Abstract
Background
Anesthesia is able to modulate the balance between proinflammatory and anti-inflammatory cytokine production during surgery. The aim of this study is to assess the effect of three anesthesia approaches, total intravenous anesthesia (TIVA), inhalation anesthesia, and xenon anesthesia, on sieric levels of nitric oxide (NO), IL6, IL10, and TNFα in obese patients undergoing Roux-en-Y laparoscopic gastric bypass.
Methods
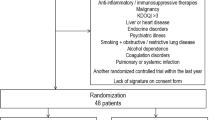
Thirty adult morbidly obese patients (BMI > 35) scheduled for Roux-en-Y laparoscopic gastric bypass were randomly recruited and allocated to TIVA (N = 10), inhalation anesthesia (SEV, N = 10), and xenon anesthesia (XE, N = 10). Exclusion criteria were ASA IV, age <18 or >60 years, and Mallampati IV. Opioid dosage and ventilation parameters were standardized. Sieric levels of NO, IL6, IL10, and TNFα were assessed at T0 (before induction of anesthesia), T1 (end of surgery), and T2 (12 h after the end of surgery). We compared the relative cytokine level variations (delta) at T1 and T2 and the cytokine exposure levels calculated as the area under the curve (AUC) between T0 and T2 in the XE and non-XE (SEV + TIVA) groups.
Results
At T1, we found a significant ΔIL10 (reduction) and ΔTNFα (reduction) between XE and SEV (p < 0.05) and XE and TIVA (p < 0.05) groups. At T2, ΔIL10 was still significant. Furthermore, we found a reduced AUC value for TNFα in the XE group.
Conclusions
Xenon anesthesia seems able to inhibit postoperative proinflammatory cytokine imbalance in morbidly obese patients undergoing Roux-en-Y laparoscopic gastric bypass; the reduced ΔTNFα at T1 and the reduced global exposition to TNFα in the XE group may explain the reduced ΔIL10 at T1 and T2.

Similar content being viewed by others
References
Gaylord HR, Simpson BT. Effect of certain anaesthetics and loss of blood upon growth of transplanted mouse cancer. J Cancer Res. 1916;1:379.
Schneemilch CE, Hachenberg T, Ansorge S, et al. Effects of different anaesthetic agents on immune cell function in vitro. Eur J Anaesthesiol. 2005;22(8):616–23.
Inada T, Yamanouchi Y, Jomura S, et al. Effect of propofol and isoflurane anaesthesia on the immune response to surgery. Anaesthesia. 2004;59(10):954–9.
Moudgil GC, Singal DP, Gordon J. Comparative effects of halothane and isoflurane anaesthesia on perioperative lymphocyte function. Anesthesiology. 1992;77:354.
Moudgil GC, Gordon J, Forrest JB. Comparative effects of volatile anaesthetic agents and nitrous oxide on human leucocyte chemotaxis in vitro. Can Anaesth Soc J. 1984;31(6):631–7.
Helmy SA, Wahby MA, El-Nawaway M. The effect of anaesthesia and surgery on plasma cytokine production. Anaesthesia. 1999;54(8):733–8.
Mikawa K, Akamatsu H, Nishina K, et al. Propofol inhibits human neutrophil functions. Anesth Analg. 1998;87:695–700.
Nishina K, Akamatsu H, Mikawa K. The inhibitory effects of thiopental, midazolam and ketamine on human neutrophil functions. Anesth Analg. 1998;86:159–65.
Bidri M, Royer B, Averlant G, et al. Inhibition of mouse mast cell proliferation and proinflammatory mediator release by benzodiazepines. Immunopharmacology. 1999;43:75–86.
Helmy SAK, Al-Attiyah RJ. The immunomodulatory effects of prolonged intravenous infusion of propofol versus midazolam in critically ill surgical patients. Anaesthesia. 2001;56:4.
Crozier TA, Muller JE, Quittkat D, et al. The effect of anaesthesia on the cytokine responses to abdominal surgery. Br J Anaesth. 1994;72:280–5.
Gilliland HE, Armstrong MA, Carabine U, et al. The choice of anesthetic maintenance technique influences the anti-inflammatory cytokine to abdominal surgery: contrasting response between patients and isolate CPB circuits. Anesth Analg. 1999;89:7.
El Azab SR, Rosseel PMJ, De Lange JJ, et al. Effect of VIMA with sevoflurane versus TIVA with propofol or midazolam–sufentanil on the cytokine response during CABG surgery. Eur J Anaesthesiol. 2002;19:276–82.
Schneemilch CE, Ittenson A, Ansorge S, et al. Effect of 2 anesthetic techniques on the postoperative proinflammatory and anti-inflammatory cytokine response and cellular immune function to minor surgery. J Clin Anesth. 2004;17:517–27.
McBride WT, Armstrong MA, McBride SJ. Immunomodulation: an important concept in modern anaesthesia. Anaesthesia. 1996;51:465–73.
Sheeran P, Hall GM. Cytokines in anaesthesia. Br J Anaesth. 1997;78:201–19.
Walton B. Effects of anaesthesia and surgery on immune status. Br J Anaesth. 1979;51:37–43.
Chassard D, Bruguerolle B. Chronobiol Anest Anesthesiol. 2004;100:413–27.
Shenkin A, Fraser WD, Series J, et al. The serum interleukin-6 response to elective surgery. Lymphokine Res. 1989;8:123–7.
Cruickshank AM, Fraser WD, Burns HJG, et al. Response of serum interleukin-6 in patients undergoing elective surgery of varying severity. Clin Sci. 1990;79:161–5.
Naito Y, Tamai S, Shingu K, et al. Responses of plasma adrenocorticotropic hormone, cortisol, and cytokines during and after upper abdominal surgery. Anesthesiology. 1992;77:426–31.
Gogos CA, Drosou E, Bassaris HP, et al. Pro- versus anti-inflammatory cytokine profile in patients with severe sepsis: a marker for prognosis and future therapeutic options. J Infect Dis. 2000;181:176–80.
Abramo A, Di Salvo C, Foltran F, Forfori F, Anselmino M, Giunta F. Xenon anesthesia improves respiratory gas exchanges in morbidly obese patients. J Obes. 2010;2010. pii:421593.
Conflict of Interest
All the authors (Antonio Abramo, Claudio Di Salvo, Giacomo Baldi, Elena Marini, Marco Anselmino, Guido Salvetti, Francesco Giunta, and Francesco Forfori) declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abramo, A., Di Salvo, C., Baldi, G. et al. Xenon Anesthesia Reduces TNFα and IL10 in Bariatric Patients. OBES SURG 22, 208–212 (2012). https://doi.org/10.1007/s11695-011-0433-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-011-0433-y