Abstract
Summary
Low serum vitamin D and increased parathormone levels were found to be associated with depression and stress in a wintering expedition of 20 healthy male subjects over a period of 1 year in Antarctica. The continuous daylight during summer and the dark polar winter affect endogenous vitamin D production. Long-term effects on bone health need to be studied further.
Purpose
Vitamin D plays a significant role in calcium and bone mineral metabolism and also affects cardiovascular, psychological, and cognitive functions. The ultraviolet B radiation component of sunlight, which shows marked seasonal variation in Antarctica, influences the synthesis of vitamin D. Depression and mood disorders are associated with this extreme photoperiod. In this study, we attempted to gauge the alteration of vitamin D homeostasis in Antarctica and its effect on bone mineral metabolism and mood over a period of 1 year.
Materials and methods
Twenty male subjects who wintered over at India’s Antarctic base Maitri (70°45′57″ S, 11°44′09″ E) from November 2010 to December 2011 were studied. Fasting serum samples were collected at baseline, 6 months, and 12 months for serum 25-hydroxyvitamin D, intact parathyroid hormone (PTH), total alkaline phosphatase (ALP), calcium, and phosphate. Beck Depression Inventory (BDI), Positive and Negative Affect Scale (PANAS X), and Perceived Stress Scale were used to measure depression, affect, and stress.
Results
Mild vitamin D deficiency was present in two (10 %) subjects on arrival, which increased to seven (35 %) subjects during the polar winter at 6 months. The mean score on the BDI-II screen for depression was significantly higher during midwinter (4.8 ± 3.9) when compared with the baseline value (2.9 ± 2.1). Only 2/20 (10 %) of subjects met the criteria for minor depression. Higher PTH levels at 6 months correlated with a higher PANAS X score (p = 0.021). The mean values of calcium, inorganic phosphorus, and ALP were comparable during the course of the expedition.
Conclusion
Low light exposure during the dark polar winter, lower vitamin D, and increased intact PTH levels were found to be associated with depression during 1 year of Antarctic residence. The low dietary intake and decreased solar radiation exposure during the polar winter reduce serum vitamin D levels in otherwise healthy individuals, which suggests that supplementation may be necessary.
Similar content being viewed by others
Introduction
Vitamin D deficiency is now acknowledged to be widespread in various studies in India. Research in different countries and ethnic groups has revealed that vitamin D concentrations which were considered normal previously may not be sufficient for optimal health [1–4]. While the association of vitamin D deficiency (VDD) with musculoskeletal disease is well described, new insight into the role of this vitamin in cardiovascular disease, neuroendocrine metabolism, cancer, and diabetes is being researched [5, 6]. Recently, a role for vitamin D in mental health and cognitive function has been reported [7, 8]. Depression has also been associated with vitamin D deficiency. Vitamin D receptors are found in the central nervous system, and enzymes necessary for hydroxylation of this vitamin have been identified in brain tissue, making a possible substrate for stress, cognition, and mood disorders. This is especially so in the amygdala of the limbic system, a control center of behavior and emotion [9, 10]. Another mechanism for vitamin D to cause depression is high parathyroid hormone (PTH) levels. Hyperparathyroidism is often associated with depression [11].
Residence in Antarctica exposes humans working in the research bases to extremes of weather, photoperiod, geographic, and social isolation and in itself is associated with changes in behavior and frequently leads to depression and mood disorders [12]. The members of over-wintering teams are exposed to about 4 months of continuous darkness during winter and 4 months of continuous daylight during the summer photoperiod. Light therapy has been shown to improve depressive symptoms in conjunction with antidepressants, which may be partially explained by improved endogenous vitamin D synthesis [13, 14].
