Abstract
Cerebral microhaemorrhage is a commonly identified neuropathological consequence of mild traumatic brain injury (mTBI) and can be identified in vivo using susceptibility weighted imaging (SWI). This study aimed to determine whether SWI-detected microhaemorrhages are more common in individuals after a single, first-ever, mTBI event relative to trauma controls (TC) and to investigate whether a linear relationship exists between microhaemorrhage numbers and cognition or symptom reporting in the post-acute period after injury, independently of age, psychological status and premorbid level of functioning. Microhaemorrhagic lesions were identified by expert clinical examination of SWI for 78 premorbidly healthy adult participants who were admitted to hospital after a traumatic injury and had suffered a first-ever mTBI (n = 47) or no head strike (n = 31). Participants underwent objective cognitive examination of processing speed, attention, memory, and executive function as well as self-reported post-concussion symptomatology. Bootstrapping analyses were used as data were not normally distributed. Analyses revealed that the mTBI group had significantly more microhaemorrhages than the TC group (Cohen’s d = 0.559). These lesions were only evident in 28% of individuals. The mTBI participants demonstrated a significant linear association between number of microhaemorrhages and processing speed, independently of age, psychological status, or premorbid level of functioning. This study shows that a single mTBI causes cerebral microhaemorrhages to occur in a minority of premorbidly healthy individuals. Greater microhaemorrhage count is independently associated with slower processing speed, but not symptom reporting, during the post-acute injury period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mild traumatic brain injury (mTBI) that results in hospital treatment is estimated to occur in 300–400/100,000 individuals per year (Voss et al., 2015). Approximately 80% of these individuals are expected to make a full cognitive recovery within 3 months of injury (Carroll, Cassidy et al., 2004). The cognitive domains most commonly affected by mTBI are speed of processing, attention, memory and executive function (Carroll et al., 2014). During the normal recovery period, and for those who do not recover fully in the typical timeframe (Carroll et al., 2014), cognitive impairment significantly contributes to disability and poor psychosocial outcome after injury (Benedictus et al., 2010; Caplain et al., 2017; Ponsford et al., 2003).
Microhaemorrhagic lesions are one of the most commonly identified neuropathological consequences of mTBI (van der Horn et al., 2018) and can be identified in vivo using susceptibility weighted imaging (SWI) (Huang et al., 2015). It has broadly been accepted that groups of individuals with mTBI have more SWI-related microhaemorrhagic lesions than orthopaedic or healthy control participants (Tate et al., 2017; Trifan et al., 2017; van der Horn et al., 2018). The clinical consequences of microhaemorrhagic lesions continue to be debated, however. Some studies have found no significant relationship between the presence of SWI-identified microhaemorrhagic lesions and cognitive function or symptom reporting (Einarsen et al., 2019; Tate et al., 2017; van der Horn et al., 2018). Others have reported a relationship between the presence of microhaemorrhages and adverse neurological and functional outcome (de Haan et al., 2017; Park et al., 2009), cognitive outcome (Huang et al., 2015; Irimia et al., 2022; Studerus-Germann et al., 2018), post-concussion symptoms (Studerus-Germann et al., 2018) and presence of recent onset depression (Wang et al., 2014).
Problematically, all these studies varied substantially with respect to the MRI scanner magnetic field strength and within study scanner consistency, comprehensiveness of outcome evaluation, time since injury, extent of control group matching, inclusion of elderly (> 60 years), presence of psychiatric history and history of previous mTBIs. Further, no previous study controlled for age or premorbid level of cognitive function. All of these variables have been shown to significantly impact microhaemorrhagic lesion presence and/or lesion detection and/or cognition and symptom reporting (Carroll, Cassidy et al., 2004; Haller et al., 2018; Lange et al., 2011; Massey et al., 2015; Ponsford, 2013; Robles et al., 2022; Salthouse, 2009; Stern, 2002; Stulemeijer et al., 2008; Terry et al., 2019; Vernooij et al., 2008). Consequently, the specificity of previous findings with respect to the presence of mTBI-related microhaemorrhagic lesions and the impact of these lesions on cognition and/or symptom reporting remains open to question.
One additional limitation of all prior studies particularly undermines the validity of past conclusions. No previous study that has examined the relationship between microhaemorrhagic lesions and outcome, (Einarsen et al., 2019; Huang et al., 2015; Studerus-Germann et al., 2018; Tate et al., 2017; van der Horn et al., 2018) has investigated or controlled for the potential impact of psychological factors on this relationship. It has been well established that psychological status significantly affects both symptom reporting and cognitive performance after mTBI (Cassidy et al., 2014; Lange et al., 2011; Snell et al., 2015). Consequently, the absence of methodological or statistical controls for the substantial influence of psychological factors on outcome in previous research is highly problematic as it prevents valid inferential conclusions being drawn from these studies.
The present prospective study aimed to investigate post-acute (6–12 weeks after injury) outcome in a premorbidly healthy group of adults, less than 60 years of age, who had suffered a first-ever mTBI, and compare it to a premorbidly healthy group of trauma control adults, who were well-matched for age, sex, premorbid level of functioning, injury cause, involvement in litigation and current psychological status. It was hypothesised that the presence of microhaemorrhagic lesions in the mTBI group would be linearly associated with cognitive function and post-concussion symptomatology after controlling for age, psychological status and premorbid level of function.
