Abstract
Background
Obesity and metabolic surgery is known to improve chronic inflammatory status. Whether improvement is related to anatomical changes or weight loss is still to debate.
Objective
The aim of this clinical trial is to compare the different bariatric procedures sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), and One-anastomosis gastric bypass (OAGB), pertaining to their effects on inflammation markers.
Methods
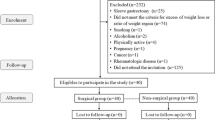
Patients who underwent SG, RYGB, or OAGB as a primary treatment for severe obesity were included. The data collected preoperatively (T0) and 1, 3, and 6 (T6) months after surgery included gender, weight, comorbidities and toxic habits at baseline, body mass index (BMI), waist circumference, total body weight loss in % (TBWL), leukocyte count in × 103/μl, C-reactive protein (CRP) in mg/l, HbA1c in %, aspartate transaminase in U/l, alanine transaminase in U/l, gamma-glutamyltransferase in U/l, bilirubin in mg/dl, cholesterol in mg/dl, and triglycerides in mg/dl.
Results
Four hundred sixty-eight patients were included. Drop-out rate was 25.8% at T6. Preoperatively the mean value of leukocytes and CRP was 7.4 × 103/μl ± 2 and 10.5 mg/l ± 8.1. At T6, mean value of leukocytes and CRP was 7.1 × 103/μl ± 1.9 (p = 0.075) and 7.2 mg/l ± 9.5 (p < 0.001). TBWL % at T6 was 24.2 ± 7.6 in the SG, 25.8 ± 5.9 in the RYGB and 25.5 ± 4.6 in the OAGB group. Comparing SG, RYGB, and OAGB in relation to leukocyte count and CRP no significant difference was seen between the groups.
Conclusion
CRP but not leukocyte count decreased after all three bariatric procedures but without any significance between the three groups. Surgically induced weight loss and not anatomical changes might play an important role for improvement in chronic inflammation.
Trial Registration
The National Clinical Trials number was NCT02697695 (https://clinicaltrials.gov/ct2/show/NCT02697695).




Similar content being viewed by others
Change history
27 June 2018
In Table 4 the column labeled “p values” and its data should be deleted.
Abbreviations
- SG:
-
Sleeve gastrectomy
- RYGB:
-
Roux-en-Y gastric bypass
- OAGB:
-
One-anastomosis gastric bypass
- BMI:
-
Body mass index
- WC:
-
Waist circumference
- EWL:
-
Excess weight loss
- TBWL:
-
Total body weight loss
- CRP:
-
C-reactive protein
- ICAM-1:
-
Intercellular adhesion molecules
- RNA:
-
Ribonucleic acid
- NF-κB:
-
Nuclear transcription factor kappa B
- TNF-α:
-
Tumor necrosis factor-α
- IL-1:
-
Interleukin-1
- IL-6:
-
interleukin-6
- BDNF:
-
Brain-derived neurotrophic factor
- T2DM:
-
Type 2 diabetes mellitus
- CD14:
-
Cluster of differentiation 14
- VLCD:
-
Very low-calorie diet
- SD:
-
Standard deviation
- NASH:
-
Non-alcoholic statosis hepatitis
- AST:
-
Aspartate transaminase
- ALT:
-
Alanine transaminase
- GGT:
-
Gamma-glutamyltransferase
- OSAS:
-
Obstructive sleep apnea
References
Hotamisligil GS. Inflammation, metaflammation and immunometabolic disorders. Nature. 2017;542(7640):177–85.
Medzhitov R. Origin and physiological roles of inflammation. Nature. 2008;454(7203):428–35.
Wellen KE, Hotamisligil GS. Inflammation, stress, and diabetes. J Clin Invest. 2005;115(5):1111–9.
Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444(7121):860–7.
Dahlman I, Elsen M, Tennagels N, et al. Functional annotation of the human fat cell secretome. Arch Physiol Biochem. 2012;118(3):84–91.
Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993;259(5091):87–91.
Krinninger P, Ensenauer R, Ehlers K, et al. Peripheral monocytes of obese women display increased chemokine receptor expression and migration capacity. J Clin Endocrinol Metab. 2014;99(7):2500–9.