A large population-based study, performed as part of the third National Health and Nutrition Examination Survey on over seven thousand young adults, concluded that the likelihood of depression is significantly higher in patients with serum vitamin D deficiency [5]. Clinicians and researchers should note that “population-based reference values” (e.g., derived from blood donors, etc.), developed by the kit manufacturers, are depicted as a “reference range” and are usually employed to define vitamin D deficiency. These values are affected by climate, sunlight exposure, and clothing habits, among others, and could therefore vary according to other local conditions. Therefore, investigators working with diverse test groups use different “reference populations,” making comparison difficult in different regions of the world. A “functional health-based reference value” based on the levels of vitamin D and PTH has been proposed. This defines vitamin D deficiency as “the critical level of 25(OH) D which prevents secondary hyperparathyroidism.” A functional staging of vitamin D deficiency has been proposed by Lips and is based on 25(OH) D levels, increase in serum PTH, and changes in bone histology. Mild vitamin D deficiency is defined as 25(OH) D levels of 10–20 ng/ml, 15 % increase in the PTH level, and normal or high turnover in bone histology. Moderate vitamin D deficiency is defined as 25(OH) D levels of 5–10 ng/ml, 15–30 % increase in the PTH level, and high turnover in bone histology; severe vitamin D deficiency is defined as 25(OH) D levels <5 ng/ml, >30 % increase in the PTH level, and mineralization defect/incipient or overt osteomalacia in bone histology. This classification encompasses the “vitamin D–calcium–PTH axis” and its impact on health [15–17].
The objective of this study was to evaluate the seasonal variation in vitamin D and PTH metabolism in 20 apparently healthy male subjects over a period of 1 year in Antarctica and to correlate these changes with objective measures of depression and perceived stress, and change in biochemical markers of bone mineral metabolism such as total serum calcium (Ca), inorganic phosphorus (iP), and total alkaline phosphatase (ALP). We also attempted to assess the dietary intake of vitamin D in the changed Indian diet in Antarctica and quantify sunlight exposure of the subjects during the polar seasonal photoperiods. Lastly, we assessed the association of vitamin D and PTH with depression in relation to age, season, and work in Antarctica.
Methods
Study design
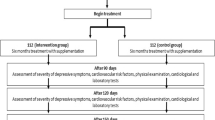
Twenty male members of the 30th Indian Scientific Expedition to Antarctica, certified to be in good mental and physical health and free of intrinsic sleep disorders following medical and psychiatric examination and acclimatization training, were recruited for this prospective study with written informed consent. The study was approved by an Institutional Ethics Board of the National Centre for Antarctic and Ocean Research (NCAOR), India’s nodal agency for Antarctic research, and was conducted in accordance with the standards of the Declaration of Helsinki. The study was started in November 2010 soon after the arrival of team members in Antarctica, and the group was followed up prospectively till the conclusion of the expedition in December 2011. The Indian Antarctic research base Maitri is located at 70°45′57″ S, 11°44′09″ E. The over-wintering team consisted of 6 scientists and 14 technical support staff who are required to keep the base functional and the scientific experiments running.
Procedure
Demographic data were recorded at the start of the study, and anthropometric and clinical data were collected on a monthly basis during the course of the expedition. The baseline samples (0 month) for vitamin D, intact PTH, calcium, phosphate, and ALP were collected soon after arrival in Antarctica and processed to obtain serum which was stored at −25 °C until assay was done. Repeat serum samples were drawn at 6 months and 12 months of the expedition. The polar night lasts from May through July at Maitri, Antarctica. Therefore, at 0 month (December 2010) and at 12 months (December 2011), the collection was during the polar summer. At 6 months, the sample represents collection in July, during the dark polar midwinter. These were stored at −25 °C in Antarctica and transported back to India on dry ice at a monitored temperature between −25 and −70 °C using cold chain transport. The tests for 25-hydroxyvitamin D, i.e., 25(OH) D, and intact PTH were done by radioimmunoassay kits (DiaSorin RIA kits, Stillwater, MN, USA). The reference range for serum 25(OH) D was 9.0–37.6 ng/ml with intra- and inter-assay variabilities of 4 and 5.8 %, respectively. The reference range for intact PTH was 10–65 pg/ml with intra- and inter-assay variabilities of 3.6 and 3.4 %, respectively, as stated by the manufacturer. The normal ranges for serum total calcium (8.8–10.3 mg/dl), inorganic phosphorus (2.7–4.5 mg/dl), and alkaline phosphatase (< 270 U/l) are as stated. The assay consists of a two-step procedure. The first step involves a rapid extraction of 25(OH) D and other hydroxylated metabolites with acetonitrile. After extraction, the treated sample was then assayed using an equilibrium RIA technique that uses a specific 25(OH) D antibody.