Method
Participants
Participants comprised individuals, excluding professional athletes and war veterans, who had suffered any traumatic injury (systemic and/or head) between September 2015 and December 2019, and been consecutively admitted to The Alfred hospital or Royal Melbourne Hospital, Melbourne, Australia, in the preceding 6–12 weeks. Detailed description of the recruitment process and the recruitment decision tree have been reported previously (Anderson & Fitzgerald, 2020; Anderson & Jordan, 2020). All admitted trauma patients were approached for recruitment consideration. The mTBI group comprised 47 premorbidly healthy adults (36 male) aged 18–60 years, whose traumatic injury included a head strike and fulfilled criteria for a mTBI event as defined by the World Health Organisation criteria (Carroll, Cassidy, Holm et al., 2004), which can be briefly summarised as (i) 1 or more of confusion or disorientation, loss of consciousness for 30 min or less, post-traumatic amnesia less than 24 h; (ii) Glasgow Coma Scale score of 13–15 after 30 min. Excluded individuals were those with: any previous neurological history, including documented mTBI; any history of heavy alcohol consumption, intravenous or regular Class A drug use; history of any past or current significant psychiatric disorder; current TBI as a result of physical assault/attack; lack of conversational English fluency. The TC participants comprised 31 premorbidly healthy adults (27 male) aged 18–60 years, whose traumatic injury had not included a head strike and who did not report any symptoms of mTBI; this group had the same exclusion criteria as the mTBI group. No ethnic group differences existed. All participants provided informed consent and the project was approved by The Alfred hospital and Royal Melbourne Hospital Human Research Ethics Committees.
Measures
Premorbid cognitive functioning
The Wechsler Test of Adult Reading (WTAR) (Wechsler, 2001) is a word reading task, from which accurate estimates of premorbid intellectual functioning (PreIQ) can be derived in individuals with mTBI (Steward et al., 2017).
Processing speed
The Symbol Digit Modality Test – (SDMT) is a measure of processing speed that is sensitive to cognitive impairment after mTBI (McCauley et al., 2014). It requires individuals to provide the correct number that corresponds to a given symbol, according to a reference key at the top of the page. On this version of the SDMT, the final score was number of correct items within 2 min.
Attention
The Digit Span subtest from the Wechsler Adult Intelligence Scale – 4th Edition (Wechsler, 2008) is a valid, reliable and widely-used measure of attention that is recommended for use in TBI research (Wilde et al., 2010). Digit Span Total (DSp) is a global measure of attention; raw scores rather than aged-scaled scores were used to enable comparative analyses with other cognitive measures.
Memory
The Rey Auditory Verbal Learning Test (RAVLT) (Schmidt, 1996) is a reliable and valid measure of verbal memory (Helmes, 2000). The total number of items learned on the five list learning trials (Total) assessed acquisition; it has demonstrated sensitivity to TBI samples (Schoenberg et al., 2006).
Executive function
The difference between Trail Making Tests A and B was used as a measure of mental flexibility (Lezak, 1995). This measure has been shown to be sensitive to executive dysfunction after mTBI (Spreen & Strauss, 1998).
Post-concussion symptoms
The Rivermead Post Concussion Symptoms Questionnaire (RPQ) is a widely used measure of post-concussion symptomatology. It assesses physical (10 items), psychological (3 items) and cognitive (3 items) symptoms experienced during the past 24 h, with each item on a 5-point likert scale (0–4) (King et al., 1995). It has been shown to be elevated after mTBI and other conditions (Cassidy et al., 2014; Ettenhofer & Barry, 2012; Laborey et al., 2014).
Psychological distress
Two widely used, valid and reliable questionnaires of psychological distress were used: The Inventory of Depressive Symptomatology (IDS) measures severity of overall depression (Rush et al., 1996). The Beck Anxiety Inventory (BAI) measures anxiety symptomatology (Beck & Steer, 1993). To reduce the number of variables and increase the power of calculations, a Psychological Distress Index was calculated by summing the raw score of the IDS and BAI.
Assessment of performance validity
The Digit Span (DSp) subtest from the Wechsler Adult Intelligence Scale, 4th Edition (WAIS-IV) (Wechsler, 2008) was used as a measure of effort (Iverson & Tulsky, 2003). Participants were identified as having problematic effort on testing if they failed on the subscales of Age Scaled Score Total (Fail = 5 or less) and Longest Digits Forward (Fail = 4 or less) (Iverson & Tulsky, 2003), which have been shown to have a likelihood ratio that successfully identifies poor effort (Babikian et al., 2006; Schutte & Axelrod, 2013).
Procedure
Following recruitment on the ward within 1–4 days of injury, participants returned to the hospital for neuropsychological examination and MRI scans, conducted on the same day, 6–10 weeks after injury. Neuropsychological measures were conducted in the following sequence for all participants: SDMT, WTAR, RAVLT, DSp, TMT, RPQ, IDS, BAI.
SWI data acquisition
Neuroimaging was performed using a 3T MR scanner (PRISMA, Siemens Healthcare) with a 32-channel head coil. The SWI sequence was acquired as part of a longer clinical research protocol in the transverse orientation (TE = 20ms, TR = 29ms, flip angle = 15°, matrix = 202 × 384, FOV 157 × 210; voxel size 0.55 × 0.55 × 1.5mm3).
