Abstract
Background
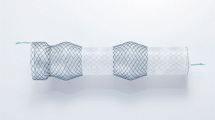
Use of a self-expandable metal stent (SEMS) as an initial intervention for leaks after laparoscopic sleeve gastrectomy (LSG) has increased. We assessed the efficacy and safety of SEMS in the treatment of post-LSG leaks, and the determinants of repeated rounds of stenting.
Methods
A retrospective chart review was conducted at a university hospital in Saudi Arabia. The study included patients who developed leaks after undergoing LSG between October 2011 and April 2016.
Results
Sixty-four patients (mean age, 35.69 ± 10.71 years) were included; 55% were males. The mean estimated size of the defect was 1.18 cm; partially covered SEMS and fully covered SEMS were used as the initial stents in 82.81 and 17.19% patients, respectively. One round of stenting was required in most patients (82.81%), two rounds in 10.94%, and three rounds in 6.25%. Clinical success was achieved in 93.75% patients, including 78.13% in the first round, 89.06% by the second round, and 93.75% by the third round. A higher proportion of patients who needed one round of stenting received a partially covered SEMS compared to those who needed two rounds (91.11 vs. 42.86%, p < 0.01). Additionally, the rate of migration in patients who underwent two rounds was higher than that in patients who underwent one round (42.86 vs. 5.26%, p < 0.01) of stenting.
Conclusion
Repeated stenting for leaks after LSG is an effective and safe intervention. The efficacy of partially covered SEMS appears superior to that of the fully covered SEMS.


Similar content being viewed by others
References
Li P, Fu P, Chen J, et al. Laparoscopic Roux-en-Y Gastric bypass vs. laparoscopic sleeve gastrectomy for morbid obesity and diabetes mellitus: a meta-analysis of sixteen recent studies. Hepatogastroenterology. 2013;60(121):132–7.
Kumar N, et al. Endoscopic management of complications after gastrointestinal weight loss surgery. Clin Gastroenterol Hepatol. 2013;11(4):343–353.
Moszkowicz D, Arienzo R, Khettab I, et al. Sleeve gastrectomy severe complications: is it always a reasonable surgical option? Obes Surg. 2013;23(5):676–86. https://doi.org/10.1007/s11695-012-0860-4.
Benedix F, Poranzke O, Adolf D, et al. Staple line leak after primary sleeve gastrectomy-risk factors and mid-term results: do patients still benefit from the weight loss procedure? Obes Surg. 2017;27(7):1780–8. https://doi.org/10.1007/s11695-017-2543-7.
van Boeckel PG, Sijbring A, Vleggaar FP, et al. Systematic review: temporary stent placement for benign rupture or anastomotic leak of the oesophagus. Aliment Pharmacol Ther. 2011;33(12):1292–301. https://doi.org/10.1111/j.1365-2036.2011.04663.x.
Puli SR, Spofford IS, Thompson CC. Use of self-expandable stents in the treatment of bariatric surgery leaks: a systematic review and meta-analysis. Gastrointest Endosc. 2012;75(2):287–93. https://doi.org/10.1016/j.gie.2011.09.010.
Eisendrath P, Deviere J. Major complications of bariatric surgery: endoscopy as first-line treatment. Nat Rev Gastroenterol Hepatol. 2015;12(12):701–10. https://doi.org/10.1038/nrgastro.2015.151.
Rosenthal RJ, International Sleeve Gastrectomy Expert P, Diaz AA, et al. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis. 2012;8(1):8–19. https://doi.org/10.1016/j.soard.2011.10.019.
Almadi MA, Bamihriz F, Aljebreen AM. Fatal aortoesophageal fistula bleeding after stenting for a leak post sleeve gastrectomy. World J Gastrointest Surg. 2013;5(12):337–40. https://doi.org/10.4240/wjgs.v5.i12.337.
Hutter MM, Schirmer BD, Jones DB, et al. First report from the American College of Surgeons bariatric surgery center network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg. 2011;254(3):410–420; discussion 20-2. https://doi.org/10.1097/SLA.0b013e31822c9dac.