The instruments for assessing physical and mental health included standardized scales such as Subjective Health Complaints (SHC) [18], Positive and Negative Affect Scale (PANAS X) [19], Beck Depression Inventory (BDI) [20], and Perceived Stress Scale (PSS) which were administered at baseline [21], during summer, and during winter. Depression was defined by International Classification of Diseases, Ninth Edition, codes: 296.2 to 296.36,311. The SHC inventory assesses subjective somatic and psychological complaints and consists of 29 items which are graded on a four-point Likert scale from 0 (no complaint) to 3 (serious). The inventory subscales for musculoskeletal disease (headache, neck pain, upper back pain, low back pain, arm pain, shoulder pain, headache, and leg pain), pseudoneurology (palpitation, heat flushes, sleep disturbance, anxiety, tiredness, and dizziness), and gastrointestinal complaints (heartburn, epigastric distress, dyspepsia, abdominal pain, diarrhea, and constipation) were evaluated. The SHC has demonstrated validity and reliability for measuring health complaints.
The PANAS X scale is a 60-item schedule which was administered on arrival in summer, during midwinter, and before departure. The scale consists of words measuring positive affect (active, alert, attentive, determined, enthusiastic, excited, inspired, interested, proud, and strong), negative affect (afraid, scared, nervous, jittery, irritable, hostile, guilty, ashamed, upset, and distressed), and three higher order scales for basic negative emotion (fear, hostility, guilt, and sadness), basic positive emotion (joviality, self-assurance, and attentiveness), and other affective states (shyness, fatigue, serenity, and surprise).
BDI and PSS are validated instruments for measurement of depression and stressful events, respectively. BDI-II measures the behavioral manifestations of depression in separate interviews 2 weeks apart to construct a score. The PSS is an instrument with 10 questions grading the individual’s perception of stressful situations over a month using a five-point scale.
Dietary assessment of vitamin D, calcium, and phosphate intake was done during summer and again during midwinter using a standardized food frequency questionnaire over a 1-month recall period developed by the Block–National Cancer Institute Health Habits and History Questionnaires (DHQ II) and a short screening instrument derived from Block–National Cancer Institute Health Habits and History Questionnaire. The positive predictive value of the short screening instrument in identifying individuals with low nutrient intakes, as assessed by the 7-day food diary, was 91.7 % for calcium and 100.0 % for vitamin D [22, 23]. Data were analyzed using the Diet*Calc analysis program and the DHQ II nutrient database. The nutrient database was modified for Indian foods using food composition tables. Subjects who were on calcium and vitamin D supplementation for short periods were also assessed, and this value was incorporated in their dietary intake [24, 25].
There is no general consensus on optimal levels of 25(OH) D. For the purpose of this study, based on functionally relevant measures from several recent publications, the lower limit of a serum 25-hydroxyvitamin D replete state was taken as 20 ng/ml. The optimal level of vitamin D was taken as >30 ng/ml. The normal reference range for intact PTH was taken as 10–65 pg/ml [26, 27].
Statistical analysis
Data are reported as means ± SD. Conventional methods (mean and standard deviation (SD), ANOVA, Student’s t-test, and independent sample t-test) were used to analyze the seasonal variation in vitamin D and intact PTH levels, with the level of significance <0.05. Pearson’s correlation was calculated to assess the strength of association between 25(OH) D, iPTH, and other parameters. The software SPSS for Windows ver. 13 (SPSS Inc; Chicago, IL, USA; www.spss.com) was used for statistical analysis.
Results
The mean age of the 20 male subjects was 39 ± 10.24 years. All of the support staff had a high school education and an additional technical qualification. The entire team was subjected to psychological testing prior to selection for the expedition, and none of them suffered from depression or sleep disorders. On arrival, 8/20 (40 %) were overweight, 5/20 (25 %) were obese, 2/20 (10 %) were underweight, and only 5/20 (25 %) had a body mass index (BMI) value in the normal range. We noted a progressive rise in the mean BMI during the stay in Antarctica, attributable to the high-calorie diet and seasonal nature of work, with reduced activity during the polar winter. The average weight gain was 1.2 kg in the first quarter, 1.3 kg in the second quarter, and 0.6 kg in the third quarter.
Subjective health complaints
There were no statistically significant changes in the subjective health complaints score (SHC sum score, musculoskeletal, pseudoneurological, or gastrointestinal subscales) during the team’s sojourn in Antarctica. However, we noted an increased mean score in the musculoskeletal subscale in the high external activity period in summer and sleep disturbances soon after arrival in Antarctica. The high scores for tiredness and depression on the baseline SHC (0 months) were actually attributable to sleep disturbances in the initial phase of adaptation to a 24-h sunlit photoperiod on arrival. This complaint reduced in the second test during summer (at 3 months) (see Table 1).