Lesion identification
Number of SWI-related microhaemorrhagic lesions on each scan was determined concurrently by two raters: a neuroradiologist and a neurosurgical fellow. Each rater had more than 10 years of clinical practice reviewing MRI scans acquired for traumatic brain injury; both raters were blinded to group classification. Any disagreement concerning lesion identification was resolved through consensus. Prior to any consensus discussions occurring, 70% of the sample was randomly selected and correlations were calculated to determine inter-rater reliability of the raters’ decisions. Consistent with previous research (Cheng et al., 2013; Cordonnier et al., 2009; Gregoire et al., 2009) inter-rater reliability in the current study was excellent (r = .99). Cerebral microhaemorrhagic lesions were defined as hypointense foci, less than 10 mm in diameter (Colbert et al., 2010) on SWI data, that were not compatible with vascular flow void (based on sulcal location or linear shape), artefacts from adjacent bone or sinus, or non-haemorrhagic iron/mineral deposition in basal ganglia and other subcortical structures, or as part of a larger intra-parenchymal haemorrhagic lesion (≥ 10 mm) (Greenberg et al., 2009; Nandigam et al., 2009). Sample images from selected study participants are provided in Fig. 1.
If there was doubt as to the aetiology of any foci, the lesions were not considered to be haemorrhagic lesions (Tong et al., 2003). Both raters considered that it was not possible to reliably manually count the absolute number of microhaemorrhages present in cases that had more than 20 microhaemorrhages. Consequently, to conservatively examine group differences, cases that were found to have more than 20 microhaemorrhages were coded as having 20 microhaemorrhages, rather than making estimates of larger microhaemorrhage numbers. A similar approach has been adopted by others when assessing numbers of microhaemorrhagic lesions using SWI images (McKinney et al., 2012).
Statistical analysis
Statistical analysis was conducted using the Statistical Program for the Social Sciences (SPSS Version 26.0; SPSS, Inc., Chicago, IL). Data were screened for relevant assumptions for all inferential statistics employed in the analyses. The distribution of microhaemorrhage count was severely skewed. Consequently, consistent with recommended statistical practice for managing non-normally distributed data (Field, 2013), analyses involving the number of microhaemorrhages were undertaken using bootstrapping, with 2,000 samples used in the bootstrapping analyses and bias corrected accelerated confidence intervals identified.
Chi-square tests-for-independence and multivariate analyses of variance (MANOVAs) were conducted to investigate group differences for demographic and clinical variables. MANOVAs were also undertaken to identify any group differences in objective cognition and endorsement of post-concussion symptoms. Bootstrapped t-tests were undertaken to compare groups on the number of microhaemorrhages in each group and bootstrapped partial Pearson correlations were conducted to investigate whether linear relationships existed between cognitive variables and the number of microhaemorrhages. As estimates of premorbid IQ are more accurate indicators of level of premorbid functioning than education (Bright & van der Linde, 2020), premorbid IQ was used as the measure of premorbid level of function.
Results
The demographic details and injury characteristics for each group are presented in Table 1.
The groups were well matched on all demographic and injury variables, with the exception of number of days between injury and assessment; the mTBI participants were assessed approximately 9 weeks after injury, whereas the TC participants were assessed, on average, 1 week earlier. The primary analyses of interest were between group comparisons of SWI-detected microhaemorrhagic lesions and within group correlational analyses, neither of which would be affected by this group difference. Consequently, to maximise power, we did not control for this variable. The groups contained equivalent proportions of litigants (13–15%), and one individual failed the assessment of performance validity. This individual was in the TC group, and on inspection was found to have 9 years of education and a predicted premorbid IQ at the cusp of the Borderline and Low Average ranges. It has been suggested that use of Digit Span, as a measure of performance validity, is likely to be less accurate in individuals with Borderline levels of general cognition (Babikian et al., 2006). Consequently, given that the individual’s performance validity status was questionable and they were also in the TC group, making their cognitive performances irrelevant to the primary analyses of interest, they were retained in the sample to maximise power.
Between group comparisons of cognitive performance and endorsement of post-concussion symptoms are shown in Table 2.
The groups did not differ with respect to objective cognition in any domain. They endorsed equivalent numbers of symptoms, and effect sizes for all analyses were small (partial η2 < 0.05) or very small (partial η2 < 0.01).
Between group comparison of number of microhaemorrhages identified on SWI revealed that the mTBI group had significantly more microhaemorrhages (\(\stackrel{-}{X}\)=2.446, SD = 5.853) than the TC group (\(\stackrel{-}{X}\)=0.129, SD = 0.341) [t(46.47) = 2.708, 95% CI: 0.0879–4.154]; this difference was associated with a medium effect size (Cohen’s d = 0.559). Of note, bootstrapping analyses provide 95% confidence intervals rather than p values as indicators of significance, with only those confidence intervals that do not contain 0.00 considered significant (Field, 2013).
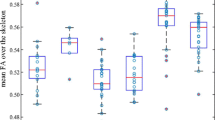
Figure 2 shows the distribution of microhaemorrhagic lesions within the groups for each individual.
For the TC group, 13% of the sample demonstrated microhaemorrhagic lesions, all of whom exhibited only a single lesion. In contrast, for the mTBI group, 28% of the sample demonstrated lesions, with 70% of those with microhaemorrhagic lesions showing more than one lesion and 30% of those with lesions demonstrating more than 20 lesions.
Lobar distribution of microhaemorrhages is presented in Table 3.