Murino A, Arvanitakis M, Le Moine O, et al. Effectiveness of endoscopic management using self-expandable metal stents in a large cohort of patients with post-bariatric leaks. Obes Surg. 2015;25(9):1569–76. https://doi.org/10.1007/s11695-015-1596-8.
Kim J, Azagury D, Eisenberg D, et al. ASMBS position statement on prevention, detection, and treatment of gastrointestinal leak after gastric bypass and sleeve gastrectomy, including the roles of imaging, surgical exploration, and nonoperative management. Surg Obes Relat Dis. 2015;11(4):739–48. https://doi.org/10.1016/j.soard.2015.05.001.
van Wezenbeek MR, de Milliano MM, Nienhuijs SW, et al. A specifically designed stent for anastomotic leaks after bariatric surgery: experiences in a tertiary referral hospital. Obes Surg. 2016;26(8):1875–80. https://doi.org/10.1007/s11695-015-2027-6.
Garofalo F, Noreau-Nguyen M, Denis R, et al. Evolution of endoscopic treatment of sleeve gastrectomy leaks: from partially covered to long, fully covered stents. Surg Obes Relat Dis. 2017;13(6):925–32. https://doi.org/10.1016/j.soard.2016.12.019.
van Halsema EE. Wong Kee Song LM, Baron TH, et al. safety of endoscopic removal of self-expandable stents after treatment of benign esophageal diseases. Gastrointest Endosc. 2013;77(1):18–28. https://doi.org/10.1016/j.gie.2012.09.001.
Guzaiz N, Arabi M, Khankan A, et al. Gastroesophageal stenting for the management of post sleeve gastrectomy leak. A single institution experience. Saudi Med J. 2016;37(12):1339–43. https://doi.org/10.15537/smj.2016.12.15761.
Nedelcu M, Manos T, Cotirlet A, et al. Outcome of leaks after sleeve gastrectomy based on a new algorithm addressing leak size and gastric stenosis. Obes Surg. 2015;25(3):559–63. https://doi.org/10.1007/s11695-014-1561-y.
Almadi MA, Aljebreen AM, Bamihriz F. Resolution of an esophageal leak and posterior gastric wall necrosis with esophageal self-expandable metal stents. World J Gastroenterol. 2013;19(40):6931–3. https://doi.org/10.3748/wjg.v19.i40.6931.
Aryaie AH, Singer JL, Fayezizadeh M, et al. Efficacy of endoscopic management of leak after foregut surgery with endoscopic covered self-expanding metal stents (SEMS). Surg Endosc. 2017;31(2):612–7. https://doi.org/10.1007/s00464-016-5005-8.
DaVee T, Irani S, Leggett CL, et al. Stent-in-stent technique for removal of embedded partially covered self-expanding metal stents. Surg Endosc. 2016;30(6):2332–41. https://doi.org/10.1007/s00464-015-4475-4.
Dirks K, Schulz T, Schellmann B, et al. Fatal hemorrhage following perforation of the aorta by a barb of the Gianturco-Rosch esophageal stent. Z Gastroenterol. 2002;40(02):81–4. https://doi.org/10.1055/s-2002-20204.
Funding
The authors extend their sincere appreciation to the Deanship of Scientific Research at King Saud University for its funding of this research through the Research Group Project number RGP-279.
Author information
Authors and Affiliations
Contributions
Majid A Almadi: Analysis of the data, writing, drafting, revising the article for important intellectual content, and final approval of the version to be published.
Fahad Bamihriz, Abdullah Aldohayan: Revising the article critically for important intellectual content and final approval of the version to be published.
Mohanned Eltayeb, Salem Thaniah, Ahmed Aljammaz, Othman Alharbi, Nahla Azzam, Abdulrahman Aljebreen: Acquisition of data, revising the article critically for important intellectual content, and final approval of the version to be published.
Corresponding author
Ethics declarations
Ethical Approval Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Almadi, M.A., Bamihriz, F., Alharbi, O. et al. Use of Self-Expandable Metal Stents in the Treatment of Leaks Complicating Laparoscopic Sleeve Gastrectomy: A Cohort Study. OBES SURG 28, 1562–1570 (2018). https://doi.org/10.1007/s11695-017-3054-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-3054-2