Abstract
Summary
Osteoporosis is associated with almost all geriatric syndromes (GSs), and the occurrence of osteoporosis in patients over 65 years of age increases by 1.2–2.5 times. Early diagnosis of osteoporosis and GSs is very important. Additional programs should be adopted by the state to introduce information about the possibilities of working with elderly patients.
Purpose
To analyze associations of osteoporosis with geriatric syndromes in patients aged 65 years and older in the Russian Federation.
Methods
A total of 4308 patients (30% men) aged 65–107 years were examined and distributed into 3 age groups (65–74 years, 75–84 years, and 85 years and older). All patients underwent a comprehensive geriatric assessment. In the “Falls and risk of falls” module, the number and circumstances of falls over the previous year were analyzed, as well as the history of fractures. The presence of osteoporosis was determined based on medical records. Physical examination included anthropometric measurements and standard enquiry, short physical performance battery (SPPB), dynamometry, measurement of gait velocity, Mini-Cog test, and orthostatic test.
Results
A total of 507 patients (11.8%) had evidence of osteoporosis; indications of low-energy fractures in history were recorded in 739 (17.3%) patients. Patients with osteoporosis were older, shorter, and predominantly women; had a lower body weight and a higher Charlson comorbidity index; and took more drugs. Patients with osteoporosis had lower gait velocity, hand grip strength, Barthel index value, and scores of the Lawton instrumental activities of daily living scale, the MNA (Mini Nutritional Assessment) short-form, and the SPPB. Osteoporosis is associated with almost all geriatric syndromes (GSs), and the occurrence of osteoporosis in patients over 65 years of age increases by 1.2–2.5 times.
Conclusions
Osteoporosis is associated with almost all GSs. The association of osteoporosis with advanced GSs aggravates the condition of these patients. Early diagnosis of osteoporosis and GSs is very important. Additional programs should be adopted by the state to introduce information about the possibilities of working with elderly patients: early detection and correction of osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The global population is aging, and the proportion of the elderly people is registered in on the rise worldwide. In the middle of the twentieth century, the proportion of people over 65 years of age was 7.7% of the world’s population; over the first 20 years of the next century, the proportion of people of this age increased to 19% (2019 data), and by the middle of the twenty-first century (2050), it will be at least 27% [1]. As the population rapidly ages, interest in age-related diseases and geriatric syndromes (GSs) also rises. GS is a multifactorial age-associated clinical condition that worsens the quality of life and increases the risk of adverse outcomes (death, dependence on external assistance, repeated hospitalizations, and need for long-term care) and functional disorders [2, 3]. Age-associated diseases and GSs include disease such as osteoporosis. The term “osteoporosis” was used in France in the early nineteenth century and implied bone pathology. Osteoporosis is classified by WHO as one of the five most significant human diseases alongside infarction, stroke, cancer, and sudden death. In the mid-2000s, 33.8% of women and 26.9% of men in Russia over the age of 50 have osteoporosis. Extrapolation of the entire population of the Russian Federation revealed 14 million patients, which is about 10% of the population [4]. At present, the social significance of osteoporosis is recorded, determined by its consequences, namely low-trauma fractures of the vertebral bodies and bones of the peripheral skeleton, leading to high healthcare burden as well as significant impairments such as disability and mortality [5, 6].
At the same time, the exact prevalence of osteoporosis is unknown due to the fact that in most cases, only fractures of the proximal femur are recorded, including in elderly patients.
In Russia, data on osteoporosis is old, and generally relates to particular regions, that is why it needs to provide new investigation.
In 2018, the EVKALIPT (Epidemiological study of the prevalence of GSs and age-associated diseases in the elderly patients in regions of the Russian Federation with different climatic, economic, and demographic characteristics) study among patients aged 65 years and older was started, aimed at obtaining the prevalence of age-associated diseases, frailty syndrome, other GSs, osteoporosis, and fractures, as well as analysis of their contribution to parameters of general health and functional status in Russia. The study was performed from 2018 to 2020 in 11 regions of Russia at the initiative of the Russian Association of Gerontologists and Geriatricians and the Russian Gerontological Research and Clinical Center in cooperation with the National Research University Higher School of Economics.