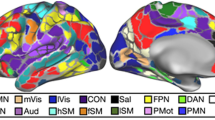
Lesion distribution primarily involved dorsolateral prefrontal cortex, orbitofrontal cortex, temporal pole and basal temporal lobe, inferior parietal lobule and the precuneus.
After covarying for age, premorbid level of functioning and psychological status, partial correlational analyses were conducted between the number of microhaemorrhages and the cognitive and symptom reporting variables for the mTBI group; these are shown in Table 4.
A significant partial linear correlation between number of microhaemorrhages and speed of processing was evident, with processing speed slowing as the number of microhaemorrhages increased. There were no other significant correlations between the number of microhaemorrhages and other measures of cognition or the symptom reporting variable. The same pattern of significance was evident for the combined mTBI and TC sample, with a significant linear association evident between processing speed and number of microhaemorrhages (r=-.272, CI: − 0.440 - − 0.077). The lack of variance in number of microhaemorrhages in the TC group prevented this analysis from being undertaken with the TC group alone.
Discussion
This study showed that the mTBI group had greater numbers of SWI-detected microhaemorrhagic lesions than the TC group and that the number of microhaemorrhagic lesions was linearly associated with cognitive function in the head injured group. Specifically, the presence of more microhaemorrhagic lesions was associated with slower processing speed. Location of microhaemorrhagic lesions was primarily in the frontal and temporal lobes, which is consistent with previous findings in individuals with mTBI (Park et al., 2009).
The current finding of greater numbers of SWI-related microhaemorrhagic lesions in those who have suffered a mTBI, relative to a control group, is consistent with recent literature (Tate et al., 2017; Trifan et al., 2017; van der Horn et al., 2018). The present study also replicated a previous finding, which showed that a minority of individuals with mTBI suffer microhaemorrhagic lesions, and that most of these individuals suffer four or more lesions (van der Horn et al., 2018); this contrasts with the single haemorrhagic lesion evident for the small minority of the TC sample that showed any lesion.
The present study demonstrated that there is a direct association between number of microhaemorrhages and speed of processing in the post-acute period after a first-ever mTBI event. Unlike previous research, the current association was found while controlling for psychological status, age and premorbid level of functioning, indicating that the identified association is independent of these factors (Massey et al., 2015; Salthouse, 2009; Stern, 2002; Terry et al., 2019). In contrast to expectations, there was no evidence of a similarly independent linear relationship between the number of SWI-detected microhaemorrhages and measures of attention, memory, executive function or post-concussion symptom reporting in either group. Ostensibly, this contrasts earlier findings that have shown relationships between microhaemorrhages and these variables. As previously reported relationships were found without controlling for age, premorbid level of functioning and psychological status, however, past studies cannot address the question of whether independent associations between these variables exist. The current findings indicate that there is no evidence of a linear relationship existing between number of microhaemorrhages and attention, memory, executive function, or post-concussion symptom reporting that is independent of age, psychological status and premorbid level of functioning.
The relationship between number of microhaemorrhages and processing speed, but not other domains of cognition, may be explained by the repeated finding that post-acute changes in processing speed after mTBI have larger effect sizes than changes in other cognitive domains (Frencham et al., 2005). Therefore, any relationship between lesion number and cognition is most likely to be evident in the domain of processing speed. This is supported by the distribution of the lesions in the present study. The location of these lesions corresponds with functional imaging findings that have identified functional and effective connectivity networks that underpin task performance on the SDMT – the measure of processing speed used in this study (Silva et al., 2019). Specifically, it has been shown that networks located in the frontoparietal, temporoparietal and inferior frontal cortices as well as the default-mode network (involving precuneus, posterior cingulate and inferior frontal cortices) underlie SDMT performance. These locations correspond well with the distribution of microhaemorrhages in the current sample.
The lack of relationship between symptom reporting and lesion number is consistent with the post-acute mTBI literature, which has repeatedly demonstrated that psychological status is more predictive of symptom reporting than other measures of injury severity (Cassidy et al., 2014; Silver, 2014). Given the relatively small number of individuals in the current study who had evidence of microhaemorrhages, however, further research examining this question with a larger sample size is warranted.
In sum, although the current study did not demonstrate an average difference in processing speed performance between those with mTBI and those without, there was clear evidence to show that mTBI causes multiple microhaemorrhagic lesions in a minority of individuals. In addition, the minority of those individuals who suffer microhaemorrhages are at significantly increased risk of experiencing slowed processing speed, with increases in the number of lesions associated with greater slowing in processing. It is noteworthy that the significant relationship between processing speed and lesion number for some individuals with mTBI is evident late in the ‘normal’ recovery period (9-weeks post-mTBI), when complete/almost complete recovery is expected for most individuals (Cassidy et al., 2004). The present study also shows that the reduction in processing speed is not due to age, psychological status or premorbid level of functioning. While it is not possible to determine whether the microhaemorrhages directly caused the slowing in processing speed from the current study’s methodology, this possibility clearly warrants future attention. Irrespective of whether a clear causal relationship can be established, however, the current findings suggest that patient care of individuals with mTBI may benefit from clinical management and rehabilitation support that integrate this risk profile in clinical decision-making. This is relevant even when patients are late in the ‘typical’ recovery period.
