Abstract
Summary
We used cluster analysis to determine the profiles of individuals who sustained wrist fractures. We found two groups: (1) young and active and (2) older and less active. This information may be used to identify individuals who require further bone health interventions to optimize healthy aging.
Introduction
Distal radial fractures (DRF) are the most common of all fractures, with 6% of males and 33% of females having one at some point in their lifetime. We hypothesize that DRF consists of two subpopulations: one with compromised bone health that is early in the osteoporosis (OP) trajectory and another which are active and healthy and suffer a misfortune fracture due to their high activity levels or risk-taking behaviors. The latter is likely to recover with a minimal disability, while the former may signal a negative health trajectory of disability and early mortality.
Objective
To determine the profiles of individuals who sustained wrist fractures using cluster analysis within the Comprehensive Cohort of the Canadian Longitudinal Study on Aging (CLSA) database considering factors that reflect bone health and activity levels.
Methods
We included all the individuals who had a wrist fracture within the CLSA comprehensive cohort of the database (n = 968). The baseline data was used for this analysis. A 2-step cluster analysis was used to identify profiles that were both statistically and clinically meaningful. Variables that were used in the cluster analysis include demographic variables, physical activity status indicators, general health indicators, mobility indicators, bone health indicators, comorbid conditions, and lifestyle factors.
Results
We were able to identify two distinct profiles that were statistically and clinically meaningful confirming our hypothesis. One cluster included a predominantly younger cohort, who are physically active, with less comorbid conditions, better bone health, and better general health, while the opposite was true of the first cohort.
Conclusion
We were able to identify two clusters—a healthy profile and a bone health compromised profile. This information may be used to identify the subgroup of people who should be targeted in the future for more intensive preventive health services to optimize healthy aging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distal radius fractures (DRF) are the most common of all fractures [1,2,3,4], with 6% of males and 33% of females [5, 6] sustaining one within their lifetime. About 40% of osteoporotic fractures in women between the ages of 50 and 60 years are DRF [7]. The incidence of DRF in men is lower and spikes later in life [7]. Upper extremity fractures can occur because of compromised bone health, or in healthy people due to misfortune. DRF is generally classified as fragility fractures when they occur due to low trauma such as a fall from a standing height. However, this is a gross generalization that does not precisely differentiate those with compromised bone health from those who have suffered misfortune.
Since DRF occurs early in the potential trajectory of osteoporosis (OP), clinical information such as bone mineral density (BMD) testing is rarely available to assist with early decision-making. Furthermore, a meta-analysis of 90,000 person-years and over 2000 fractures indicated that there is a wide overlap in the BMD of patients who develop a fracture and those who do not [8]. One Canadian population-based study of over 260,000 1st incident upper extremity fractures identified that DRF was the most frequent fracture and occurs most commonly in women in the 50–65-year-old age group. Another Canadian population-based study identified the 10-year probability of a secondary fracture after an initial DRF (14%) is elevated compared to the 10% population risk but was a lower risk indicator than the 24% rate that occurred for proximal humerus fractures (PHF) [9]. This suggests that PHF is a more definite fragility fracture than DRF. Current systems for establishing future fracture risk provide substantially different risk estimates, especially for people under 65 years of age [9]. However, what is clear across studies is that BMD alone is insufficient to characterize bone health or the risks of fracture.
Upper extremity fragility fractures occur sufficiently in advance of more osteoporotic fractures affecting the spine and larger bones, such that intensive early interventions to improve bone health along with proper nutrition and exercise are likely to have a positive impact on future bone health. Furthermore, early risk identification is a focus in current osteoporosis (OP) clinical practice guidelines [10]. Targeting secondary prevention to those at risk may prevent the severe disability and early mortality [11] that results from osteoporotic spinal and hip fractures [10]. We hypothesize that DRF consists of two subpopulations: one with compromised bone health that is early in an OP trajectory and another which consists of individuals who are active and healthy but suffer a misfortune fracture due to their lifestyle behaviors. The latter is likely to recover with minimal disability [12, 13], while the former may signal a negative health trajectory of disability and early mortality [14]. Some epidemiological data support our hypothesis of different profiles with different fracture populations since DRF occurs in more active people and is more related to weather and activity [15].