Materials and methods
In a cross-sectional analytical epidemiological study, EVKALIPT included patients aged from 65 to 107 years (mean age 78 ± 8 years), from April 2018 to October 2019, who live in 11 Russian regions (Republics of Bashkortostan, Dagestan, and Chuvashia; Voronezh and the Voronezh region; Moscow; Saratov; St. Petersburg and the Leningrad region; Ivanovo, Ryazan, Samara, and Smolensk region). Inclusion criteria were age of 65 years or older and written voluntary informed consent to participate in the study. In accordance with the protocol, participants were distributed into three age groups (65–74 years, 75–84 years, and ≥ 85 years).
Initially, it was planned to include 600 people from each region (200 participants in each age group) in the study. However, only a small number of participants were included in this way. Most of the participants were recruited on the basis of seeking medical care, i.e., planned inpatient treatment in geriatric departments/hospitals, so the actual total number of participants and their distribution by age groups in individual regions did not always correspond to the planned. The majority (60%) of the participants were examined in a clinic, every fifth in a hospital (20%) or at home (19%), and 1% in nursing homes.
This data is a part of a large epidemiological study of EVKALIPT conducted in the Russian Federation. Russian EVKALIPT study protocol and basic characteristics of participants are summarized in the article [7].
All patients underwent a comprehensive geriatric assessment (CGA) in two stages: (1) survey based on a specially designed questionnaire and (2) physical examination. This was performed simultaneously by a geriatrician and a geriatric nurse at the patient’s residence (in a hospital, clinic, residential institution/assisted-living facility, or at home).
The questionnaire included the “Socio-economic status,” “Occupational history,” “Risk factors for chronic non-communicable diseases,” “Chronic non-communicable diseases,” “Drug therapy,” “Obstetrics and gynecological history,” “Falls and risk of falls,” “Chronic pain,” “Sensory deficits,” “Oral health,” “Urine and fecal incontinence,” “Use of aids,” “Laboratory examination results,” and a number of standardized scales: screening scale “Age is not a problem,” the Geriatric Depression Scale GDS-15, Basic Functional Activity Scale (Barthel Index), Lawton Instrumental Activities of Daily Living Scale, MNA (Mini Nutritional Assessment) short-form, Charlson comorbidity index, and Visual Analog Scale (VAS) for self-assessment of quality of life, health status, and intensity of pain syndrome at the time of the examination and during their stay.
For screening frailty in daily practice in Russia, they developed the questionnaire “Vozrast ne pomekha” (VNP), which translates into English as “Age is not a hindrance.” The study questionnaire was composed of seven dichotomous items for evaluation of the following characteristics: weight loss (“Did you lose 5 kg or more in the past 6 months?”), impaired vision or hearing (“Do you have any restrictions in daily living due to decreased vision or hearing?”), fall-related injuries (“Have you had any injury-related falls during the last year?”), mood disorder (“Have you felt depressed, sad or anxious over the past weeks?”), cognitive impairment (“Do you have problems with memory, comprehension, orientation or ability to plan?”), urinary incontinence (“Do you have urinary incontinence?”), and difficulty walking (“Do you have any difficulty walking at home or on the street up to a distance of 100 m, or climbing a flight of stairs?”). One point was recorded for each positive answer, so the total score ranged from 0 to 7 [8]. A score of ≥ 5 indicates a high probability of frailty syndrome. This questionnaire underwent a validation process, and the results of that process were published previously and are presented in abridged form here [9]. This scale was added in clinical guidelines on frailty in Russia [10].
The physical examination included (1) short physical performance battery tests (SPPB), (2) dynamometry, (3) measurement of gait velocity, (4) Mini-Cog test, (5) measurement of height and body weight, calculation of body mass index (BMI), (6) measurement of blood pressure (BP) and heart rate (HR), and (7) orthostatic test.
All tests, scales, and questionnaires used in the study (with the exception of the Charlson comorbidity index) are in the Russian clinical guidelines “Frailty syndrome” [10, 11]. The detailed study protocol and baseline characteristics of the participants have been presented in our previously published article [7].
The “Falls and risk of falls” module considered the number and circumstances of falls over the previous year, as well as the history of fractures (fractures of the vertebrae, femur, and radius when falling from standing height and their number, surgical treatment for fractures of the vertebrae, the need for care due to fracture, fracture of the femoral neck in parents).