Vitamin D, iPTH, and biochemical parameters
The mean serum levels of 25(OH) D, iPTH, Ca, inorganic phosphorus, and ALP are shown in Table 2 on arrival (0 month), during midwinter (at 6 months), and prior to departure (12 months). The levels of vitamin D were significantly lower at 6 months and at 12 months when compared with the baseline. The corresponding mean levels of iPTH were also significantly higher, suggesting worsening of vitamin D status in the subjects during the course of the expedition. The mean values of calcium, inorganic phosphorus, and ALP were comparable during the course of the expedition.
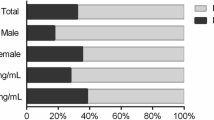
Functional status of vitamin D
Even though the 20 subjects had a normal mean serum level at baseline (30.7 ± 8.0 ng/ml), Table 3 provides information about the functional status of VDD. Nine (45 %) of the subjects had optimal vitamin D levels at 0 months. Seven (35 %) and eight (40 %) individuals had mild VDD at 6 months and 12 months, respectively, as compared with just two (10 %) on arrival, suggesting a progressive decline in vitamin D levels during the polar night, which then stabilized with the onset of the polar summer.
Four subjects developed musculoskeletal pain due to injury and were started on vitamin D supplements (400 IU/day) and calcium carbonate (equivalent to 500 mg elemental calcium) in addition to dietary advice on increasing calcium- and vitamin-D-rich foodstuffs. The number of subjects with optimal vitamin D levels >30 ng/ml declined from 9 (45 %) at baseline to 2 (10 %) at 6 months and none at 12 months, while VDD (<20 ng/ml) was seen in 2 (10 %), 10 (50 %), and 11 (55 %) at 6 and 12 months, respectively. Multivariate analysis of vitamin D levels with other biochemical parameters showed that the levels of iPTH had a significant negative correlation with serum vitamin D levels at baseline and at 6 months. No significant correlation was obtained with calcium, inorganic phosphorus, and ALP levels (see Table 4).
Dietary assessment
Total caloric and fat intake was found to be higher and dietary fiber lower when compared with the regular diet in India. Mean total calorie intake was 2,927.04 ± 472.05 kcal in summer and 2,319.51 ± 355.56 kcal in winter. Fat contributed to 34.7 % of energy intake in summer as compared to 28.3 % in winter (see Table 5). There was an increase in the mean amount of vitamin D in the diet during winter (p = 0.050), although we noted a lower fat intake in winter. We found a significant correlation for dietary vitamin D estimates and the attained serum 25(OH) D levels during summer (Pearson’s r 0.523, p = 0.043) but not during winter (Pearson’s r 0.163, p = 0.459). However, no such association was found for iPTH and dietary vitamin D. The food items rich in vitamin D available all through the year were eggs, frozen fish, milk, fortified cereals, and meat. The vegetarian subgroup had lower mean dietary vitamin D intake than the non-vegetarian group, but the difference was statistically equivalent, nor was there any difference in the attained mean serum 25(OH) D levels in the two groups.
Depression, affect, and perceived stress
The mean score on the BDI-II screen for depression was significantly higher during midwinter (4.8 ± 3.9) when compared with the baseline summer value (2.9 ± 2.1). Five subjects had a score >5 during midwinter, suggestive of minimal depression according to this scale. However, only 2/20 (10 %) of subjects met ICD criteria for minor depression. Winter was also associated with higher mean scores on the perceived stress scale which came down to the baseline again prior to departure (see Table 6). This could be correlated with a higher score on the pseudoneurology subscale of the SHC during winter. Lower vitamin D levels at 6 months did not correlate with a higher BDI score (Pearson’s r 0.069, p = 0.377), but at departure, the correlation was significant (Pearson’s r -0.523, p = 0.018). The PANAS X scores provide information about mood and affect over a 1-month period. The scores for the basic negative emotion scales (fear, sadness, and hostility) were significantly higher during midwinter (see Table 7). We found a correlation between higher PTH levels at midwinter with a higher PANAS X score at midwinter (Pearson’s r 0.623, p = 0.021) and prior to departure (Pearson’s r 0.532, p = 0.045). We also found that for subjects with a vitamin D concentration less than 9 ng/ml (lower limit of reference range), the mean PANAS X score during summer and midwinter was significantly higher than in the group with vitamin D >9 ng/ml, 9 (p = 0.000).