In Canada, OP costs about $2 billion/year, and those costs double if the proportion of those placed in long-term care as a result of OP is taken into consideration [16]. Previous research suggests that in older adults who sustain a fragility fracture, future healthcare costs increase exponentially post-fracture [16, 17, 17, 18]. The majority of the costs of managing OP relate to managing the incident costs of the fractures, suggesting that secondary fracture prevention is critical [16, 19]. However, given the high incidence of DRF and moderate risks, broad-scale prevention strategies that are not appropriately targeted will not be cost-effective or feasible. In addition, practice pattern analysis indicates that therapists [20] and orthopedic surgeons [21] rarely initiate early conservative bone health interventions following a DRF. Clinical indicators that could be used to appropriately target this for early intervention to a smaller subset of patients might be cost-effective and feasible for implementation.
The purpose of this study is to determine the profiles of individuals with compromised bone health and unfortunate wrist fractures using cluster analysis within the Canadian Longitudinal Study on Aging (CLSA) database.
Methods
Participants
Both men and women (N = 968) aged 45 and older who have had a wrist fracture and enrolled in the Comprehensive Cohort of the Canadian Longitudinal Study of Aging (CLSA) (https://www.clsa-elcv.ca/) were included in the study. The CLSA is a large long-term (20 years) national longitudinal study conducted to identify ways to help people live longer and live well and to better understand healthy aging [22, 23]. CLSA is a strategic initiative of the Canadian Institutes of Health Research (CIHR). The CLSA comprises 51,338 participants who were aged between 45 and 85 years when recruited (2010 and 2015). They will be followed up until 2033 or death whichever is earlier. Out of the 51,338 participants, 31,097 participants (comprehensive cohort) underwent in-home interviews and in-person comprehensive assessments at the data collection centers. More in-depth information can be found on the CLSA website (https://www.clsa-elcv.ca/). The baseline data from the Comprehensive Cohort was used in this study. Demographic characteristics of the wrist fracture cohort are included in Table 1.
Variables used in this study
We view health as an interaction between body structure, impairments, activity, and participation; modified by personal and environmental factors;22 consistent with how health and functioning are defined by the World Health Organization (WHO) International Classification of Functioning (ICF) [24]. The following variables were used in the cluster analysis:
Demographic variables:
age, gender, and age group [25]
Biological variables:
body mass index, total body fat percentage, DEXA bone scan bone mineral density (BMD) hip, and average grip strength
Physical activity and mobility indicators
average balance, Timed Up and Go test, and following questions from the Physical Activities (PA2) [26]. Questionnaire was used to indicate physical activity levels:
-
a.
Light sports, or recreation activities in the past 7 days (in days)
-
b.
Moderate sports, or recreation activities in the past 7 days (in days)
-
c.
Strenuous sports, or recreation activities in the past 7 days (in days)
-
d.
Strength and endurance exercise in the past 7 days (in days)
-
e.
Walking in the past 7 days (in days)
-
f.
Sitting activities in the past 7 days (in days)
-
g.
Past 7 days, light housework (yes/no)
-
h.
Past 7 days, heavy housework (yes/no)
-
i.
Past 7 days, caring for others (yes/no)
General health indicators
Number of falls in the past 12 months, self-rated general health, self-rated vision, grouped musculoskeletal (MSK) comorbid conditions, osteoporosis diagnosis, menopause [25]
Lifestyle factors
calcium supplement use, vitamin D supplement use, hormone replacement therapy (HRT), smoking [25].
Statistical analysis
Data preparation
All analyses were completed using SPSS version 27(SPSS Inc., Chicago, IL). Missing data were handled using multiple imputations [27]. Missing data patterns were analyzed before completing imputations. In the baseline dataset, 23.81% of the cases had missing values and on the whole 2.7% of the data were missing. All variables except for one had missing values. Missing value pattern analysis indicated that there was no specific pattern.