The physician assessed cognitive function and completed the modules “Chronic non-communicable diseases,” “Drug therapy,” “Obstetrics and gynecological history,” and “Laboratory examination results.” The nurse completed all other modules and the physical examination.
The presence of the following GSs was determined: (1) frailty syndrome, (2) cognitive impairment, (3) depression, (4) malnutrition, (5) orthostatic hypotension, (6) urinary incontinence, (7) fecal incontinence, (8) functional disorders, (9) loss of autonomy, (10) falls (for the previous year), (11) vision deficit, (12) hearing loss, (13) sensory deficit (any), (14) chronic pain syndrome, and (15) bedsores.
Osteoporosis was diagnosed if in medical history is registered a low-trauma (i.e., fragility) fracture of major bones (vertebral or proximal femur fracture or multiple fracture), increased fracture risk using FRAX® (Fracture Risk Assessment Tool) Russian-specific threshold, or if patient had results of Bone Densitometry with T-score − 2.5 or below in the lumbar spine, femoral neck, total proximal femur, or patient’s information. A fragility fracture was mean as a fracture sustained from low-energy trauma, such as a fall from standing height or less, that would not have occurred in healthy bone, excepting fractures of the skull, face, fingers, and toes.
Characteristics of the participants
The study included 4308 patients (30% men) aged 65–107 years (Table 1). The majority (60%) of participants were examined in a polyclinic setting, 20% examined in a hospital, 19% at home, and 1% in residential institutions/assisted-living facilities. Among those examined, overweight patients prevailed (41%), while the proportion of patients with obesity and normal body weight was similar (30% and 28%), and 1.3% of participants were underweight (Table 1). Among patients with obesity, the majority of participants were obesity type I. With an increase in age, there is a decrease in height, body weight, BMI, the proportion of obese patients, and the severity of obesity, as well as an increase in the proportion of patients with normal weight. The proportion of overweight patients was identical in all age groups. The mean values of systolic and diastolic BP and heart rate were within the normal range in all patients; however, diastolic BP also decreased with age and pulse BP increased with similar identical values of systolic BP and HR.
Statistical data analysis
The study was performed using IBM® SPSS® Statistics version 23.0 (SPSS Inc., USA). The type of distribution of quantitative variables was analyzed using the one-sample Kolmogorov–Smirnov test. Results of parametric data were presented as M ± SD, where M is the mean, and SD is the standard deviation; while that of non-parametric data, the results are presented as Me (25%; 75%), where Me is the median, and 25% and 75% are the 25th and 75th percentiles. For clarity, some variables are presented simultaneously as Me (25%; 75%) and M ± SD. For intergroup comparisons, the Mann–Whitney, Kruskal–Wallis, and Pearson’s χ2 tests, as well as Fisher’s two-tailed exact test, were used. Relationships between variables were assessed using binary logistic regression with the odds ratio (OR) and 95% confidence interval (CI). One-way and multivariate regression analyses were performed after adjusting for age and gender. We analyzed the variables using the direct stepwise selection method of multivariate analysis. Differences were considered significant at a two-tailed p < 0.05.
Results
The presence of osteoporosis was determined based on past medical records. Information related to chronic disease was present for 4295 (99.7%) participants, and 507 (11.8%) were osteoporotic. Information about drugs was known in 501 (98.8%) patients with osteoporosis, and almost half (49.1%) of them were not on treatment of osteoporosis. Among all patients treated with drugs, the majority (91.4%) were on calcium and vitamin D supplements, 12 (4.7%) patients received antiresorptive therapy, 1 (0.4%) patient received bone anabolic therapy, and 9 (3.5%) patients received antiresorptive and bone-metabolic therapy.
Information related to the history of fragility fractures was available in 4275 (99.2%) participants. A history of fragility fractures was recorded in 739 (17.3%) patients, and 292 (39.6%) had a fracture of the proximal femur, 464 (63%) had a fracture of the radial bone, and 158 (21.5%) had a fracture of the vertebrae. We noted a decrease in the proportion of patients undergoing surgical treatment for vertebral fractures alongside (Table 2); there were no differences in other parameters across the age groups.