Total global solar radiation
Total global solar radiation over Maitri (70°45′57″ S, 11°44′09″ E) was continuously recorded using a thermoelectric pyranometer sensor (Global Pyranometer, IMD, Pune SN 45-77) installed on the roof of the station and radiation data logger (9210 X Lite, Sutron) in the IMD laboratory. The total global solar radiation was found maximum in the month of November, December, and January due to periods of cloud-free sky, high solar elevation, and continuous polar day. From February, as the solar elevation and duration of sunshine started reducing, total solar radiation also reduced rapidly and became almost zero by the beginning of the long polar night in May. Solar radiation again started to increase from the end of the polar night, i.e., the last week of July, and increased rapidly.
Discussion
Antarctica has exposed human subjects to a challenging external environment: a long polar night with reduced physical activity, polar summer with no dark photoperiod, low temperatures, and seasonally variant electromagnetic radiation exposure. While the polar environment has changed little, modern research bases are now well equipped to deal with the geographic and social isolation. Artificial illumination, central heating, motorized vehicles, automated machinery, and better communication facilities have completely changed living conditions of polar residents in Antarctic research stations. This has greatly changed the psychological factors, energy dynamics, physical activity, and stress patterns of the lifestyle at these research bases. The sense of isolation in winter has been greatly reduced with the availability of internet access, news updates, and satellite television. So, psychological research conducted in modern scientific polar stations has to be interpreted accordingly, especially in context with older studies [28]. We did note higher depression scores during midwinter, suggesting that a few members were affected by the “over-wintering” syndrome, and this affected the mean group scores. The main causes of depression in these subjects were stressful events such as health problems, breakdown of machinery requiring extensive repair, snowstorm duties, and work-related discord. This differs with findings in other studies where depression was attributed to sleep disorders and musculoskeletal fatigue.
Vitamin D metabolism in Antarctica
Few studies have been done on the impact of prolonged Antarctic residence on vitamin D status [13, 29–32]. The effect of over-wintering and the consequent bearing on bone health and behavior have not been studied in Indian expedition members over a long-term period. Factors which are known to affect vitamin D metabolism include race, dietary vitamin D intake, sun exposure, skin pigmentation, adiposity, age, physical activity, etc. Even when all of these factors are taken into account, it is still difficult to assess and explain the individual variation in vitamin D levels. Keeping this in mind, the clinical and biochemical consequences at any given 25(OH) D level cannot be accurately predicted in a subject due to variations in responsiveness of the vitamin D receptor type, duration of VDD, and individual calcium and vitamin D requirements [6, 26].
Another confounding factor in circumpolar regions is the degree of solar radiation and exposure times. We measured the total global solar radiation over the station which fell to near zero during the polar night. Besides, even during adequate sunlight exposure during summer, subjects wear bulky polar gear covering nearly all exposed skin. Gloves, protective goggles, and balaclava caps are worn in addition to multilayer thermal gear, which grossly limits ultraviolet (UV) exposure and endogenous vitamin D production.
In a French study, levels of 25(OH) D and 1, 25 dihydroxy D significantly decreased in 15 Caucasian subjects during the expedition, minimum levels being observed 10 months after their departure from France. Intact PTH concentrations did not change throughout this study, but osteocalcin levels were found to be higher at the end of the sojourn than before departure, which could argue for the existence of bone remodeling changes [29]. In another study on 17 wintering team members from Argentina, vitamin D levels decreased in autumn and winter (nadir in July) and recovered the initial levels by the end of the sojourn. This correlated with UV radiation levels and would suggest that endogenous production of 25(OH) D ceases for at least the duration of the Antarctic winter [13]. An Australian study on a group of 19 men showed a drop in concentration of 25(OH) D in the dark winter period. In contrast with other studies, however, they found no significant alterations in 1, 25 dihydroxy D or calcium concentrations over the same period. This led them to conclude that provided that individuals with pre-existing vitamin D deficiencies are detected before departure for Antarctica and missions are limited in duration, clinical deficiency is unlikely to occur [30] (see Table 8). Later, a large prospective Australian study on 120 Antarctic members showed vitamin D insufficiency (<50 nmol/l) in 85 % of subjects by 6 months associated with a decrease in serum calcium and increase in iPTH. They concluded that vitamin D supplementation will thus be necessary in such expeditions [31]. An American 5-month, prospective, randomized control study on 55 subjects showed improvement in vitamin D levels with supplementary doses of vitamin D [14].