Cluster analysis
We completed a 2-step cluster analysis of sex-stratified wrist fracture participants. We stratified by sex as we did not want the clustering to be driven by the underlying differences between the two sexes in many variables that were included in the model like body mass index (BMI), total body fat percentage, DEXA bone scan BMD hip, and average grip strength. Effectively, we completed two different 2-step cluster analyses for the following groups: (1) women who have sustained a wrist fracture and (2) men who have sustained a wrist fracture. We used the 2-step cluster analysis approach as it efficiently handles continuous and categorical variables [28]. The following variables were used in the cluster analysis: age, DEXA total body fat percentage, DEXA bone scan neck of femur T score, DEXA bone scan whole body T score, maximum grip strength, balance scores, and Timed Up and Go (TUG) test. The statistical analysis runs a pre-clustering in the first step to identify groupings and in the second step, it runs a hierarchical clustering method that automatically selects the number of clusters. For the second step, the program utilizes the Bayesian information criterion (BIC) to select the “best” cluster solution. A smaller BIC value indicates a better-fitting model. The 2-step cluster analysis uses a distance measure that defines the distance between two clusters as the corresponding decrease in log-likelihood by combining them into one cluster [29, 30]. It can handle large datasets with ease because of the pre-clustering completed in the first step.
Results
Sample characteristics
Women comprised over two-thirds of the participants (70.5%). The mean age was 67.5 years SD 9.72 with a range from 45 to 84 years. About 28.5% and 13.9% of the participants were diagnosed with osteopenia and osteoporosis, respectively. Two-thirds of the participants (66.9%) were either obese or overweight. Most participants (89.2%) rated their general health as good or excellent. Forty-three percent of the participants had an osteoarthritis diagnosis. The majority of participants rated themselves as active on the physical activity self-report questions (see Table 1 for details).
Cluster analysis
For both sexes, a two-step cluster analysis identified 2 distinct clusters with homogenous patterns of the variables that were included in the model. We named the first cluster as younger and active while the second cluster was named older and less active.
Wrist fracture group (female) (seeTables 2, 3, and 4)
Younger and active cluster (n = 246, 46.9%)
They were relatively younger with a mean age of 63.1 years when compared to the older and less active cluster (mean age of 73.13 years). The majority fell within the 45 to 64 age group (66%). Most had gone through menopause (87%). Thirty-seven percent of them were treated with hormone replacement therapy (HRT). These participants had better T scores when compared to the older and less active cluster (femoral neck—mean − 1.35; SD 1.06 and whole body—mean − 0.97; SD 1.37). The majority (59%) were either obese or overweight. They reported that they have very good or excellent general health (70%) and vision (66%). Most were either non-smokers (51%) or former smokers (43%). They reported a relatively high level of physical activity when compared to the other cluster. Almost half of them reported taking part in strenuous sports activities (40%); almost everyone walked in the last week (87%); close to three-quarters reported doing heavy housework (73%); and 46% did some yard work. This cluster faired well in the physical performance tests when compared to the other cluster. They had higher grip strength (mean 27.33 kg; SD 4.98); higher balance scores (mean 48.20 s; SD 17.36); a lower TUG time (mean 8.74 s; SD 1.19); and a lower chair rise test time (mean 12.94 s; SD 3.21).
Older and less active cluster (n = 279, 53.1%)
This group was relatively older with a mean age of 73.13 years (SD 7.11) when compared to the younger and active cluster. The majority fell within the 65 and older age group (87%). Most had gone through menopause (96%). Fifty-one percent were treated with HRT. They had lower T scores when compared to the other cluster (femoral neck—mean − 1.82; SD 0.84 and whole body—mean − 1.62; SD 1.30) and forty-four percent were osteoporotic. More than two-thirds of the participants were either obese or overweight. More than half of them reported that they have very good or excellent general health (56%) and vision (50%). Most of them were either non-smokers (52%) or former smokers (43%). They reported relatively lower levels of physical activity when compared to the other cluster. Almost one-quarter of them reported taking part in strenuous sports activities (23%); three-quarters reported that they walked in the last week (77%); 59% did heavy housework; and 30% did some yard work. This cluster performed poorly in the physical performance tests when compared to the other cluster. They had lower grip strength (mean 23.13 kg; SD 5.11); lower balance scores (mean 9.17 s; SD 9.52); a higher TUG time (mean 10.51 s; SD 2.06); and a higher chair rise test time (mean 14.99 s; SD 3.84).