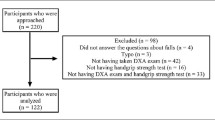
Among patients without documented osteoporosis (n = 3788), 594 (15.7%) presented with low-energy fractures in history: thus, these patients also had osteoporosis not diagnosed in a timely manner. For further analysis, patients with documented osteoporosis and with a history of fractures were combined into one group (group with osteoporosis; n = 1101). The osteoporosis group accounted for 25.6% of all patients. Comparison group consisted of patients without documented osteoporosis or history of low-energy fractures (group without osteoporosis; n = 3168). Increased prevalence of osteoporosis increased significantly with age (Fig. 1).
Patients with osteoporosis were older, shorter, and predominantly females; had a lower BMI and a higher Charlson comorbidity index; and took much more drugs (Table 3).
According to the results of CGA, patients with osteoporosis had lower gait velocity, hand grip strength, Barthel index value, Lawton Instrumental Activities of Daily Living Scale scores, MNA (Mini Nutritional Assessment) short-form, and SPPB. However, they presented with higher Geriatric Depression Scale and the screening scale “Age is not a problem” scores. Patients with osteoporosis presented with lower quality of life and health status, and higher intensity of pain syndrome at the time of examination as well as 7 days prior to examination (Table 4).
Patients with osteoporosis used assistive products more often (with the exception of spectacles/lenses which, however, they tended to use more frequently), and their number per patient was significantly higher than in those without osteoporosis (Table 5).
Patients with osteoporosis showed a higher incidence of all GSs, except for orthostatic hypotension and hearing loss (Table 6); and the most common GSs were chronic pain syndrome (95%), basic dependence in everyday life (71%), frailty syndrome (68%), cognitive impairment (65%), instrumental dependence in everyday life (58%), probable depression (57%), and urinary incontinence (57%).
A one-way regression analysis adjusted for age and gender. GSs were considered as a dependent variable, and the presence of osteoporosis, age (as an extended variable), and gender were independent variables. Results demonstrated that osteoporosis is associated with almost all GSs, with the exception of orthostatic hypotension, hearing loss, and cognitive impairment (OR from 1.19 to 3.10) (Table 7).
Multivariate regression analysis (adjusted for age and gender) included 12 GSs with a significance level of p < 0.05 based on the results of one-way analysis; the presence of osteoporosis was considered a dependent variable, and GSs, age (as an extended variable), and gender were considered independent variables. Multivariate analysis revealed that five of them were independently associated with osteoporosis and the likelihood of the occurrence of osteoporosis was multiplied 1.2–2.5 times, and in women, the risk of osteoporosis is 84% higher than in men (Table 8). The order of variables inclusion in the model was as follows: falls in the previous year, female gender, chronic pain syndrome, malnutrition, urinary incontinence, and probable depression.
Discussion
The presented subanalysis of data of the Russian epidemiological study EVKALIPT reveals that the prevalence of osteoporosis in patients based on the survey was 11.8% (n = 507). In addition, a group of patients with a history of low-energy fractures (n = 594; 15.7%) was identified according to modern criteria, and also who had osteoporosis; however, it was not diagnosed in time. For further analysis, these patients were combined into one group with patients with registered osteoporosis (osteoporosis group: n = 1101). Consequently, the prevalence of osteoporosis in patients aged 65 years and older increases to 25.6% with a predominance in women. Most guidelines and publications include information obtained in the early 2000s based on the results of a cluster cross-sectional study in a random sample of one of the districts of Moscow, when osteoporosis was diagnosed in patients aged 50 years and older based on changes in DXA densitometry in spine and/or proximal femur, and was detected in 33.8% of women and 26.9% of men [4]. However, we examined the indices of patients 15 years younger in this study. The prevalence of osteoporosis is known to increase with age [12]. In our study, this trend was also demonstrated and the maximum prevalence was recorded in patients over 85 years of age (29.1%) (Fig. 1). According to the social research program conducted by the US National Center for Health Statistics, National Health and Nutrition Examination Survey, from 1988 to 1994, 1.3 and 1.6% of men and 12.1 and 9.7% of women aged 75–84 years and 85 years and older, respectively, were surveyed and reported having osteoporosis; however, densitometry detected this disease already in 6.4 and 13.7% of men and 32.5 and 50.5% of women in the corresponding age categories [13]. Thus, in the Russian study EVKALIPT, we established a similar awareness (11.6%) about the presence of osteoporosis. The lack of information about instrumental examination, and in particular densitometry, limits our data obtained. In 2017–2018, in the USA, the prevalence of osteoporosis in patients over 65 years old was studied based on instrumental data alone (low BMD according to densitometry results), and it amounted to 17.7% [14]. In a European study, among patients of all ages with osteoporosis diagnosed based on a decrease in BMD in the femur, the overall prevalence was 5.6% [15].
