan stimulates vascular smooth muscle cell proliferation and migration. Am Heart Assoc. 2011;
Béchard D, Scherpereel A, Hammad H, et al. Human endothelial-cell specific molecule-1 binds directly to the integrin CD11a/CD18 (LFA-1) and blocks binding to intercellular adhesion molecule-1. J Immunol. 2001;167(6):3099–106.
Wang X-s, Yang W, Luo T, et al. Serum endocan levels are correlated with the presence and severity of coronary artery disease in patients with hypertension. Genet Test Mol Biomark. 2015;19(3):124–7.
Altintas N, Mutlu LC, Akkoyun DC, et al. Effect of CPAP on new endothelial dysfunction marker, endocan, in people with obstructive sleep apnea. Angiology. 2016;67(4):364–74.
Yang J, Yang Q, Yu S, et al. Endocan: a new marker for cancer and a target for cancer therapy. Biomed Rep. 2015;3(3):279–83.
Lv Y, Zhang Y, Shi W, et al. The association between Endocan levels and subclinical atherosclerosis in patients with type 2 diabetes mellitus. Am J Med Sci. 2017;353(5):433–8.
Steinberg HO, Chaker H, Leaming R, et al. Obesity/insulin resistance is associated with endothelial dysfunction. Implications for the syndrome of insulin resistance. J Clin Invest. 1996;97(11):2601–10.
Perticone F, Ceravolo R, Candigliota M, et al. Obesity and body fat distribution induce endothelial dysfunction by oxidative stress: protective effect of vitamin C. Diabetes. 2001;50(1):159–65.
Borzì AM, Buscemi C, Corleo D, et al. Endothelial function in obese patients treated with bariatric surgery. Diabetes Metab Synd Obes. 2020;13:247.
Yadav R, Hama S, Liu Y, et al. Effect of Roux-en-Y bariatric surgery on lipoproteins, insulin resistance, and systemic and vascular inflammation in obesity and diabetes. Front Immunol. 2017;8:1512.
Gorostegi-Anduaga I, Maldonado-Martín S, MartinezAguirre-Betolaza A, et al. Effects on cardiovascular risk scores and vascular age after aerobic exercise and nutritional intervention in sedentary and overweight/obese adults with primary hypertension: the EXERDIET-HTA randomized trial study. High Blood Press Cardiovasc Prev. 2018;25(4):361–8.
Gorostegi-Anduaga I, Pérez-Asenjo J, Aispuru GR, et al. Assessment of cardiovascular risk and vascular age in overweight/obese adults with primary hypertension: the EXERDIET-HTA study. Blood Press Monit. 2017;22(3):154–60.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cekici, Y., Kaya, B.C. & Elkan, H. The Effect of Laparoscopic Sleeve Gastrectomy on Subclinical Atherosclerosis in Patients with Severe Obesity. OBES SURG 31, 738–745 (2021). https://doi.org/10.1007/s11695-020-05121-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-05121-y