Wrist fracture group (male) (seeTables 2, 3, and 4)
Younger and more active cluster (n = 112, 46.5%)
They were relatively younger with a mean age of 59.72 years (SD 8.76) when compared to the other cluster. The majority fell within the 45 to 64 age group (74%). They had better T scores when compared to the younger and active cluster (femoral neck—mean − 0.41; SD 1.14 and whole body—mean 0.73; SD 1.34). Only 4% were osteoporotic. Seventy percent of them were either obese or overweight. Most reported that they had very good or excellent general health (74%) and vision (69%). Most of them were either non-smokers (50%) or former smokers (41%). They reported a relatively high level of physical activity when compared to the other cluster. Almost half of them reported taking part in strenuous sports activities (48%); almost everyone walked in the last week (89%); close to three-quarters reported doing heavy housework (71%); and 64% did some yard work. This cluster faired well in the physical performance tests when compared to the older and less active cluster. They had higher grip strength (mean 48.16 kg; SD 7.62); higher balance scores (mean 53.59 s; SD 13.32); a lower TUG time (mean 8.65 s; SD 1.22); and a lower chair rise test time (mean 12.13 s; SD 3.19).
Older and less active cluster (n = 129, 53.5%)
They were relatively older with a mean age of 69.21 years (SD 8.13) when compared to the other cluster. Most of them fell within the 65 and older age group (69%). They had lower T scores when compared to the younger and active cluster (femoral neck—mean − 0.89; SD 1.01 and whole body—mean 0.25; SD 1.40). Eleven percent were osteoporotic. More than three-quarters of them were either obese or overweight. More than half of them reported that they have very good or excellent general health (57%) and vision (61%). Most of them were either non-smokers (35%) or former smokers (54%). They reported relatively lower levels of physical activity when compared to the other cluster. More than a quarter of them reported taking part in strenuous sports activities (28%); 88% reported that they walked in the last week; 54% did heavy housework; and 54% did some yard work. This cluster performed poorly in the physical performance tests when compared to the other cluster. They had relatively lower grip strength (mean 37.72 kg; SD 8.05); lower balance scores (mean 15.49 s; SD 17.51); a higher TUG time (mean 10.19 s; SD 1.79); and a higher chair rise test time (mean 14.46 s; SD 3.91).
Discussion
The results of the current study support our hypothesis that within those who sustain distal wrist fractures, there are two distinct groups of individuals. One group is characterized by older individuals with lower BMD and lower physical activity levels. This is consistent with age-related changes exacerbated by inactivity and poor nutrition [31] that may result in compromised bone health and true fragility fractures. The other cluster is characterized by younger individuals, with normal bone mineral density and higher physical activity levels; in this group, fractures are more likely attributable to misfortunate while engaged in physical activity. These separate subgroups explain why DRF is less predictive of future fractures than PHF [32] which occurs in an older more fragile population. This study suggests that DRF has subtypes of fragility fracture and misfortunate fracture. This has clinical relevance since these subgroups have different risk trajectories and may have different expectations for functional recovery.
Frailty is an important medical and public health problem [33] that can result in an increased burden on the healthcare system in terms of utilization and cost [34, 35]. Frailty comprises a combination of clinical and physiological changes in the human body as individuals grow older. In the current study, the older and less active cluster with distal wrist fracture was characterized by the presence of decreased grip strength, longer time duration to complete the chair rise test, and lower physical activity. These characteristics match the phenotype for frailty proposed by previous studies [33, 36,37,38]. Since the incidence of a DRF is not a stand-alone indicator of frailty, these cluster characteristics must be considered. However, a DRF should act as a positive screening test, indicating the need to assess frailty parameters and identify aspects that can be remediated.