According to Russian experts in the field of epidemiology, it has been established that the prevalence of osteoporosis in women in the Russian Federation is comparable to global data, and Russian women are of average risk of osteoporosis on a pair with residents of North America and Western Europe, and in Russian men, it exceeds the prevalence of osteoporosis in North America and Western Europe [4]. In the EVKALIPT study, women obviously predominated in the osteoporosis group among patients aged 65 years and older (Table 3). Thus, in general, the prevalence of osteoporosis in Russia is comparable to that in other countries.
The social and medical significance of osteoporosis is determined by the fractures caused by it [5]. In the EVKALIPT study, 17% of patients had a history of low-energy fractures (Table 2). According to localization, fractures of the radial bone in the history prevailed (10.8%), proximal femur fractures were less common (6.8%), and fractures of the vertebrae due to a fall from standing height in the history rarely occurred (3.7%) (Table 2). Fractures of the radial bone were more common in patients aged 75–84 years, and fractures of the proximal femur and vertebrae were registered more often in patients older than 85 years. At the age of 50 years, the probability of fracture of the proximal femur during the subsequent life in the Russian Federation is 4% for men and 7% for women. In 2010, the number of fracture cases of the proximal femur in Russia was 112,000 cases; by 2035, due to increased life expectancy alone, it will increase by 36% in men and 43% in women, and will amount to 159 thousand cases per year [16]. According to available statistics, the prevalence of bone fractures in Russia is 18.6 cases per 1000 adult population, or 21.5% [4], which is somewhat higher than in our study. Osteoporotic vertebral fractures represent a serious problem, which is due not only to their high real prevalence and low detectability, but also to a significant impact on the decrease in the quality of life [17]. Studies conducted earlier in three cities of Russia (Moscow, Yekaterinburg, and Yaroslavl) showed that the prevalence of these fractures is 7.2% and higher in men and 7% and higher in women, but again at a younger age [18]. Nevertheless, the results of detection of vertebral fractures in the EVKALIPT study (3.7%) still indicate their insufficient diagnostics in patients over 65 years of age. At the same time, the vast majority of them had fractures of the radial bone (Table 2). This type of fracture (distal part of the forearm) is one of the most common fractures in a fall from standing height. According to an epidemiological study in Russia, its frequency was 426/100,000 of the population, exceeding the incidence of femoral fracture by 3–7 times in men and 4–8 times in women, and significantly prevailing in women. In our study, the first fracture of the radial bone most often occurred at the age of 65–74 years, but a repeated fracture of the same location was registered already at the age of 75–84 years, which is consistent with the data that the risk of a subsequent fracture after the initial fracture increases by 1.6–4.3 times at any age [19].
However, it is noteworthy that in 594 (15.77%) patients with a history of fracture in the subanalysis presented, osteoporosis was not diagnosed and, accordingly, no treatment was prescribed. When analyzing data from 6 European countries (France, Spain, Italy, Great Britain, Sweden), 60–85% of women with a history of fracture also did not receive subsequent treatment for osteoporosis [20]. Our study revealed that only 12 (4.7%) patients received antiresorptive therapy, 1 (0.4%) patient received bone anabolic therapy, and 9 (3.5%) patients received both antiresorptive and bone-metabolic therapy; however, 91.4% of patients still confirmed the prescription of vitamin D and calcium supplements. These data indicate insufficiently complete treatment of osteoporosis. Similar results were obtained in Europe; thus, 71% of women with indications for anti-osteoporotic treatment did not receive this therapy [15]. These findings can be due to a number of factors, including the low awareness of doctors and patients about the need for osteoporosis treatment, the need for long-term treatment of osteoporosis, the high cost of drugs for the treatment of osteoporosis, and the large number of drugs taken for other diseases. Thus, in the osteoporosis group, a greater number of patients were recorded who took 5 or more drugs. Polypharmacy is a GS which is often cited as a potential barrier to adherence to the regimen of drug intake, used to treat osteoporosis, and is an independent negative factor in long-term therapy [21]. It has been revealed that women taking medications for other diseases were less adherent to osteoporosis therapy, and those who used more than ten drugs had a 1.87-fold risk of being non-adherent compared to those who did not use medications [22].