The primary limitation of the current study was the modest sample size. In particular, the small number of individuals who demonstrated microhaemorrhagic lesions prevented examination of whether there was a predictive relationship between microhaemorrhagic lesion numbers and processing speed performance. Another limitation associated with small sample sizes is the increased risk of making Type II errors. Thus, it is possible that the current study did not identify group differences in cognition due to the modest sample size. Examining the effect sizes of the between group analyses indicates this is relatively unlikely, however, as all effect sizes of non-significant group comparisons were very small. The sample size was considered adequate for bootstrapping analyses (Chernick, 2008), indicating that the partial correlation analyses were unlikely significantly influenced by the modest sample size. A final potential limitation of this study is the possibility that individuals may have suffered pre-traumatic microbleeds, unrelated to the trauma event. Given that the TC and mTBI groups were equivalently pre-morbidly healthy, however, there is no reason to believe that the number of possible pre-traumatic bleeds would have differed between the groups. Consequently, this possibility does not affect the implications that can be drawn from (a) the reported group difference in microhaemorrhagic count and (b) the relationship between processing speed and microhaemorrhagic count.
Conclusions
In conclusion, this study indicates that a single mTBI seems to cause multiple microhaemorrhagic lesions for a minority of premorbidly healthy adults. Further, for this minority, there is a significantly increased likelihood of experiencing progressively slower processing speed as the number of lesions increases, even at 9 weeks post-injury. While it is not possible to determine if the relationship between number of lesions and processing speed is causal from the current study, the clinical implications of these findings are nevertheless important. Specifically, they raise the question of whether an individual’s mTBI-related microhaemorrhagic lesion load might be an influential factor in the cognitive recovery trajectory after mTBI for some individuals. It is possible that higher lesion load could be associated with slower processing speed and therefore slower cognitive recovery in a minority of individuals with mTBI. Thus, these findings highlight a possible pathological mechanism that might be contributing to variations in cognitive recovery after a single mTBI event in premorbidly healthy adults. Further research will be needed to answer this clinically important question.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Anderson, J. F. I., & Fitzgerald, P. (2020). Associations between coping style, illness perceptions and self-reported symptoms after mild traumatic brain injury in prospectively studied pre-morbidly healthy individuals. Neuropsychol Rehabil, 1115–1128.
Anderson, J. F. I., & Jordan, A. S. (2020). An observational study of the association between sleep disturbance, fatigue and cognition in the post-acute period after mild traumatic brain injury in prospectively studied premorbidly healthy adults. Neuropsychol Rehabil, 1–22.
Babikian, T., Boone, K. B., Lu, P., & Arnold, G. (2006). Sensitivity and specificity of various digit span scores in the detection of suspect effort. The Clinical Neuropsychologist, 20(1), 145–159.
Beck, A. T., & Steer, R. A. (1993). Beck anxiety Inventory Manual. Psychological Corporation.
Benedictus, M. R., Spikman, J. M., & van der Naalt, J. (2010). Cognitive and behavioral impairment in traumatic brain injury related to outcome and return to work. Archives Of Physical Medicine And Rehabilitation, 91(9), 1436–1441.
Bright, P., & van der Linde, I. (2020). Comparison of methods for estimating premorbid intelligence. Neuropsychol Rehabil, 30(1), 1–14.
Caplain, S., Blancho, S., Marque, S., Montreuil, M., & Aghakhani, N. (2017). Early detection of poor outcome after mild traumatic brain Injury: Predictive factors using a Multidimensional Approach a pilot study. Frontiers In Neurology, 8, 666.
Carroll, L. J., Cassidy, J. D., Cancelliere, C., Cote, P., Hincapie, C. A., Kristman, V. L., Holm, L. W., Borg, J., Nygren-de Boussard, C., & Hartvigsen, J. (2014). Systematic review of the prognosis after mild traumatic brain injury in adults: Cognitive, psychiatric, and mortality outcomes: Results of the International collaboration on mild traumatic brain Injury Prognosis. Archives Of Physical Medicine And Rehabilitation, 95(3 Suppl), 152–173.
Carroll, L. J., Cassidy, J. D., Peloso, P. M., Borg, J., von Holst, H., Holm, L., Paniak, C., Pepin, M., & Injury, W. H. O. C. C. T. F. o. M. T. B. (2004). Prognosis for mild traumatic brain injury: Results of the WHO collaborating Centre Task Force on mild traumatic brain Injury. Journal Of Rehabilitation Medicine, 43(Suppl), 84–105.
Carroll, L. J., Cassidy, J. D., Holm, L., Kraus, J., Coronado, V. G., & Injury, W. H. O. C. C. T. F. o. M. T. B. (2004). Methodological issues and research recommendations for mild traumatic brain injury: The WHO collaborating Centre Task Force on mild traumatic brain Injury. Journal Of Rehabilitation Medicine, 43(Suppl), 113–125.
Cassidy, J. D., Carroll, L. J., Peloso, P. M., Borg, J., von Holst, H., Holm, L., Kraus, J., Coronado, V. G., & Injury, W. H. (2004). O. C. C. T. F. o. M. T. B. Incidence, risk factors and prevention of mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med(43 Suppl), 28–60.
Cassidy, J. D., Cancelliere, C., Carroll, L. J., Cote, P., Hincapie, C. A., Holm, L. W., Hartvigsen, J., Donovan, J., de Nygren-, C., Kristman, V. L., & Borg, J. (2014). Systematic review of self-reported prognosis in adults after mild traumatic brain injury: Results of the International collaboration on mild traumatic brain Injury Prognosis. Archives Of Physical Medicine And Rehabilitation, 95(3 Suppl), 132–151.