The older and compromised bone health cluster should be the target group for interventions related to bone health, such as fall prevention strategies and exercise-based programs aimed at increased strength, balance, and endurance. A study where post-menopausal women were followed up for more than 11 years concluded that a wrist fracture is associated with increased risk of the subsequent hip (HR = 1.36, 95% CI 1.26–1.48), spine (HR = 1.48, 95% CI 1.32–1.66), upper extremity (HR = 1.88, 95% CI 1.70–2.07), and lower extremity fractures (HR = 1.36, 95% CI 1.26–1.48) [39]. If these interventions are not applied at the right time, it can be considered as a missed opportunity to contain a cascade of fractures that are non-wrist related [20]. However, previous research described below indicates that these interventions are less often initiated with wrist fractures. A retrospective nationwide cohort study in Korea concluded that wrist fracture patients were less often evaluated and treated for osteoporosis by their treating physician managing the fracture when compared to hip or spine fractures [40]. A Canadian study indicated that only 50% of those with a wrist fracture were followed up for osteoporosis evaluation and management post-fracture [41]. Patients presenting with wrist fractures with the characteristics described in this study must be screened for osteoporosis and utilize this as a window of opportunity to put in place targeted interventions to prevent further fractures and resulting frailty and disability [11].
A previous study demonstrated younger patients with DRF are at greater risk of poor outcomes in terms of pain and functional disability when malalignment of the fracture is present, compared to older patients [42]. This is presumed to be related to life demands, a concept that is supported in our cluster findings. However, studies also suggest that the younger active cohort might recover faster than the older adult group [43]. Young women with a wrist fracture are more prone to subsequent non-wrist fractures [39]. In addition, the management of wrist fractures in this group differs from the elderly frail group [44]. However, clinical practice guidelines [45, 46] recommend a bone mineral density test in the following cases: in all women over 65 and men over 70 years of age; individuals who break a bone after age 50; a woman of menopausal age with risk factors; and postmenopausal woman under age 65 with risk factors. This recommendation unfortunately does not address women less than 50 years of age who sustain a wrist fracture. This might affect the prospects of this cohort of women obtaining a BMD scan, which can potentially help prevent secondary fractures.
The younger and active group reported higher engagement in moderate to strenuous activities suggesting that to a certain extent, the fracture risk may have been related to activities, environmental hazards, and risk-taking. Secondary fracture prevention for this group might focus on fall hazard reduction and activity analysis. Since the younger more active cohort fracture profiles were less representative of fragility fractures, we hypothesize they may have occurred with high-energy trauma and may require more specialized fracture management to optimize anatomic reduction and allow individuals to return to their previously active lifestyle.
Our study showed that individuals who were in the older and less active group also had relatively lower levels of bone mineral density and higher rates of osteoporosis diagnosis. A previous study has found that a decrease of 1 SD of the femoral neck BMD was associated with a 66% higher relative risk of wrist fracture [47]. In addition, we also found that there was a greater incidence of osteoporosis and lower BMD in women than in men in both groups. These study findings are in line with previous estimates [48,49,50,51] that indicate a strong female predominance among those incurring a DRF, especially after the age of 50.
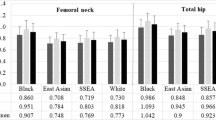
The balance score was the main indicator in differentiating the clusters in the 2-step cluster analysis in the current study. This did not come as a surprise as previous studies have confirmed that balance levels decline in individuals as they age [52, 53]. A review completed to look into the changes in gait and balance associated with aging found that older adults showed an age-related decrease in balance and increased gait variability with associated risk for falls [53]. This may explain why this factor turned out to be the significant factor in differentiating the clusters. Another significant indicator was grip strength. Grip strength as an indicator of general health [54] has been previously shown that the unaffected side grip strength can predict fracture risk in the 4 years after a DRF in a prospective cohort study [55]. Another study has concluded that the grip strength of the unaffected side can act as a surrogate for general bone health, frailty, and overall muscle strength [20]. We found stark differences in both the balance scores and grip strength between the two clusters (Figs. 1 and 2). The older less active cluster demonstrated poorer balance and grip strength. This is in line with previous studies. A case–control study identified that older adults with distal radius fractures (DRF) had poorer balance [56]. In another case–control study, women with DRF had poorer dynamic balance and grip strength [57]. Studies have indicated that exercise intervention focussed on strength and balance is effective for fracture prevention in the elderly [58, 59]. However, the implementation rate of these interventions is very low [56].