Patients with osteoporosis have a high comorbidity, a burdened geriatric status [12]. Thus, in our study, the greatest number of GSs was revealed in patients with osteoporosis, with the exception of orthostatic hypotension and hearing loss (Table 6). In addition, osteoporosis, being associated with almost all GSs (OR 1.19–3.10), was not associated with orthostatic hypotension, hearing loss, and cognitive impairment (Table 7). This could be explained by the fact that patients over 65 years of age with osteoporosis frequently used hearing aids than patients without osteoporosis (Table 5). Osteoporosis, as a change in bone mineral density, obviously develops at an earlier age than the main many GSs. However, osteoporosis is diagnosed at an older age, when GSs already appear and are detected (addiction in everyday life, various sensitivity disorders, frailty syndrome, malnutrition, signs of immobility, such as fecal incontinence, bedsores, and falls, as well as chronic pain). It should be noted that in patients of the age categories considered, significant hormonal changes occur in the body, namely the levels of growth hormone, sex hormones, and insulin-like growth factor as well as their bioavailability (decreases). Such changes lead to impaired osteogenesis and increased bone resorption. A significant contribution to the pathogenesis of bone aging is due to vitamin D deficiency that increases with age and is aggravated by such GSs as malnutrition. Such an association of GSs and osteoporosis arises possibly, among other things, due to increased immune inflammation and secretion of pro-inflammatory interleukins (IL-1, IL-6) and TNF. Aged patients have decreased glomerular filtration rate which exacerbates age-related vitamin D deficiency. All these changes initiate the progression of osteoporosis in patients over 65 years of age [23, 24]. Thus, geriatric syndromes are associated with the presence of osteoporosis and its severity. The results of the association of most GSs and osteoporosis are consistent with the findings obtained in a study conducted at the Russian Gerontological Research and Clinical Center among patients of the geriatric therapy department, which revealed that patients with osteoporosis had frailty syndrome, malnutrition, and physical inactivity significantly more often (p < 0.001) [25]. So the geriatric status of older patients with osteoporosis tends to be worse.
It should be noted that weight loss and a decrease in muscle mass/strength are associated with frailty syndrome and are signs of sarcopenia [26]. Sarcopenia is a progressive generalized skeletal muscle disorder associated with a high risk of adverse outcomes, including falls, fractures, and physical disability as well as death. Sarcopenia and osteopenia have common risk factors and pathogenesis and are associated with myogenesis and osteogenesis. The combination of sarcopenia and osteoporosis/osteopenia is called sarcoosteopenia. In 2009, this term was first used in elderly patients with a higher risk of falls, fractures, disability, and decrepitude [27]. In our study, muscle strength was assessed using carpal dynamometry (Table 4). In the osteoporosis group, muscle strength was reduced in 73% of patients; in the same group, the SPPB score was lower (Table 4). Thus, the decrease in these indicators in the osteoporosis group was due to osteosarcopenia. Age-related changes in the hormonal and metabolic status in combination with the majority of GSs and the probable development of osteosarcopenia, as well as changes in the life status of a person with age, could explain the results of the multivariate analysis (Table 8).