A recent study analyzed the relationship between serum 25(OH) D levels and total intake of vitamin during the winter season at high latitudes above 49.5° N or in the Antarctic in each of three age groups—children and adolescents, young and middle-aged adults, and older adults. They found no effect of age in the response of serum 25(OH) D levels to total intake of dietary vitamin D. There also appears to be a non-linear response of serum vitamin D levels to supplementary doses of the vitamin in addition to dietary intake, especially in areas with minimal UVB exposure. These regression analysis data are important for two reasons. It is relevant to make recommendations for the daily allowance (RDA) to achieve a serum 25(OH) D level consistent with optimal metabolism. Secondly, it eliminates the confounding role of endogenous vitamin D production, as UVB exposure is minimal in high-latitude regions. Similar intake of vitamin D was found to achieve comparable serum levels across all age groups [33, 34]. Based on these findings and the data from our study, it is possible to recommend vitamin D supplementation during the polar winter in future expeditions.
Psychological changes in Antarctica
Antarctica has been used as a psychological laboratory ever since the first polar expeditions of Shackleton, Scott, and Amundsen. The “winter-over” syndrome includes insomnia, irritability, depression, and social withdrawal. This can be attributed to changes in the circadian rhythm and the altered photoperiod and only rarely requires intervention or pharmacological therapy. It has been estimated that the prevalence of psychiatric illness is about 5 % of personnel at Antarctic stations. The most common ailments reported are mood and sleep disorders [12, 35]. Another condition described is the polar T3 syndrome, which is due to seasonal alteration of the hypothalamic pituitary thyroid axis in response to prolonged polar residence. In this condition, there is increased pituitary release of thyroid-stimulating hormone (TSH) in response to intravenous thyrotropin-releasing hormone and normal free T4 and unstimulated TSH levels. The production and clearance of T3 are increased. It allows for an increased calorie intake with a minimal change in body weight due to altered energy metabolism. This may be considered an adaptive response to the cold external environment [36]. Another overlapping condition is the presence of subsyndromal seasonal affective disorder (SAD) in high-latitude areas. Large population-based surveys in the Arctic have estimated a prevalence rate of 9 % for SAD. Research in large populations in the Arctic has established this condition to have a prevalence rate of about 9 % [37]. Since the Antarctic does not have a permanent population, it is difficult to estimate long-term consequences of this disorder as most over-wintering teams spend 12–14 months on an average at any station. Secondly, the number of team members who over-winter is kept to a bare minimum. Therefore, pooling of data is necessary to draw any conclusions regarding the multifactorial causation of psychiatric illness in such expeditions. Parallels have been drawn between wintering expeditions in the Antarctic and space missions. The individuals chosen for these expeditions have already undergone extensive psychological testing and endurance training prior to selection. Hence, any disturbance in the mental health of such a highly skilled and motivated team is significant [38].
Limitations of this study and future research
Most wintering Antarctic expeditions are stationed for a period of 12–14 months. This is a short period to assess changes in bone mineral metabolism and predict future bone health outcomes. Secondly, resources for extensive testing are limited or unavailable, and long-term follow-up is difficult. Thirdly, the average strength of the team is between 15 and 30 members, just sufficient for maintaining the station and keeping the scientific experiments running during the polar winter. Thus, the number of subjects in polar expeditions restricts the effect size and therefore the power of the study. The difference in racial, genetic, and environmental factors hinders pooling of data, and results have to be interpreted carefully. We were unable to carry out bone densitometry tests, which is planned for future research. Long-term health consequences of the Antarctic sojourn will be assessed on longitudinal follow-up.
Conclusions
Vitamin D levels were found to decrease in the winter months, which partially recovered by the end of the expedition. Seasonal variations in mood were noted in the 20 over-wintering subjects, and there were significant increases in the midwinter stress and depression scores. There was a corresponding decrease in the serum 25(OH) D levels and increase in iPTH level during midwinter, which correlated with decreased solar radiation during the polar night. In view of the fall in vitamin D levels during midwinter, there is a worsening of vitamin D status in over-wintering teams due to poor endogenous production at high latitudes and insufficient dietary intake. Therefore, screening for deficiency at baseline and routine vitamin D supplementation may be recommended on the basis of the recent research. While fluctuations in vitamin D and iPTH levels may be associated with the observed subsyndromal SAD, a causal role can only be hypothesized. The role of the social environment and team structure in addition to the external environment and physical factors in determining mental health at these stations cannot be emphasized enough. We did not find any alteration in serum calcium, phosphate, or alkaline phosphatase levels over 1 year, and the long-term effect on bone mass in these subjects remains to be seen.
