Abstract
Summary
The study examined the risk factors of recurrent fragility fractures in elderly. Female and older age increased the risk of refracture. Older age at the first fracture also resulted in shorter time to the second fracture. The prevention program should be emphasized.
Purpose
The study examined the characteristics of the fragility fractures and refractures and the factors affecting the incidence and duration to the second fragility fracture.
Methods
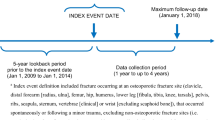
The retrospective cohort study reviewed electronic medical records from Nan Provincial Public Health Office, Thailand. Patients aged ≥ 60 years with fragility fractures (hip, wrist, vertebra, and proximal humerus) from low-energy injuries between 1 January 2009 and 31 December 2018 were included. The characteristics of the first and second fractures and the factors that had effect on refracture incidence and duration were investigated.
Results
Among 4322 patients, 306 patients (7%) had subsequent fragility fractures. Risk factors of refracture included female (adjusted odd ratio 1.79, 95%CI 1.304–2.467) and older age at the first fracture (adjusted odd ratio 1.016, 95%CI 1.003–1.029). Factor resulted in shorter time to second fracture was older age at the first fracture (β-coefficient − 0.96, 95%CI − 1.4–(− 0.5)). Any type of the first fracture resulted in similar risk and duration to subsequent fracture. Half (48%) and two-third (65%) of the second fractures occurred within 3 and 4 years, respectively.
Conclusion
Female and older age were risk factors of subsequent fragility fracture. Older age resulted in shorter time to the second fracture. Refracture prevention program should be initiated in patients with any type of first fragility fracture and should be continued for at least 3–4 years.
Similar content being viewed by others
References
Center JR, Bliuc D, Nguyen TV, Eisman JA (2007) Risk of subsequent fracture after low-trauma fracture in men and women. JAMA 297(4):387–394. https://doi.org/10.1001/jama.297.4.387
Stone KL, Seeley DG, Lui LY, Cauley JA, Ensrud K, Browner WS et al (2003) BMD at multiple sites and risk of fracture of multiple types: long-term results from the Study of Osteoporotic Fractures. J Bone Miner Res 18(11):1947–1954. https://doi.org/10.1359/jbmr.2003.18.11.1947
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J et al (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8(1):136. https://doi.org/10.1007/s11657-013-0136-1
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359(9319):1761–1767. https://doi.org/10.1016/s0140-6736(02)08657-9
Odén A, McCloskey EV, Kanis JA, Harvey NC, Johansson H (2015) Burden of high fracture probability worldwide: secular increases 2010–2040. Osteoporos Int 26(9):2243–2248. https://doi.org/10.1007/s00198-015-3154-6
Leboime A, Confavreux CB, Mehsen N, Paccou J, David C, Roux C (2010) Osteoporosis and mortality. Joint Bone Spine 77(Suppl 2):S107-12. https://doi.org/10.1016/s1297-319x(10)70004-x
Gibson-Smith D, Klop C, Elders PJ, Welsing PM, van Schoor N, Leufkens HG et al (2014) The risk of major and any (non-hip) fragility fracture after hip fracture in the United Kingdom: 2000–2010. Osteoporos Int 25(11):2555–2563. https://doi.org/10.1007/s00198-014-2799-x
Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P et al (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35(2):375–382. https://doi.org/10.1016/j.bone.2004.03.024
Montoya-García MJ, Giner M, Marcos R, García-Romero D, Olmo-Montes FJ, Miranda MJ et al. (2021) Fragility fractures and imminent fracture risk in the Spanish population: a retrospective observational cohort study. J Clin Med 10(5). https://doi.org/10.3390/jcm10051082
Shim YB, Park JA, Nam JH, Hong SH, Kim JW, Jeong J et al (2020) Incidence and risk factors of subsequent osteoporotic fracture: a nationwide cohort study in South Korea. Arch Osteoporos 15(1):180. https://doi.org/10.1007/s11657-020-00852-y
Wong RMY, Ho WT, Wai LS, Li W, Chau WW, Chow KS et al (2019) Fragility fractures and imminent fracture risk in Hong Kong: one of the cities with longest life expectancies. Arch Osteoporos 14(1):104. https://doi.org/10.1007/s11657-019-0648-4
Tsuda T (2017) Epidemiology of fragility fractures and fall prevention in the elderly: a systematic review of the literature. Curr Orthop Pract 28(6):580–585. https://doi.org/10.1097/bco.0000000000000563