Conclusion
Osteoporosis is a severe age-related disease that can lead to poor outcomes. Geriatric syndromes are associated with the presence of osteoporosis and its severity; so the geriatric status of older patients with osteoporosis tends to be worse. The association of osteoporosis with a large number of GSs aggravates the condition of these patients making treatment difficult. Therefore, scheduled, early, and timely diagnosis of osteoporosis (careful assessment of the history of falls, fractures, and their localization, as well as changes in anthropometric parameters, namely reduced height) and GSs, as well as development of an individual treatment plan to alleviate the condition of these patients, is of great clinical utility. “Treat the patient the way you would like to be treated” is an ancient truth which is at the core of medicine. It is an obvious fact that important, new, and interesting conclusions were made in the EVKALIPT study, despite its complicated, time-consuming, and diverse nature. Success and efficiency in the management are achieved only in a team approach to solving problems. Thus, it is necessary to adopt additional programs at the state level to introduce information about GSs and opportunities to work with elderly patients; timely (early) detection and correction of osteoporosis; and dissemination of information among medical workers, patients, and their relatives.
Limitations of the study
-
1.
One of the disadvantages is the fact that the diagnosis of osteoporosis was revealed on the past medical history, which limits us in comparison with other studies where DXA was performed.
-
2.
The study focuses on 3 localizations of osteoporotic fractures, which we believe are the most important and relevant. Other fractures are less often taken into account by patients and doctors, and are more difficult to statistically analyze.
Data availability
The data that support the findings of this study are available on request from the corresponding author [OnuchinaY.S.]. The data are not publicly available due to them containing information that could compromise research participant privacy/consent.
Change history
02 March 2023
A Correction to this paper has been published: https://doi.org/10.1007/s11657-023-01228-8
References
Beard JR, Officer A, de Carvalho IA et al (2016) The World report on ageing and health: a policy framework for healthy ageing. Lancet 387(10033):2145–2154
Inouye SK, Studenski S, Tinetti ME, Kuchel GA (2007) Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc 55:780–791
Rosso AL, Eaton CB, Wallace R, Gold R, Stefanick ML, Ockene JK et al (2013) Geriatric syndromes and incident disability in older women: results from the women’s health initiative observational study. J Am Geriatr Soc 61:371–379
Lesnyak OM, Baranova IA, Belova KYu, Gladkova EN, Evstigneeva LP, Ershova OB, Karonova TL, Kochish AYu, Nikitinskaya OA, Skripnikova IA, Toroptsova NV, Aramisova RM (2018) Osteoporosis in the Russian Federation: epidemiology, medical, social, and economic aspects of the problem (literature review). Travmatologiya i ortopediya Rossii 24(1):155–167
Camacho PM, Petak SM, Binkley N et al (2020) American Association of Clinical Endocrinologists/American College of Endocrinology Clinical Practice Guidelines for the Diagnosis and Treatment of Postmenopausal Osteoporosis-2020 Update. Endocr Pract 26(Suppl 1):1–46. https://doi.org/10.4158/GL-2020-0524SUPPL
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8(1):136. https://doi.org/10.1007/s11657-013-0136-1
Vorobyeva NM, Tkacheva ON, Kotovskaya Yu V et al (2021) Russian epidemiological study EVKALIPT: protocol and basic characteristics of participants. Russ J Geriatr Med (1):35–43
Tkacheva ON, Runikhina NK, Ostapenko VS et al (2018) Prevalence of geriatric syndromes among people aged 65 years and older at four community clinics in Moscow. Clin Interv Aging 251–259
Tkacheva ON, Runikhina NK, Ostapenko VS et al (2017) Validation of the questionnaire for screening frailty. Adv Gerontol 30(2):236–242
Tkacheva N, Yu V, Kotovskaya NK, Runikhina EV et al (2020) Clinical recommendations frailty syndrome. Russ J Geriatr Med (1):11–46
Tkacheva ON, Kotovskaya YV, Runikhina NK et al (2020) Clinical guidelines frailty. Part 2. Russ J Geriatr Med (2):115–130. https://doi.org/10.37586/2686-8636-2-2020-115-130
Aspray TJ, Hill TR (2019) Osteoporosis and the ageing skeleton. Subcell Biochem 91:453–476. https://doi.org/10.1007/978-981-13-3681-2_16
Vondracek SF, Linnebur SA (2009) Diagnosis and management of osteoporosis in the older senior. Clin Interv Aging 4:121–136
Sarafrazi N, Wambogo EA, Shepherd JA (2021) Osteoporosis or low bone mass in older adults: United States, 2017–2018. NCHS Data Brief (405):1–8