References
Marwaha RK, Tandon N, Garg MK, Kanwar R, Narang A, Sastry A, Saberwal A, Bandra K (2011) Vitamin D status in healthy Indians aged 50 years and above. J Assoc Physicians India 59:706–709
Harinarayan CV, Joshi SR (2009) Vitamin D status in India—its implications and remedial measures. J Assoc Phys India 57:40–48
Marwaha RK, Sripathy G (2008) Vitamin D and bone mineral density of healthy school children in northern India. Indian J Med Res 127:239–244
Ramakrishnan S, Bhansali A, Bhadada SK, Sharma R, Walia R, Ravikiran M, Shanmugasundar G, Ravikumar P (2010) Vitamin D status and its seasonal variability in young healthy adults in an Asian Indian urban population. Endocr Pract 14:1–26
Ganji V, Milone C, Cody MM, McCarty F, Wang YT (2010) Serum vitamin D concentrations are related to depression in young adult US population: the Third National Health and Nutrition Examination Survey. Int Arch Med 11(3):29
Holick MF (2004) Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr 79:362–371
Thacher TD, Clarke BL (2011) Vitamin D insufficiency. Mayo Clin Proc 86(1):50–60
Oudshoorn C, Mattace-Raso FU, van der Velde N, Colin EM, van der Cammen TJ (2008) Higher serum vitamin D3 levels are associated with better cognitive test performance in patients with Alzheimer's disease. Dement Geriatr Cogn Disord 25:539–543
Pruefer K, Veenstra T, Jirikowski G, Kumar R (1999) Distribution of 1,25-dihydroxyvitamin D3 receptor immunoreactivity in the rat brain and spinal cord. J Chem Neuroanat 16:135–145
Eyles D, Smith S, Kinobe R, Hewison M, McGrath J (2005) Distribution of the vitamin D receptor and 1 alpha-hydroxylase in human brain. J Chem Neuroana 29:21–30
Hoogendijk WJ, Lips P, Dik MG, Deeg DJ, Beekman AT, Penninx BW (2008) Depression is associated with decreased 25-hydroxyvitamin D and increased parathyroid hormone levels in older adults. Arch Gen Psychiatry 65(5):508–512
Palinkas LA, Suedfeld P (2008) Psychological effects of polar expeditions. Lancet 371(9607):153–163
Oliveri B, Zeni S, Lorenzetti MP, Aguilar G, Mautalen C (1999) Effect of one year residence in Antarctica on bone mineral metabolism and body composition. Eur J Clin Nutr 53(2):88–91
Smith SM, Gardner KK, Locke J, Zwart SR (2009) Vitamin D supplementation during Antarctic winter. Am J Clin Nutr 89(4):1092–1098, Epub 2009 Feb 18
Heaney RP (2008) Vitamin D, in health and disease. Clin J Am Soc Nephrol 3:1535–1541
Lips P (2001) Vitamin D, deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev 22(4):477–501
Aloia JF, Patel M, Dimaano R et al (2008) Vitamin D intake to attain a desired serum 25-hydroxyvitamin D concentration. Am J Clin Nutr 87:1952–1958
Eriksen HR, Ihlebaek C, Ursin H (1999) A scoring system for subjective health complaints (SHC). Scand J Public Health 27(1):63–72
Watson D, Clark LA, Tellegen A (1988) Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 54(6):1063–1070
Carney CE, Ulmer C, Edinger JD, Krystal AD, Knauss F (2009) Assessing depression symptoms in those with insomnia: an examination of the Beck Depression Inventory second edition (BDI-II). J Psychiatr Res 43(5):576–582
Cohen S, Karmarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24(4):385–396
Diet History Questionnaire (2010) National Cancer Institute, available from http://riskfactor.cancer.gov/DHQ. Accessed 14 Dec 2010
Blalock SJ, Norton LL, Patel RA, Cabral K, Thomas CL (2003) Development and assessment of a short instrument for assessing dietary intakes of calcium and vitamin D. J Am Pharm Assoc 43(6):685–693
Gopalan C, Ramshastri BV, Balasubramanian SC (1989) Nutritive value of Indian foods. National Institute of Nutrition, Hyderabad