Bochud M, Marquant F, Marques-Vidal PM, et al. Association between C-reactive protein and adiposity in women. J Clin Endocrinol Metab. 2009;94(10):3969–77.
Shemesh T, Rowley KG, Jenkins A, et al. Differential association of C-reactive protein with adiposity in men and women in an aboriginal community in Northeast Arnhem Land of Australia. Int J Obes. 2007;31(1):103–8.
Mortensen OH, Nielsen AR, Erikstrup C, et al. Calprotectin—a novel marker of obesity. PLoS One. 2009;4(10):e7419.
Hanusch-Enserer U, Cauza E, Spak M, et al. Acute-phase response and immunological markers in morbid obese patients and patients following adjustable gastric banding. Int J Obes Relat Metab Disord. 2003;27(3):355–61.
Netto BD, Bettini SC, Clemente AP, et al. Roux-en-Y gastric bypass decreases pro-inflammatory and thrombotic biomarkers in individuals with extreme obesity. Obes Surg. 2015;25(6):1010–8.
Schmidt MI, Duncan BB, Sharrett AR, et al. Markers of inflammation and prediction of diabetes mellitus in adults (atherosclerosis risk in communities study): a cohort study. Lancet. 1999;353(9165):1649–52.
van Wijk DF, Boekholdt SM, Arsenault BJ, Ahmadi-Abhari S, Wareham NJ, Stroes ES, et al. C-reactive protein identifies low-risk metabolically healthy obese persons: the European prospective investigation of Cancer-Norfolk Prospective Population Study. J Am Heart Assoc 2016;5(6).
Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386(9997):964–73.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med. 2017;376(7):641–51.
van Dielen FM, Buurman WA, Hadfoune M, et al. Macrophage inhibitory factor, plasminogen activator inhibitor-1, other acute phase proteins, and inflammatory mediators normalize as a result of weight loss in morbidly obese subjects treated with gastric restrictive surgery. J Clin Endocrinol Metab. 2004;89(8):4062–8.
Santos J, Salgado P, Santos C, et al. Effect of bariatric surgery on weight loss, inflammation, iron metabolism, and lipid profile. Scand J Surg. 2014;103(1):21–5.
Cottam DR, Schaefer PA, Shaftan GW, et al. Effect of surgically-induced weight loss on leukocyte indicators of chronic inflammation in morbid obesity. Obes Surg. 2002;12(3):335–42.
Park S, Kim YJ, Choi CY, et al. Bariatric surgery can reduce albuminuria in patients with severe obesity and normal kidney function by reducing systemic inflammation. Obes Surg. 2018;28(3):831–7.
Pontiroli AE, Frige F, Paganelli M, et al. In morbid obesity, metabolic abnormalities and adhesion molecules correlate with visceral fat, not with subcutaneous fat: effect of weight loss through surgery. Obes Surg. 2009;19(6):745–50.
Rao SR. Inflammatory markers and bariatric surgery: a meta-analysis. Inflamm Res. 2012;61(8):789–807.
Cummings DE. Endocrine mechanisms mediating remission of diabetes after gastric bypass surgery. Int J Obes. 2009;33(Suppl 1):S33–40.
Billeter AT, Senft J, Gotthardt D, et al. Combined non-alcoholic fatty liver disease and type 2 diabetes mellitus: sleeve gastrectomy or gastric bypass?—a controlled matched pair study of 34 patients. Obes Surg. 2016;26(8):1867–74.
Patterson RE, Sears DD. Metabolic effects of intermittent fasting. Annu Rev Nutr. 2017;37:371–93.
Marathe PH, Gao HX, Close KL. American Diabetes Association Standards of Medical Care in Diabetes 2017. J Diabetes. 2017;9(4):320–4.
Chiappetta S, Stier C, Squillante S, et al. The importance of the Edmonton Obesity Staging System in predicting postoperative outcome and 30-day mortality after metabolic surgery. Surg Obes Relat Dis. 2016;12(10):1847–55.
Guidelines for reporting results in bariatric surgery. Standards Committee, American Society for Bariatric Surgery. Obes Surg. 1997;7(6):521–2.