The strengths of the current study include the use of data from a large population-based database that was randomly sampled. This has helped us to study the profiles of people from different geographical regions and social strata in Canada. This increases the power and generalizability of our findings. Our study also had some limitations. A limitation common to all CLSA studies is that this large population study may reflect a healthier volunteer cohort rather than the true population norms. This could be because participation in the current study would have been more difficult for those with mobility, health, or transportation issues since it required in-person testing. Another limitation is that the information about fracture is limited to self-reported, is not time-indexed, and we have limited information on the nature of the fracture or its management.
In conclusion, this study was able to identify two distinct clusters with profiles of people who sustain a wrist fracture—an older less active cluster and a younger active group. Screening procedures and secondary prevention interventions should be tailored to these different risk profiles with the type and weighting of hazard awareness, balance training, and strength training.
Data availability
Data are available from the Canadian Longitudinal Study on Aging (www.clsa-elcv.ca) for researchers who meet the criteria for access to de-identified CLSA data.
References
Baron JA, Karagas M, Barrett J et al (1996) Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiol Camb Mass 7:612–618
Karl JW, Olson PR, Rosenwasser MP (2015) The epidemiology of upper extremity fractures in the United States, 2009. J Orthop Trauma 29:e242-244
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37:691–697
MacIntyre NJ, Dewan N (2016) Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther Off J Am Soc Hand Ther 29:136–145
Bonafede M, Espindle D, Bower AG (2013) The direct and indirect costs of long bone fractures in a working age US population. J Med Econ 16:169–178
Ahmed LA, Schirmer H, Bjørnerem A et al (2009) The gender- and age-specific 10-year and lifetime absolute fracture risk in Tromsø. Norway Eur J Epidemiol 24:441–448
Kanas M, Faria RS, Salles LG et al (1992) Home-based exercise therapy for treating non-specific chronic low back pain. Rev Assoc Medica Bras 2018(64):824–831
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312:1254–1259
Beattie PF, Silfies SP (2015) Improving long-term outcomes for chronic low back pain: time for a new paradigm? J Orthop Sports Phys Ther 45:236–239
Papaioannou A, Morin S, Cheung AM et al (2010) 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ Can Med Assoc J J Assoc Medicale Can 182:1864–1873
Ioannidis G, Papaioannou A, Hopman WM et al (2009) Relation between fractures and mortality: results from the Canadian Multicentre Osteoporosis Study. CMAJ Can Med Assoc J J Assoc Medicale Can 181:265–271
MacDermid JC, Donner A, Richards RS et al (2002) Patient versus injury factors as predictors of pain and disability six months after a distal radius fracture. J Clin Epidemiol 55:849–854
MacDermid JC, Roth JH, Richards RS (2003) Pain and disability reported in the year following a distal radius fracture: a cohort study. BMC Musculoskelet Disord 4:24
Rozental TD, Branas CC, Bozentka DJ et al (2002) Survival among elderly patients after fractures of the distal radius. J Hand Surg 27:948–952
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet Lond Engl 359:1761–1767
Hopkins RB, Burke N, Von Keyserlingk C et al (2016) The current economic burden of illness of osteoporosis in Canada. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 27:3023–3032
Nikitovic M, Wodchis WP, Krahn MD et al (2013) Direct health-care costs attributed to hip fractures among seniors: a matched cohort study. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 24:659–669
Leslie WD, Lix LM, Finlayson GS et al (2013) Direct healthcare costs for 5 years post-fracture in Canada: a long-term population-based assessment. Osteoporos Int 24:1697–1705
