Abstract
Introduction
Preoperative very low energy diets (VLEDs) improve access during bariatric surgery. Compliance with traditional VLED is variable, mainly due to gastrointestinal side effects. Formulite™ is a new formulation of VLED, with higher protein, soluble fibre and probiotics.
Aims
To compare traditional VLED (Optifast™) with the new VLED (Formulite™) and assess compliance, weight loss, satisfaction, side effects and surgical access.
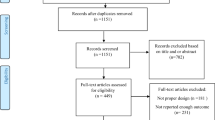
Methods
This was a randomised double-blinded study involving patients scheduled for bariatric surgery. The primary outcome was compliance, assessed by urinary ketone concentration and proportion of patients in ketosis at 2 weeks. Secondary outcomes were weight loss, satisfaction and patient reported outcomes, gastrointestinal side effects and operative conditions.
Results
There were 69 participants: 35 in the Formulite™ group and 34 in the Optifast™ group. Ketosis at 2 weeks was achieved in both groups (88.5% vs 83.3%, Formulite™ vs. Optifast™, p = 0.602). Urinary ketones were higher with Formulite™ (1.5 vs 15 mmol/L, p = 0.030). Total body weight loss percentage, hunger and operative conditions were similar in both groups. Formulite™ produced less flatulence (score 3 vs 2, p = 0.010) and emotional eating (score 2 vs 1, p = 0.037); however, Optifast™ ranked higher in terms of taste (score 4 vs 3, p = 0.001) and overall satisfaction (score 5 vs 7, p = 0.011).
Conclusions
Compliance over 2 weeks was high in both VLEDs with most subjects achieving ketosis. Overall satisfaction was moderately high, although variable. Whilst Formulite™ is a viable alternative to Optifast™, better formulations of VLED that addresses key adverse effects, whilst achieving ketosis, would be of significant value.



Similar content being viewed by others
Change history
01 July 2019
In the original article the name of author Alexandra Klejn was misspelled.
References
Colles SL, Dixon JB, Marks P, et al. Preoperative weight loss with a very-low-energy diet: quantitation of changes in liver and abdominal fat by serial imaging. Am J Clin Nutr. 2006;84(2):304–11.
Alami RS et al. Is there a benefit to preoperative weight loss in gastric bypass patients? A prospective randomized trial. Surg Obes Relat Dis. 2007;3(2):141–5.
Gerber P, Anderin C, Thorell A. Weight loss prior to bariatric surgery: an updated review of the literature. Scand J Surg. 2015;104:33–9.
Faria SL, Faria OP, Cardeal MA, et al. Effects of a very low calorie diet in the preoperative stage of bariatric surgery: a randomized trial. Surg Obes Relat Dis. 2015;11:230–7.
Van Nieuwenhove Y et al. Preoperative very low-calorie diet and operative outcome after laparoscopic gastric bypass: a randomized multicenter study. Arch Surg. 2011;146(11):1300–5.
Glenn NM, Raine KD, Spence JC. Mandatory weight loss during the wait for bariatric surgery. Qual Health Res. 2015;25(1):51–61.
Formulite. Formulite Home Page. 2018 [cited 2018 19 Oct 2018]; Available from: https://formulite.com.au/.
Santesso N, Akl EA, Bianchi M, et al. Effects of higher-versus lower-protein diets on health outcomes: a systematic review and meta analysis. Eur J Clin Nutr. 2012;66:780–8.
Dong JY, Zhang ZL, Wang PY, et al. Effects of high-protein diets on body weight, glycaemic control, blood lipids and blood pressure in type 2 diabetes: meta-analysis of randomised controlled trials. Br J Nutr. 2013;110:781–9.
Schwingshackl L, Hoffmann G. Long-term effects of low-fat diets either low or high protein on cardiovascular and metabolic risk factors: a systematic review and meta-analysis. Nutr J. 2013;12:48-2891-12-48.
De Luis DA et al. Effects of a high-protein/low carbohydrate versus a standard hypocaloric diet on adipocytokine levels and insulin resistance in obese patients along 9 months. J Diabetes Complicat. 2015;29:950–4.
Larsen TM, Dalskov SM, van Baak M, et al. Diets with high or low protein content and glycemic index for weight-loss maintenance. N Engl J Med. 2010;363:2102–13.
Nagarajan N, Morden A, Bischof D, et al. The role of fiber supplementation in the treatment of irritable bowel syndrome: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2015;27:1002–10.
Moayyedi P, Quigley EMM, Lacy BE, et al. The effect of fiber supplementation on irritable bowel syndrome: a systematic review and meta-analysis. Am J Gastroenterol. 2014;109:1367–74.
Lewis MC et al. Changes in liver size and fat content after treatment with Optifast very low calorie diet. Obes Surg. 2006;16(6):697–701.
Edholm D, Kullberg J, Haenni A, et al. Preoperative 4-week low-calorie diet reduces liver volume and intrahepatic fat, and facilitates laparoscopic gastric bypass in morbidly obese. Obes Surg. 2011;21(3):345–50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Statement
Ethics approval was obtained from the Avenue Ethics Committee (ref no. 210). The trial was registered with the Australian Clinical Trials Register (ACTRN 12616001091493 at www.anzctr.org.au).
Consent Statement
All participants provided written informed consent.
Conflict of Interest
The product Formulite™ was donated by the manufacturer for the purpose of this study.
Author 1: no conflicts of interest to declare.
Author 2: no conflicts of interest to declare.
Author 3: no conflicts of interest to declare.
Author 4: no conflicts of interest to declare.
Author 5: no conflicts of interest to declare.
Author 6: received a grant from the NHMRC, outside the submitted work.
Author 7: received grants from Johnson and Johnson, grants from Medtronic, grants from GORE, personal fees from GORE, grants from Applied Medical, grants from Apollo Endosurgery, grants and personal fees from Novo Nordisc, personal fees from Merck Sharpe and Dohme, outside the submitted work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Davenport, L., Johari, Y., Klejn, A. et al. Improving Compliance with Very Low Energy Diets (VLEDs) Prior to Bariatric Surgery—a Randomised Controlled Trial of Two Formulations. OBES SURG 29, 2750–2757 (2019). https://doi.org/10.1007/s11695-019-03916-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03916-2