Nijhuis J, van Dielen FM, Fouraschen SM, et al. Endothelial activation markers and their key regulators after restrictive bariatric surgery. Obesity (Silver Spring). 2007;15(6):1395–9.
Pekala P, Kawakami M, Vine W, et al. Studies of insulin resistance in adipocytes induced by macrophage mediator. J Exp Med. 1983;157(4):1360–5.
Rubino F, Nathan DM, Eckel RH, et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Diabetes Care. 2016;39(6):861–77.
De Luca M, Angrisani L, Himpens J, et al. Indications for surgery for obesity and weight-related diseases: position statements from the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO). Obes Surg. 2016;26(8):1659–96.
Rubino F, Nathan DM, Eckel RH, et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Surg Obes Relat Dis. 2016;12(6):1144–62.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248–256.e5.
Afshar S, Malcomson F, Kelly SB, Seymour K, Woodcock S, Mathers JC. Biomarkers of colorectal cancer risk decrease 6 months after Roux-en-Y gastric bypass surgery. Obes Surg 2017.
Illan-Gomez F, Gonzalvez-Ortega M, Orea-Soler I, et al. Obesity and inflammation: change in adiponectin, C-reactive protein, tumour necrosis factor-alpha and interleukin-6 after bariatric surgery. Obes Surg. 2012;22(6):950–5.
Shimobayashi M, Albert V, Woelnerhanssen B, et al. Insulin resistance causes inflammation in adipose tissue. J Clin Invest. 2018;128(4):1538–50.
Yadav R, Hama S, Liu Y, et al. Effect of roux-en-Y bariatric surgery on lipoproteins, insulin resistance, and systemic and vascular inflammation in obesity and diabetes. Front Immunol. 2017;8:1512.
Dixon JB, O'Brien PE. Obesity and the white blood cell count: changes with sustained weight loss. Obes Surg. 2006;16(3):251–7.
Thorand B, Baumert J, Doring A, et al. Sex differences in the relation of body composition to markers of inflammation. Atherosclerosis. 2006;184(1):216–24.
Kassi E, Spilioti E, Nasiri-Ansari N, et al. Vascular inflammation and atherosclerosis: the role of estrogen receptors. Curr Med Chem. 2015;22(22):2651–65.
Fenske WK, Dubb S, Bueter M, et al. Effect of bariatric surgery-induced weight loss on renal and systemic inflammation and blood pressure: a 12-month prospective study. Surg Obes Relat Dis. 2013;9(4):559–68.
Iannelli A, Anty R, Schneck AS, et al. Inflammation, insulin resistance, lipid disturbances, anthropometrics, and metabolic syndrome in morbidly obese patients: a case control study comparing laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy. Surgery. 2011;149(3):364–70.
Lips MA, van Klinken JB, Pijl H, et al. Weight loss induced by very low calorie diet is associated with a more beneficial systemic inflammatory profile than by Roux-en-Y gastric bypass. Metabolism. 2016;65(11):1614–20.
Brandhorst S, Choi IY, Wei M, et al. A periodic diet that mimics fasting promotes multi-system regeneration, enhanced cognitive performance, and health span. Cell Metab. 2015;22(1):86–99.
Gill RS, Karmali S, Sharma AM. The potential role of the Edmonton obesity staging system in determining indications for bariatric surgery. Obes Surg. 2011;21(12):1947–9.
Casimiro Perez JA, Fernandez Quesada C, Del Val Groba Marco M, et al. Obesity Surgery Score (OSS) for prioritization in the bariatric surgery waiting list: a need of public health systems and a literature review. Obes Surg. 2018;28(4):1175–84.
Iyengar NM, Gucalp A, Dannenberg AJ, et al. Obesity and cancer mechanisms: tumor microenvironment and inflammation. J Clin Oncol. 2016;34(35):4270–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Informed Consent
Informed consent was obtained from all the individual participants included in the study.
Ethical Approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Chiappetta, S., Schaack, H.M., Wölnerhannsen, B. et al. The Impact of Obesity and Metabolic Surgery on Chronic Inflammation. OBES SURG 28, 3028–3040 (2018). https://doi.org/10.1007/s11695-018-3320-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3320-y