Cheng, A. L., Batool, S., McCreary, C. R., Lauzon, M. L., Frayne, R., Goyal, M., & Smith, E. E. (2013). Susceptibility-weighted imaging is more reliable than T2*-weighted gradient-recalled echo MRI for detecting microbleeds. Stroke, 44(10), 2782–2786.
Chernick, M. R. (2008). Bootstrap methods: A guide for practitioners and researchers (2nd ed.). Wiley-Interscience.
Colbert, C. A., Holshouser, B. A., Aaen, G. S., Sheridan, C., Oyoyo, U., Kido, D., & Ashwal, S. (2010). Value of cerebral microhemorrhages detected with susceptibility-weighted MR Imaging for prediction of long-term outcome in children with nonaccidental trauma. Radiology, 256(3), 898–905.
Cordonnier, C., Potter, G. M., Jackson, C. A., Doubal, F., Keir, S., Sudlow, C. L., Wardlaw, J. M., & Al-Shahi Salman, R. (2009). Improving interrater agreement about brain microbleeds: Development of the Brain Observer MicroBleed Scale (BOMBS). Stroke, 40(1), 94–99.
de Haan, S., de Groot, J. C., Jacobs, B., & van der Naalt, J. (2017). The association between microhaemorrhages and post - traumatic functional outcome in the chronic phase after mild traumatic brain injury. Neuroradiology, 59(10), 963–969.
Einarsen, C. E., Moen, K. G., Haberg, A. K., Eikenes, L., Kvistad, K. A., Xu, J., Moe, H. K., Tollefsen, M. H., Vik, A., & Skandsen, T. (2019). Patients with mild traumatic brain Injury recruited from both hospital and primary care settings: A controlled longitudinal magnetic resonance imaging study. Journal Of Neurotrauma, 36(22), 3172–3182.
Ettenhofer, M. L., & Barry, D. M. (2012). A comparison of long-term postconcussive symptoms between university students with and without a history of mild traumatic brain injury or orthopedic injury. Journal Of The International Neuropsychological Society, 18(3), 451–460.
Field, A. (2013). Discovering Statistics using IBM SPSS Statistics. SAGE Publications.
Frencham, K. A., Fox, A. M., & Maybery, M. T. (2005). Neuropsychological studies of mild traumatic brain injury: A meta-analytic review of research since 1995. Journal Of Clinical And Experimental Neuropsychology, 27(3), 334–351.
Greenberg, S. M., Vernooij, M. W., Cordonnier, C., Viswanathan, A., Al-Shahi Salman, R., Warach, S., Launer, L. J., Van Buchem, M. A., Breteler, M. M., & Study, M., G (2009). Cerebral microbleeds: A guide to detection and interpretation. Lancet Neurology, 8(2), 165–174.
Gregoire, S. M., Chaudhary, U. J., Brown, M. M., Yousry, T. A., Kallis, C., Jager, H. R., & Werring, D. J. (2009). The Microbleed Anatomical Rating Scale (MARS): Reliability of a tool to map brain microbleeds. Neurology, 73(21), 1759–1766.
Haller, S., Vernooij, M. W., Kuijer, J. P. A., Larsson, E. M., Jager, H. R., & Barkhof, F. (2018). Cerebral Microbleeds: Imaging and clinical significance. Radiology, 287(1), 11–28.
Helmes, E. (2000). Learning and memory. In G. Groth, & Marnat (Eds.), Neuropsychological assessment in clinical practice: A guide to test interpretation and integration (pp. 293–334). John Wiley & Sons, Inc.
Huang, Y. L., Kuo, Y. S., Tseng, Y. C., Chen, D. Y., Chiu, W. T., & Chen, C. J. (2015). Susceptibility-weighted MRI in mild traumatic brain injury. Neurology, 84(6), 580–585.
Irimia, A., Ngo, V., Chaudhari, N. N., Zhang, F., Joshi, S. H., Penkova, A. N., O’Donnell, L. J., Sheikh-Bahaei, N., Zheng, X., & Chui, H. C. (2022). White matter degradation near cerebral microbleeds is associated with cognitive change after mild traumatic brain injury. Neurobiology of aging, 120, 68–80.
Iverson, G. L., & Tulsky, D. S. (2003). Detecting malingering on the WAIS-III. Unusual digit span performance patterns in the normal population and in clinical groups. Archives of clinical neuropsychology: the official journal of the National Academy of Neuropsychologists, 18(1), 1–9.
King, N. S., Crawford, S., Wenden, F. J., Moss, N. E., & Wade, D. T. (1995). The Rivermead Post concussion symptoms Questionnaire: A measure of symptoms commonly experienced after head injury and its reliability. Journal Of Neurology, 242(9), 587–592.
Laborey, M., Masson, F., Ribereau-Gayon, R., Zongo, D., Salmi, L. R., & Lagarde, E. (2014). Specificity of postconcussion symptoms at 3 months after mild traumatic brain injury: Results from a comparative cohort study. The Journal Of Head Trauma Rehabilitation, 29(1), E28–36.
Lange, R. T., Iverson, G. L., & Rose, A. (2011). Depression strongly influences postconcussion symptom reporting following mild traumatic brain injury. The Journal Of Head Trauma Rehabilitation, 26(2), 127–137.
Lezak, M. D. (1995). Neuropsychological assessment (Third ed.). Oxford University Press.