Yamanashi A, Yamazaki K, Kanamori M, Mochizuki K, Okamoto S, Koide Y et al (2005) Assessment of risk factors for second hip fractures in Japanese elderly. Osteoporos Int 16(10):1239–1246. https://doi.org/10.1007/s00198-005-1835-2
Banefelt J, Åkesson KE, Spångéus A, Ljunggren O, Karlsson L, Ström O et al (2019) Risk of imminent fracture following a previous fracture in a Swedish database study. Osteoporos Int 30(3):601–609. https://doi.org/10.1007/s00198-019-04852-8
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381. https://doi.org/10.1007/s00198-014-2794-2
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15(4):721–739. https://doi.org/10.1359/jbmr.2000.15.4.721
Ross PD, Davis JW, Epstein RS, Wasnich RD (1991) Pre-existing fractures and bone mass predict vertebral fracture incidence in women. Ann Intern Med 114(11):919–923. https://doi.org/10.7326/0003-4819-114-11-919
Cuddihy MT, Gabriel SE, Crowson CS, O’Fallon WM, Melton LJ 3rd (1999) Forearm fractures as predictors of subsequent osteoporotic fractures. Osteoporos Int 9(6):469–475. https://doi.org/10.1007/s001980050172
Söreskog E, Ström O, Spångéus A, Åkesson KE, Borgström F, Banefelt J et al (2020) Risk of major osteoporotic fracture after first, second and third fracture in Swedish women aged 50 years and older. Bone 134:115286. https://doi.org/10.1016/j.bone.2020.115286
Dang DY, Zetumer S, Zhang AL (2019) Recurrent fragility fractures: a cross-sectional analysis. J Am Acad Orthop Surg 27(2):e85–e91. https://doi.org/10.5435/jaaos-d-17-00103
Balasubramanian A, Zhang J, Chen L, Wenkert D, Daigle SG, Grauer A et al (2019) Risk of subsequent fracture after prior fracture among older women. Osteoporos Int 30(1):79–92. https://doi.org/10.1007/s00198-018-4732-1
Kanis JA, Johnell O, Oden A, Sembo I, Redlund-Johnell I, Dawson A et al (2000) Long-term risk of osteoporotic fracture in Malmö. Osteoporos Int 11(8):669–674. https://doi.org/10.1007/s001980070064
Ensrud KE, Blackwell TL, Fink HA, Zhang J, Cauley JA, Cawthon PM et al (2016) What proportion of incident radiographic vertebral fractures in older men is clinically diagnosed and vice versa: a prospective study. J Bone Miner Res 31(8):1500–1503. https://doi.org/10.1002/jbmr.2831
Kendler DL, Bauer DC, Davison KS, Dian L, Hanley DA, Harris ST et al (2016) Vertebral fractures: clinical importance and management. Am J Med 129(2):221.e1–10. https://doi.org/10.1016/j.amjmed.2015.09.020
Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM et al (2011) Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int 22(5):1277–1288. https://doi.org/10.1007/s00198-011-1601-6
Baba T, Hagino H, Nonomiya H, Ikuta T, Shoda E, Mogami A et al (2015) Inadequate management for secondary fracture prevention in patients with distal radius fracture by trauma surgeons. Osteoporos Int 26(7):1959–1963. https://doi.org/10.1007/s00198-015-3103-4
Osuna PM, Ruppe MD, Tabatabai LS (2017) Fracture liaison services: multidisciplinary approaches to secondary fracture prevention. Endocr Pract 23(2):199–206. https://doi.org/10.4158/ep161433.ra
Frenkel Rutenberg T, Vitenberg M, Haviv B, Velkes S (2018) Timing of physiotherapy following fragility hip fracture: delays cost lives. Arch Orthop Trauma Surg 138(11):1519–1524. https://doi.org/10.1007/s00402-018-3010-1
Wasfie T, Jackson A, Brock C, Galovska S, McCullough JR, Burgess JA (2019) Does a fracture liaison service program minimize recurrent fragility fractures in the elderly with osteoporotic vertebral compression fractures? Am J Surg 217(3):557–560. https://doi.org/10.1016/j.amjsurg.2018.09.027
Bonafede M, Shi N, Barron R, Li X, Crittenden DB, Chandler D (2016) Predicting imminent risk for fracture in patients aged 50 or older with osteoporosis using US claims data. Arch Osteoporos 11(1):26. https://doi.org/10.1007/s11657-016-0280-5
Kanis JA, Cooper C, Rizzoli R, Abrahamsen B, Al-Daghri NM, Brandi ML et al (2017) Identification and management of patients at increased risk of osteoporotic fracture: outcomes of an ESCEO expert consensus meeting. Osteoporos Int 28(7):2023–2034. https://doi.org/10.1007/s00198-017-4009-0
Roux C, Briot K (2017) Imminent fracture risk. Osteoporos Int 28(6):1765–1769. https://doi.org/10.1007/s00198-017-3976-5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sriruanthong, K., Philawuth, N., Saloa, S. et al. Risk factors of refracture after a fragility fracture in elderly. Arch Osteoporos 17, 98 (2022). https://doi.org/10.1007/s11657-022-01143-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01143-4