Abstract
Background
Currently, Roux-en-Y gastric bypass (RYGB) is one of the most widely used bariatric surgeries. Banding the pouch forms a banded gastric bypass operation, an accepted and frequently used variant. Placing a silastic ring around the pouch to band the gastric bypass operation increases the restriction mechanism. However, the ubiquitous use of the banded gastric bypass remains controversial. One of the controversies is the effect of the silastic ring on patients’ perception of their well being after surgery because of the frequency of vomiting. A prospective, blindly randomized, comparative trial was undertaken to resolve this controversy.
Method
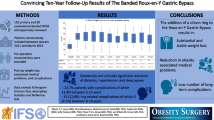
Four hundred subjects scheduled for gastric bypass surgery were randomized into two arms of the trial, 200 with a silastic ring (WR) and 200 without (NR). After 2-year follow-up, the variables associated with the scores of Bariatric Analysis and Reporting Outcome System (BAROS) were analyzed.
Results
The initial median weight (125 kg), BMI (47), and age (36 years) were the same in both the NR and WR groups. The median excess weight loss, weight regain, and incidence of vomiting were 71, 10.5, and 7.75 %, respectively, in the NR group vs. 75.4 and 1.1, and 24.4 % in the WR group. The mean QOL score was 79 % in the NR group vs. 80 % in the WR group.
Conclusion
After 2-year follow-up, silastic ring placement in the RYGB resulted in greater weight loss and weight stability and a threefold greater incidence of vomiting. There was no difference in the scores in the quality of life analysis.

Similar content being viewed by others
References
NIH Conference. Gastrointestinal surgery for severe obesity. Consensus development conference panel. Ann Intern Med. 1991;115(12):956–61.
Duval K, Marceau P, Lescelleur O, et al. Health-related quality of life in morbid obesity. Obes Surg. 2006;16(5):574–9.
Sjostrom L. Review of the key results from the swedish obese subjects (sos) trial—a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273(3):219–34.
Colquitt JL, Picot J, Loveman E, et al. Surgery for obesity. Cochrane Database Syst Rev. 2009;2:CD003641.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23(4):427–36.
Fobi MA, Lee H. The surgical technique of the fobi-pouch operation for obesity (the transected silastic vertical gastric bypass). Obes Surg. 1998;8(3):283–8.
Capella RF, Capella JF, Mandec H, et al. Vertical banded gastroplasty-gastric bypass: preliminary report. Obes Surg. 1991;1(4):389–95.
Blackburn GL, Hutter MM, Harvey AM, et al. Expert panel on weight loss surgery: executive report update. Obesity (Silver Spring). 2009;17(5):842–62.
Oria HE, Moorehead MK. Bariatric analysis and reporting outcome system (baros). Obes Surg. 1998;8(5):487–99.
Bessler M, Daud A, Kim T, et al. Prospective randomized trial of banded versus nonbanded gastric bypass for the super obese: early results. Surg Obes Relat Dis. 2007;3(4):480–4. discussion 4-5.
Halverson JD, Koehler RE. Gastric bypass: analysis of weight loss and factors determining success. Surgery. 1981;90(3):446–55.
Arasaki CH, Del Grande JC, Yanagita ET, et al. Incidence of regurgitation after the banded gastric bypass. Obes Surg. 2005;15(10):1408–17.
Clarke MG, Wong K, Pearless L, et al. Laparoscopic silastic ring mini-gastric bypass: a single centre experience. Obes Surg. 2013;23(11):1852–7.
Novais PF, Junior IR, Shiraga EC, et al. Food aversions in women during the 2 years after roux-en-y gastric bypass. Obes Surg. 2011;21(12):1921–7.
Fobi M, Lee H, Igwe D, et al. Band erosion: Incidence, etiology, management and outcome after banded vertical gastric bypass. Obes Surg. 2001;11(6):699–707.
Salinas A, Salinas HM, Santiago E, et al. Silastic ring vertical gastric bypass: cohort study with 83% rate of 5-year follow-up. Surg Obes Relat Dis. 2009;5(4):455–8.
Crampton NA, Izvornikov V, Stubbs RS. Silastic ring gastric bypass: a comparison of two ring sizes: a preliminary report. Obes Surg. 1997;7(6):495–9.
Brethauer SA, Aminian A, Romero-Talamas H, et al. Can diabetes be surgically cured? Long-term metabolic effects of bariatric surgery in obese patients with type 2 diabetes mellitus. Ann Surg. 2013;258(4):628–36. discussion 36-7.
Livhits M, Mercado C, Yermilov I, et al. Patient behaviors associated with weight regain after laparoscopic gastric bypass. Obes Res Clin Pract. 2011;5(3):e169–266.
Awad W, Garay A, Martinez C. Ten years experience of banded gastric bypass: does it make a difference? Obes Surg. 2012;22(2):271–8.
Wolf AM, Falcone AR, Kortner B, et al. Baros: an effective system to evaluate the results of patients after bariatric surgery. Obes Surg. 2000;10(5):445–50.
Ministério da Saúde do Brasil. Portaria n. 424 de 19/03/2013. In: Gabinete do Ministro, editor. Diário Oficial da União 2013.
Conflict of Interest
A summary statement: IRINEU RASERA JUNIOR is Ethicon J&J proctorship.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rasera, I., Coelho, T.H., Ravelli, M.N. et al. A Comparative, Prospective and Randomized Evaluation of Roux-en-Y Gastric Bypass With and Without the Silastic Ring: A 2-Year Follow Up Preliminary Report on Weight Loss and Quality of Life. OBES SURG 26, 762–768 (2016). https://doi.org/10.1007/s11695-015-1851-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1851-z