Massey, J. S., Meares, S., Batchelor, J., & Bryant, R. A. (2015). An exploratory study of the association of acute posttraumatic stress, depression, and pain to cognitive functioning in mild traumatic brain injury. Neuropsychology, 29(4), 530–542.
McCauley, S. R., Wilde, E. A., Barnes, A., Hanten, G., Hunter, J. V., Levin, H. S., & Smith, D. H. (2014). Patterns of early emotional and neuropsychological sequelae after mild traumatic brain injury. Journal Of Neurotrauma, 31(10), 914–925.
McKinney, A. M., Sarikaya, B., Gustafson, C., & Truwit, C. L. (2012). Detection of microhemorrhage in posterior reversible encephalopathy syndrome using susceptibility-weighted imaging. Ajnr. American Journal Of Neuroradiology, 33(5), 896–903.
Nandigam, R. N., Viswanathan, A., Delgado, P., Skehan, M. E., Smith, E. E., Rosand, J., Greenberg, S. M., & Dickerson, B. C. (2009). MR imaging detection of cerebral microbleeds: Effect of susceptibility-weighted imaging, section thickness, and field strength. Ajnr. American Journal Of Neuroradiology, 30(2), 338–343.
Park, J. H., Park, S. W., Kang, S. H., Nam, T. K., Min, B. K., & Hwang, S. N. (2009). Detection of traumatic cerebral microbleeds by susceptibility-weighted image of MRI. Journal Of Korean Neurosurgical Society, 46(4), 365–369.
Ponsford, J. (2013). Factors contributing to outcome following traumatic brain injury. Neurorehabilitation, 32(4), 803–815.
Ponsford, J., Olver, J., Ponsford, M., & Nelms, R. (2003). Long-term adjustment of families following traumatic brain injury where comprehensive rehabilitation has been provided. Brain Inj, 17(6), 453–468.
Robles, D. J., Dharani, A., Rostowsky, K. A., Chaudhari, N. N., Ngo, V., Zhang, F., O’Donnell, L. J., Green, L., Sheikh-Bahaei, N., Chui, H. C., & Irimia, A. (2022). Older age, male sex, and cerebral microbleeds predict white matter loss after traumatic brain injury. Geroscience, 44(1), 83–102.
Rush, A. J., Gullion, C. M., Basco, M. R., Jarrett, R. B., & Trivedi, M. H. (1996). The Inventory of Depressive Symptomatology (IDS): Psychometric properties. Psychological Medicine, 26(3), 477–486.
Salthouse, T. A. (2009). When does age-related cognitive decline begin? [Research Support, N.I.H., Extramural]. Neurobiology of aging, 30(4), 507–514.
Schmidt, M. (1996). Rey Auditory-Verbal Learning Test. Western Psychological Services.
Schoenberg, M. R., Dawson, K. A., Duff, K., Patton, D., Scott, J. G., & Adams, R. L. (2006). Test performance and classification statistics for the Rey Auditory Verbal Learning Test in selected clinical samples. Archives of clinical neuropsychology: the official journal of the National Academy of Neuropsychologists, 21(7), 693–703.
Schutte, C., & Axelrod, B. N. (2013). Use of embedded cognitive symptom validity measures in mild traumatic brain injury cases. In D. A. Carone, & S. S. Bush (Eds.), Mild traumatic brain injury: Symptom validity assessment and malingering (pp. 159–181). Springer Publishing Company.
Silva, P. H. R., Spedo, C. T., Baldassarini, C. R., Benini, C. D., Ferreira, D. A., Barreira, A. A., & Leoni, R. F. (2019). Brain functional and effective connectivity underlying the information processing speed assessed by the Symbol Digit Modalities Test. Neuroimage, 184, 761–770.
Silver, J. M. (2014). Neuropsychiatry of persistent symptoms after concussion. Psychiatric Clinics Of North America, 37(1), 91–102.
Snell, D. L., Surgenor, L. J., Hay-Smith, E. J., Williman, J., & Siegert, R. J. (2015). The contribution of psychological factors to recovery after mild traumatic brain injury: Is cluster analysis a useful approach? Brain Inj, 29(3), 291–299.
Spreen, O., & Strauss, E. (1998). A compendium of neuropsychological tests: Administration, norms, and commentary (2nd ed.). Oxford University Press.
Stern, Y. (2002). What is cognitive reserve? Theory and research application of the reserve concept. Journal Of The International Neuropsychological Society, 8(3), 448–460.
Steward, K. A., Novack, T. A., Kennedy, R., Crowe, M., Marson, D. C., & Triebel, K. L. (2017). The Wechsler Test of Adult Reading as a measure of Premorbid Intelligence following traumatic Brain Injury. Archives of clinical neuropsychology: the official journal of the National Academy of Neuropsychologists, 32(1), 98–103.
Studerus-Germann, A. M., Gautschi, O. P., Bontempi, P., Thiran, J. P., Daducci, A., Romascano, D., von Ow, D., Hildebrandt, G., von Hessling, A., & Engel, D. C. (2018). Central nervous system microbleeds in the acute phase are associated with structural integrity by DTI one year after mild traumatic brain injury: A longitudinal study. Case Report Neurologia I Neurochirurgia Polska, 52(6), 710–719.
Stulemeijer, M., van der Werf, S., Borm, G. F., & Vos, P. E. (2008). Early prediction of favourable recovery 6 months after mild traumatic brain injury. Journal Of Neurology, Neurosurgery And Psychiatry, 79(8), 936–942.