Hernlund E, Svedbom A, Ivergård M et al (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136
Dewan N, MacDermid JC, MacIntyre NJ et al (2019) Therapist’s practice patterns for subsequent fall/osteoporotic fracture prevention for patients with a distal radius fracture. J Hand Ther Off J Am Soc Hand Ther 32:497–506
Dreinhöfer KE, Anderson M, Féron J-M et al (2005) Multinational survey of osteoporotic fracture management. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 16(Suppl 2):S44-53
Raina PS, Wolfson C, Kirkland SA et al (2009) The Canadian Longitudinal Study on Aging (CLSA). Can J Aging Rev Can Vieil 28:221–229
Raina P, Wolfson C, Kirkland S et al (2019) Cohort profile: the Canadian Longitudinal Study on Aging (CLSA). Int J Epidemiol 48:1752–1753j
Rauch A, Cieza A, Stucki G (2008) How to apply the International Classification of Functioning, Disability and Health (ICF) for rehabilitation management in clinical practice. Eur J Phys Rehabil Med 44:329–342
Canadian Longitudinal Study on Aging (2018) 60-min. questionnaire (tracking main wave) v4.0 (baseline). Available at: https://www.clsa-elcv.ca/doc/446
Canadian Longitudinal Study on Aging (2015) Physical Activity Scale for the Elderly (PASE) (baseline) adapted from New England Research Institutes (NERI). Maintain Contact (Tracking and Comprehensive) 2(7):30–41. Availble at: https://www.clsa-elcv.ca/doc/540
He Y, Zaslavsky AM, Landrum MB et al (2010) Multiple imputation in a large-scale complex survey: a practical guide. Stat Methods Med Res 19:653–670
Meilă M, Heckerman D (2001) An experimental comparison of model-based clustering methods. Mach Learn 42:9–29
Zhang T, Ramakrishnan R, Livny M (1996) BIRCH: an efficient data clustering method for very large databases. ACM Sigmod Rec 25:103–114
Banfield JD, Raftery AE (1993) Model-based Gaussian and non-Gaussian clustering. Biometrics 49:803–821
Hickson M (2006) Malnutrition and ageing. Postgrad Med J 82:2–8
Hodsman AB, Leslie WD, Tsang JF et al (2008) 10-year probability of recurrent fractures following wrist and other osteoporotic fractures in a large clinical cohort: an analysis from the Manitoba Bone Density Program. Arch Intern Med 168:2261–2267
Rockwood K, Andrew M, Mitnitski A (2007) A comparison of two approaches to measuring frailty in elderly people. J Gerontol A Biol Sci Med Sci 62:738–743
Mondor L, Maxwell CJ, Hogan DB et al (2019) The incremental health care costs of frailty among home care recipients with and without dementia in Ontario, Canada: a cohort study. Med Care 57:512–520
Hajek A, Bock J-O, Saum K-U et al (2018) Frailty and healthcare costs-longitudinal results of a prospective cohort study. Age Ageing 47:233–241
Fried LP, Tangen CM, Walston J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146-156
Bandeen-Roche K, Xue Q-L, Ferrucci L et al (2006) Phenotype of frailty: characterization in the women’s health and aging studies. J Gerontol A Biol Sci Med Sci 61:262–266
Ensrud KE, Ewing SK, Taylor BC et al (2008) Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med 168:382–389
Crandall CJ, Hovey KM, Cauley JA et al (2015) Wrist fracture and risk of subsequent fracture: findings from the Women’s Health Initiative study. J Bone Miner Res Off J Am Soc Bone Miner Res 30:2086–2095
Gong HS, Oh WS, Chung MS et al (2009) Patients with wrist fractures are less likely to be evaluated and managed for osteoporosis. J Bone Joint Surg Am 91:2376–2380
Khan SA, de Geus C, Holroyd B et al (2001) Osteoporosis follow-up after wrist fractures following minor trauma. Arch Intern Med 161:1309–1312
Grewal R, MacDermid JC (2007) The risk of adverse outcomes in extra-articular distal radius fractures is increased with malalignment in patients of all ages but mitigated in older patients. J Hand Surg 32:962–970
Földhazy Z, Törnkvist H, Elmstedt E et al (2007) Long-term outcome of nonsurgically treated distal radius fractures. J Hand Surg 32:1374–1384
