Abstract
Purpose
Obesity in fertile women has negative effect on fertility. Anti-mullerian hormone (AMH) represents a good index of fertility, and it is considered a marker of ovarian reserve and of polycystic ovarian syndrome (PCOS) gravity. Previous studies evaluated the relationship between obesity and AMH with contradictory results.
The aim of the study was to investigate the relationship between obesity and AMH and the changes of AMH in obese women in reproductive age submitted to bariatric surgery.
Materials and Methods
Fifty-five obese patients between 18 and 39 years with (29 patients) and without PCOS (26 patients) were compared with a control group of normal weight women with (24 patients) and without PCOS (19 patients). Fourteen obese women with PCOS and 18 without PCOS underwent to bariatric surgery. Serum AMH, testosterone, androstenedione, and DHEAS were performed in all patients before and 1 year after surgical intervention.
Results
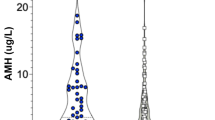
AMH was significantly higher in the PCOS groups (p < 0.001), both in obese (5.84 ± 3.94 ng/ml) and non-obese women (7.35 ± 4.39 ng/ml). AMH was positively related to testosterone (p < 0.0001), androstenedione (p = 0.0005), and DHEAS (p = 0.003). After bariatric surgery, AMH levels were reduced in the both PCOS (p = 0.02) and non-PCOS group (p = 0.04).
Conclusions
AMH levels are elevated in PCOS patients regardless of the body weight. Bariatric surgery is effective in the normalization of AMH levels (a possible indirect marker of better fertility) only in obese patients with PCOS.


Similar content being viewed by others
References
Bessesen DH. Update on obesity. J Clin Endocrinol Metab. 2008;93(6):2027–34.
Gosman GG, King WC, Schrope B, et al. Reproductive health of women electing bariatric surgery. Fertil Steril. 2010;94(4):1426–31.
Maheshwari A, Stofberg L, Bhattacharya S. Effect of overweight and obesity on assisted reproductive technology—a systematic review. Hum Reprod Update. 2007;13(5):433–44.
Pournaras DJ, Manning L, Bidgood K, et al. Polycystic ovary syndrome is common in patients undergoing bariatric surgery in a British center. Fertil Steril. 2010;94(2):e41.
Glueck CJ, Dharashivkar S, Wang P, et al. Obesity and extreme obesity, manifest by ages 20–24 years, continuing through 32–41 years in women, should alert physicians to the diagnostic likelihood of polycystic ovary syndrome as a reversible underlying endocrinopathy. Eur J Obstet Gynecol Reprod Biol. 2005;122(2):206–12.
Hart R, Norman R. Polycystic ovarian syndrome—prognosis and outcomes. Best Pract Res Clin Obstet Gynaecol. 2006;20(5):751–78.
Hart R, Doherty DA. The potential implications of a PCOS diagnosis on a woman’s long-term health using data linkage. J Clin Endocrinol Metab. 2015;100(3):911–9.
Pandey S, Pandey S, Maheshwari A, et al. The impact of female obesity on the outcome of fertility treatment. J Hum Reprod Sci. 2010;3(2):62–7.
Moran LJ, Norman RJ. The effect of bariatric surgery on female reproductive function. J Clin Endocrinol Metab. 2012;97(12):4352–4.
Patel JA, Colella JJ, Esaka E, et al. Improvement in infertility and pregnancy outcomes after weight loss surgery. Med Clin North Am. 2007;91:515–28.
Maggard MA, Yermilov I, Li Z, et al. Pregnancy and fertility following bariatric surgery: a systematic review. J Am Med Assoc. 2008;300:2286–96.
Deitel M, Stone E, Kassam HA, et al. Gynecologic-obstetric changes after loss of massive excess weight following bariatric surgery. J Am Coll Nutr. 1988;7(2):147–53.
Kaska L, Kobiela J, Abacjew-Chmylko A, et al. Nutrition and pregnancy after bariatric surgery. ISRN Obes. 2013;2013:492060.
Freeman EW, Gracia CR, Sammel MD, et al. Association of anti-mullerian hormone levels with obesity in late reproductive-age women. Fertil Steril. 2007;87(1):101–6.
Halawaty S, ElKattan E, Azab H, et al. Effect of obesity on parameters of ovarian reserve in premenopausal women. J Obstet Gynaecol Can. 2010;32(7):687–90.
Skałba P, Cygal A, Madej P, et al. Is the plasma anti-mullerian hormone (AMH) level associated with body weight and metabolic and hormonal disturbances in women with and without polycystic ovary syndrome? Eur J Obstet Gynecol Reprod Biol. 2011;158(2):254–9.
Usta T, Oral E. Is the measurement of anti-Müllerian hormone essential? Curr Opin Obstet Gynecol. 2012;24(3):151–7.
Merhi M. Relationship of bariatric surgery to Mullerian-inhibiting substance levels. Fertil Steril. 2008;90:221–4.
Bhandari S, Ganguly I, Bhandari M, et al. Effect of sleeve gastrectomy bariatric surgery-induced weight loss on serum AMH levels in reproductive aged women. Gynecol Endocrinol. 2016;17:1–4.
Escobar-Morreale HF, Botella-Carretero JI, Alvarez-Blasco F, et al. The polycystic ovary syndrome associated with morbid obesity may resolve after weight loss induced by bariatric surgery. J Clin Endocrinol Metab. 2005;90(12):6364–9.
Nybacka Å, Carlström K, Fabri F, et al. Serum antimullerian hormone in response to dietary management and/or physical exercise in overweight/obese women with polycystic ovary syndrome: secondary analysis of a randomized controlled trial. Fertil Steril. 2013;100(4):1096–102.
Georgopoulos NA, Saltamavros AD, Decavalas G, et al. Serum AMH, FSH, and LH levels in PCOS. Fertil Steril. 2010;93(3):e13.
Su HI, Sammel MD, Freeman EW, et al. Body size affects measures of ovarian reserve in late reproductive age women. Menopause. 2008;15(857–61):70.
Nakhuda GS. The role of mullerian inhibiting substance in female reproduction. Curr Opin Obstet Gynecol. 2008;20(257–64):71.
Merhi ZO. Impact of bariatric surgery on female reproduction. Fertil Steril. 2009;92(5):1501–8.
Eid GM, Cottam DR, Velcu LM, et al. Effective treatment of polycystic ovarian syndrome with Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2005;1(2):77–80.
Malinowski SS. Nutritional and metabolic complications of bariatric surgery. Am J Med Sci. 2006;331(4):219–25.
Bojsen-Møller KN. Mechanisms of improved glycaemic control after Roux-en-Y gastric bypass. Dan Med J. 2015;62(4):B5057.
Acknowledgements
None
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
For this type of study, formal consent is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Chiofalo, F., Ciuoli, C., Formichi, C. et al. Bariatric Surgery Reduces Serum Anti-mullerian Hormone Levels in Obese Women With and Without Polycystic Ovarian Syndrome.. OBES SURG 27, 1750–1754 (2017). https://doi.org/10.1007/s11695-016-2528-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2528-y