Tate, D. F., Gusman, M., Kini, J., Reid, M., Velez, C. S., Drennon, A. M., Cooper, D. B., Kennedy, J. E., Bowles, A. O., Bigler, E. D., Lewis, J. D., Ritter, J., & York, G. E. (2017). Susceptibility weighted imaging and White Matter Abnormality Findings in Service Members with Persistent cognitive symptoms following mild traumatic brain Injury. Military Medicine, 182(3), e1651–e1658.
Terry, D. P., Brassil, M., Iverson, G. L., Panenka, W. J., & Silverberg, N. D. (2019). Effect of depression on cognition after mild traumatic brain injury in adults. The Clinical Neuropsychologist, 33(1), 124–136.
Tong, K. A., Ashwal, S., Holshouser, B. A., Shutter, L. A., Herigault, G., Haacke, E. M., & Kido, D. K. (2003). Hemorrhagic shearing lesions in children and adolescents with posttraumatic diffuse axonal injury: Improved detection and initial results. Radiology, 227(2), 332–339.
Trifan, G., Gattu, R., Haacke, E. M., Kou, Z., & Benson, R. R. (2017). MR imaging findings in mild traumatic brain injury with persistent neurological impairment. Magnetic Resonance Imaging, 37, 243–251.
van der Horn, H. J., de Haan, S., Spikman, J. M., de Groot, J. C., & van der Naalt, J. (2018). Clinical relevance of microhemorrhagic lesions in subacute mild traumatic brain injury. Brain Imaging Behav, 12, 912–916.
Vernooij, M. W., van der Lugt, A., Ikram, M. A., Wielopolski, P. A., Niessen, W. J., Hofman, A., Krestin, G. P., & Breteler, M. M. (2008). Prevalence and risk factors of cerebral microbleeds: The Rotterdam scan study. Neurology, 70(14), 1208–1214.
Voss, J. D., Connolly, J., Schwab, K. A., & Scher, A. I. (2015). Update on the epidemiology of Concussion/Mild traumatic brain Injury. Current Pain And Headache Reports, 19(7), 32.
Wang, X., Wei, X. E., Li, M. H., Li, W. B., Zhou, Y. J., Zhang, B., & Li, Y. H. (2014). Microbleeds on susceptibility-weighted MRI in depressive and non-depressive patients after mild traumatic brain injury. Neurological Sciences : Official Journal Of The Italian Neurological Society And Of The Italian Society Of Clinical Neurophysiology, 35(10), 1533–1539.
Wechsler, D. (2001). The Wechsler Test of Adult Reading. The Psychological Corporation.
Wechsler, D. (2008). Wechsler Adult Intelligence Scale - Fourth Edition. The Psychological Corporation.
Wilde, E. A., Whiteneck, G. G., Bogner, J., Bushnik, T., Cifu, D. X., Dikmen, S., French, L., Giacino, J. T., Hart, T., Malec, J. F., Millis, S. R., Novack, T. A., Sherer, M., Tulsky, D. S., Vanderploeg, R. D., & von Steinbuechel, N. (2010). Recommendations for the use of common outcome measures in traumatic brain injury research. Archives Of Physical Medicine And Rehabilitation, 91(11), 1650–1660e1617.
Acknowledgements
The authors would like to acknowledge the contribution of post-graduate students and research assistants: Georgia Bolt, Emily Cockle, Nicolette Ingram, Courtney Lewis, Katie Priestley, Joshua Nash, Aimee Savage, Nicola Singleton and Patrick Summerell for their assistance in collecting this data.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This work was supported by The University of Melbourne [2017 MRGSS]. Imaging analysis was conducted within the Developmental Imaging research group, Murdoch Children’s Research Institute at the Children’s MRI Centre, Royal Children’s Hospital, Melbourne Victoria. This was supported by the Murdoch Children’s Research Institute, Royal Children’s Hospital, The University of Melbourne Department of Paediatrics and the Victorian Government’s Operational Infrastructure Support Program. This work was also part funded by a grant from The University of Melbourne, and the Royal Children’s Hospital Foundation (RCH1000 and RCH 2022-1402). Dr JYMY receives position funds from the Royal Children’s Hospital Foundation (RCH1000 and RCHF 2022 − 1402).
Author information
Authors and Affiliations
Contributions
Author contributions included conception and study design (J.A; L.H; M.S., J.Y), data collection or acquisition (L.H; M.W; J.Y), statistical analysis (J.A; L.H), interpretation of results (J.A; L.H; M.S., J.Y), drafting the manuscript work or revising it critically for important intellectual content (J.A; L.H; M.S., J.Y) and approval of final version to be published and agreement to be accountable for the integrity and accuracy of all aspects of the work (All authors).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflicts of interest/Competing interest
No conflicts of interest were declared by any author.
Ethics approval
The project was approved by The Alfred hospital and Royal Melbourne Hospital Human Research Ethics Committees.
Consent to participate
All participants provided informed consent.
Consent for publication
All participants provided informed consent to publish the data.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Anderson, J.F., Higson, L., Wu, M.H. et al. Cerebral microhaemorrhage count is related to processing speed, but not level of symptom reporting, independently of age, psychological status and premorbid functioning, after first-ever mild traumatic brain injury. Brain Imaging and Behavior 17, 608–618 (2023). https://doi.org/10.1007/s11682-023-00788-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-023-00788-0