Lindau TR, Aspenberg P, Arner M et al (1999) Fractures of the distal forearm in young adults. An epidemiologic description of 341 patients. Acta Orthop Scand 70:124–8
LeBoff MS, Greenspan SL, Insogna KL et al (2022) The clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. https://doi.org/10.1007/s00198-021-05900-y
Cosman F, de Beur SJ, LeBoff MS et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 25:2359–2381
Crandall CJ, Hovey KM, Andrews CA et al (2015) Bone mineral density as a predictor of subsequent wrist fractures: findings from the Women’s Health Initiative study. J Clin Endocrinol Metab 100:4315–4324
Cawthon PM (2011) Gender differences in osteoporosis and fractures. Clin Orthop 469:1900–1905
De Martinis M, Sirufo MM, Polsinelli M et al (2020) Gender differences in osteoporosis: a single-center observational study. World J Mens Health. https://doi.org/10.5534/wjmh.200099
Melton LJ 3rd (2001) The prevalence of osteoporosis: gender and racial comparison. Calcif Tissue Int 69:179–181
Hannan MT, Felson DT, Dawson-Hughes B et al (2000) Risk factors for longitudinal bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res Off J Am Soc Bone Miner Res 15:710–720
Matsumura BA, Ambrose AF (2006) Balance in the elderly. Clin Geriatr Med 22:395–412
Osoba MY, Rao AK, Agrawal SK et al (2019) Balance and gait in the elderly: a contemporary review. Laryngoscope Investig Otolaryngol 4:143–153
Syddall H, Cooper C, Martin F et al (2003) Is grip strength a useful single marker of frailty? Age Ageing 32:650–656
Dewan N, MacDermid JC, Grewal R et al (2018) Recovery patterns over 4 years after distal radius fracture: descriptive changes in fracture-specific pain/disability, fall risk factors, bone mineral density, and general health status. J Hand Ther 31:451–464
Louer CR, Boone SL, Guthrie AK et al (2016) Postural stability in older adults with a distal radial fracture. J Bone Joint Surg Am 98:1176–1182
Fujita K, Kaburagi H, Nimura A et al (2019) Lower grip strength and dynamic body balance in women with distal radial fractures. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 30:949–956
Wong RMY, Chong KC, Law SW et al (2020) The effectiveness of exercises on fall and fracture prevention amongst community elderlies: a systematic review and meta-analysis. J Orthop Transl 24:58–65
Hopewell S, Adedire O, Copsey BJ et al (2018) Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 7:CD012221
Acknowledgements
Joy C. MacDermid was supported by a Canada Research Chair in Musculoskeletal Health Outcomes and Knowledge Translation and the Dr. James Roth Chair in Musculoskeletal Measurement and Knowledge Translation. This research was made possible using the data/biospecimens collected by the Canadian Longitudinal Study on Aging (CLSA). Funding for the Canadian Longitudinal Study on Aging (CLSA) is provided by the Government of Canada through the Canadian Institutes of Health Research (CIHR) under grant reference: LSA 94473 and the Canada Foundation for Innovation as well as the following provinces: Newfoundland, Nova Scotia, Quebec, Ontario, Manitoba, Alberta, and British Columbia. This research has been conducted using the CLSA dataset (comprehensive baseline v4.1), under Application Number 1909032. The CLSA is led by Drs. Parminder Raina, Christina Wolfson, and Susan Kirkland.
Funding
This work was supported by an operating grant from the Canadian Institutes of Health Research under grant reference: 428539.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Disclaimer
The opinions expressed in this manuscript are the author’s own and do not reflect the views of the Canadian Longitudinal Study on Aging.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vincent, J.I., MacDermid, J.C., Bassim, C.W. et al. Cluster analysis to identify the profiles of individuals with compromised bone health versus unfortunate wrist fractures within the Canadian Longitudinal Study of Aging (CLSA) database. Arch Osteoporos 18, 148 (2023). https://doi.org/10.1007/s11657-023-01350-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-023-01350-7