Bharathi AV, Kurpad AV, Thomas T et al (2008) Development of food frequency questionnaires and a nutrient database for the prospective Urban and Rural epidemiological (PURE) pilot study in South India: methodological issues. Asia Pac J Clin Nutr 17(1):178–185
Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B (2006) Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr 84:18–28
Dawson-Hughes B, Heaney RP, Holick MF, Lips P, Meunier PJ, Vieth R (2005) Estimates of optimal vitamin D status. Osteoporos Int 16:713–716
Palinkas LA, Johnson JC, Boster JS, Rakusa-Suszczewski S, Klopov VP, Fu XQ, Sachdeva U (2004) Cross-cultural differences in psychosocial adaptation to isolated and confined environments. Aviat Space Environ Med 75(11):973–980
Zérath E, Holy X, Gaud R, Schmitt D (1999) Decreased serum levels of 1,25-(OH)2 vitamin D during 1 year of sunlight deprivation in the Antarctic. Eur J Appl Physiol Occup Physiol 79(2):141–147
Pitson GA, Lugg DJ, Roy CR (1996) Effect of seasonal ultraviolet radiation fluctuations on vitamin D homeostasis during an Antarctic expedition. Eur J Appl Physiol 72(3):231–234
Iuliano-Burns, Wang XF, Ayton J, Jones G, Seeman E (2009) Skeletal and hormonal responses to sunlight deprivation in Antarctic expeditioners. Osteoporos Int 20(9):1523–1528
Yonei T, Hagino H, Katagiri H, Kishimoto H (1999) Bone metabolic changes in Antarctic wintering team members. Bone 2492:145–150
Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ (2003) Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr 77(1):204–210
Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium; Ross AC, Taylor CL, Yaktine AL, et al., editors. Dietary reference intakes for calcium and vitamin D. Washington: National Academies Press (US); 2011. 5, Dietary reference intakes for adequacy: calcium and vitamin D. Available from: http://www.ncbi.nlm.nih.gov/books/NBK56056/
Palinkas LA, Houseal M, Rosenthal NE (1996) Subsyndromal seasonal affective disorder in Antarctica. J Nerv Ment Dis 184(9):530–534
Reed HL, Reedy KR, Palinkas LA, Van Do N, Finney NS, Case HS, LeMar HJ, Wright J, Thomas J (2001) Impairment in cognitive and exercise performance during prolonged Antarctic residence: effect of thyroxine supplementation in the polar triiodothyronine syndrome. J Clin Endocrinol Metab 86(1):110–116
Kegel M, Dam H, Ali F, Bjerregaard P (2009) The prevalence of seasonal affective disorder (SAD) in Greenland is related to latitude. Nord J Psychiatry 63(4):331–335
Premkumar M, Sable T, Dhanwal D, Dewan R (2013) Circadian levels of serum melatonin and cortisol in relation to changes in mood sleep, and neurocognitive performance, spanning a year of residence in Antarctica. Neurosci J 2013. doi:10.1155/2013/254090, Article ID 254090, 10 pages
Acknowledgments
We would like to thank the team members of the 30th Indian Scientific Expedition to Antarctica. Ms. Nemisha Dawra, University of Massachusetts Medical School, Boston provided invaluable technical assistance for sample preparation and manuscript editing. Mr. Shankar Prasad and Mr. Ashok Kuthwad of the Indian Meteorological Department provided data on solar radiation over Maitri. Mr. Prabhat Sahoo of the Snow and Avalanche Study Establishment, DRDO, Chandigrah and Mr Roy, Nuclear Medicine Laboratory, Maulana Azad Medical College, New Delhi provided technical assistance. The project was supported by an institutional grant by the National Centre for Antarctic and Ocean Research (NCAOR), Ministry of Earth Sciences, Headland Sada, Goa, India (NCAOR 02/2013).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Premkumar, M., Sable, T., Dhanwal, D. et al. Vitamin D homeostasis, bone mineral metabolism, and seasonal affective disorder during 1 year of Antarctic residence. Arch Osteoporos 8, 129 (2013). https://doi.org/10.1007/s11657-013-0129-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-013-0129-0