Kanis JA, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon M, McCloskey EV, Willers C, Borgström F (2021) SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos 16(1):82. https://doi.org/10.1007/s11657-020-00871-9
Lesnyak OM, Ershova OB, Belova KYu, Gladkova EN et al (2014) Epidemiology of osteoporotic fractures in the Russian Federation and the Russian FRAX model. Osteoporoz i osteopatii, No 3:3–8
Johansson L, Sundh D, Nilsson M et al (2018) Vertebral fractures and their association with health-related quality of life, back pain and physical function in older women. Osteoporos Int 29(1):89–99
Evstigneeva LP, Piven AI (2001) Epidemiology of osteoporotic vertebral fractures among population sample of inhabitants of the Yekaterinburg city of 50 years and older based on X-ray morphometric analysis. Osteoporoz i osteopatii [Osteoporosis and and Bone Diseases] 2:2–6
Hodsman AB, Leslie WD, Tsang JF et al (2008) 10-year probability of recurrent fractures following wrist and other osteoporotic fractures in a large clinical cohort: an analysis from the Manitoba Bone Density Program. Arch Intern Med 168(20):2261–2267
Borgström F et al (2020) Fragility fractures in Europe : burden, management and opportunities. Arch Osteoporos 15:59
Weiss TW, Henderson SC, McHorney CA, Cramer JA (2007) Persistence across weekly and monthly bisphosphonates: analysis of US retail pharmacy prescription refills. Curr Med Res Opin 23(9):2193–2203
Penning-van Beest FJ, Erkens JA, Olson M, Herings RM (2008) Determinants of non-compliance with bisphosphonates in women with postmenopausal osteoporosis. Curr Med Res Opin 24(5):1337–1344
Soysal P, Stubbs B, Lucato P et al (2016) Inflammation and frailty in the elderly: a systematic review and meta-analysis. Ageing Res Rev 31:1–8. https://doi.org/10.1016/j.arr.2016.08.006
Ma L, Sha G, Zhang Y, Li Y (2018) Elevated serum IL-6 and adiponectin levels are associated with frailty and physical function in Chinese older adults. Clin Interv Aging 13:2013–2020. https://doi.org/10.2147/CIA.S180934
Khovasova NO, Naumov AV, Tkacheva ON, Dudinskaya EN (2021) Characteristics of geriatric and somatic status in patients with osteoporosis. Problemy endokrinologii, No 67(3):45–54
Cruz-Jentoft AJ, Sayer AA (2019) Sarcopenia. Lancet 393(10191):2636–2646
Binkley N, Buehring B (2009) Beyond FRAX: It’s time to consider ‘sarco-osteopenia.’ J Clin Densitom 12(4):413–416
Author information
Authors and Affiliations
Contributions
Dudinskaya Ekaterina N.—substantial contributions to conception and design, acquisition of data, analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, and approval of the version to be published and all subsequent versions.
Vorobyeva Natalia M.—substantial contributions to conception and design, acquisition of data, analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, and approval of the version to be published and all subsequent versions.
Onuchina Julia S.—substantial contributions to conception and design, acquisition of data, analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, and approval of the version to be published and all subsequent versions.
Machekhina Lubov V.—substantial contributions to conception and design, acquisition of data, analysis and interpretation of data, and approval of the version to be published and all subsequent versions.
Selezneva Elena V.—substantial contributions to conception and design, acquisition of data, and analysis and interpretation of data.
Ovcharova Lilia N.—substantial contributions to conception and design acquisition of data and analysis and interpretation of data.
Kotovskaya Yulia V.—substantial contributions to conception and design, or acquisition of data, analysis and interpretation of data, and approval of the version to be published and all subsequent versions.
Tkacheva Olga N.—substantial contributions to conception and design, acquisition of data, analysis and interpretation of data, and approval of the version to be published and all subsequent versions.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Russian Gerontology Research and Clinical Centre Ethics Committee (No. 262). Informed consent was obtained from all individual participants included in the study.
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to a retrospective Open Access order.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dudinskaya, E.N., Vorobyeva, N.M., Onuchina, J.S. et al. The association of osteoporosis and geriatric syndromes in the elderly: data from the Russian epidemiological study EVKALIPT. Arch Osteoporos 18, 30 (2023). https://doi.org/10.1007/s11657-023-01217-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-023-01217-x