Abstract
Background
Glucagon-like peptide-1 receptor agonists (GLP-1RA) have cardiovascular benefits in type 2 diabetes, but none of the cardiovascular trials studied atrial fibrillation/atrial flutter (AF) as a primary endpoint. Data from post-marketing surveillance studies remains sparse.
Objective
To examine the real-world risk of AF comparing GLP-1RA with other non-insulin glucose-lowering agents.
Design
Cohort study using de-identified electronic health record data from the Optum Labs Data Warehouse.
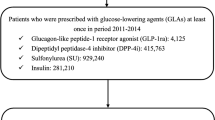
Participants
Adult patients with diabetes who were newly prescribed add-on non-insulin glucose-lowering agents and were on metformin between 2005-2020.
Exposures
New users of GLP-1RA were separately compared with new users of dipeptidyl peptidase-4 inhibitors (DPP4i) and sodium-glucose cotransporter 2 inhibitors (SGLT2i), using 1:1 propensity score matching to adjust for differences in patient characteristics.
Main Measures
The primary outcome was incident AF, defined and captured by diagnosis code for AF. Incidence rate difference (IRD) and hazard ratio (HR) were estimated in the matched cohorts.
Key Results
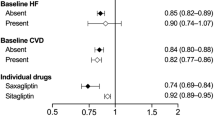
In the matched cohort of 14,566 pairs of GLP-1RA and DPP4i followed for a median of 3.8 years, GLP-1RA use was associated with a lower risk of AF (IRD, -1.0; 95% CI, -1.8 to -0.2 per 1000 person-years; HR, 0.82; 95% CI, 0.70 to 0.96). In the matched cohort of 9,424 pairs of patients on GLP-1RA and SGLT2i with a median follow-up of 2.9 years, there was no difference in the risk for AF (IRD, 0.4; 95% CI -0.7 to 1.5 per 1000 person-years; HR, 1.12; 95% CI, 0.89 to 1.42).
Conclusions
In this real-word study, GLP-1RA was associated with a lower risk of AF compared with DPP4i, but no difference compared with SGLT2i, suggesting that cardiovascular benefits of GLP-1RA use may extend to prevention for AF in patients with diabetes. Our findings call for future randomized controlled trials to focus on the effects of GLP-1RA on AF prevention.


Similar content being viewed by others
REFERENCES
Centers for Disease Control and Prevention. National Diabetes Statistics Report website. Accessed January 4, 2023. https://www.cdc.gov/diabetes/data/statistics-report/index.html
Dal Canto E, Ceriello A, Rydén L, et al. Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol. 2019;26(2_suppl):25-32. https://doi.org/10.1177/2047487319878371
Huxley RR, Filion KB, Konety S, Alonso A. Meta-analysis of Cohort and Case-Control Studies of Type-2 Diabetes Mellitus and Risk of Atrial Fibrillation. Am J Cardiol. 2011;108(1):56-62. https://doi.org/10.1016/j.amjcard.2011.03.004
Bell DSH, Goncalves E. Atrial fibrillation and type 2 diabetes: Prevalence, etiology, pathophysiology and effect of anti-diabetic therapies. Diabetes, Obesity and Metabolism. 2019;21(2):210-217. https://doi.org/10.1111/dom.13512
Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271(11):840-844.
Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics—2023 Update: A Report From the American Heart Association. Circulation. 2023;147(8):e93-e621. https://doi.org/10.1161/CIR.0000000000001123
Okunrintemi V, Mishriky BM, Powell JR, Cummings DM. Sodium-glucose co-transporter-2 inhibitors and atrial fibrillation in the cardiovascular and renal outcome trials. Diabetes, Obesity and Metabolism. 2021;23(1):276-280. https://doi.org/10.1111/dom.14211
Lyu B, Sang Y, Selvin E, et al. Pharmacologic Treatment of Type 2 Diabetes in the U.S., Sweden, and Israel. Diabetes Care. 2022;45(12):2926-2934. https://doi.org/10.2337/dc22-1253
ElSayed NA, Aleppo G, Aroda VR, et al. Summary of Revisions: Standards of Care in Diabetes—2023. Diabetes Care. 2022;46(Supplement_1):S5-S9. https://doi.org/10.2337/dc23-Srev
ElSayed NA, Aleppo G, Aroda VR, et al. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes—2023. Diabetes Care. 2022;46(Supplement_1):S140-S157. https://doi.org/10.2337/dc23-S009
Sharma A, Verma S. Mechanisms by Which Glucagon-Like-Peptide-1 Receptor Agonists and Sodium-Glucose Cotransporter-2 Inhibitors Reduce Cardiovascular Risk in Adults With Type 2 Diabetes Mellitus. Canadian Journal of Diabetes. 2020;44(1):93-102. https://doi.org/10.1016/j.jcjd.2019.09.003
Vergès B, Aboyans V, Angoulvant D, et al. Protection against stroke with glucagon-like peptide-1 receptor agonists: a comprehensive review of potential mechanisms. Cardiovasc Diabetol. 2022;21(1):242. https://doi.org/10.1186/s12933-022-01686-3
Li W, Chen X, Xie X, et al. Comparison of Sodium–Glucose Cotransporter 2 Inhibitors and Glucagon-like Peptide Receptor Agonists for Atrial Fibrillation in Type 2 Diabetes Mellitus: Systematic Review With Network Meta-analysis of Randomized Controlled Trials. Journal of Cardiovascular Pharmacology. 2022;79(3):281-288. https://doi.org/10.1097/FJC.0000000000001197
Liu Z, Bian N, Wu S, et al. A meta-analysis evaluating indirectly GLP-1 receptor agonists and arrhythmias in patients with type 2 diabetes and myocardial infarction. Front Cardiovasc Med. 2022;9:1019120. https://doi.org/10.3389/fcvm.2022.1019120
Optum Labs. Optum Labs and Optum Labs Data Warehouse (OLDW) Descriptions and Citation. PDF. March 2023. Reproduced with permission from Optum Labs.
Zheng RJ, Wang Y, Tang JN, Duan JY, Yuan MY, Zhang JY. Association of SGLT2 Inhibitors With Risk of Atrial Fibrillation and Stroke in Patients With and Without Type 2 Diabetes: A Systemic Review and Meta-Analysis of Randomized Controlled Trials. J Cardiovasc Pharmacol. 2022;79(2):e145-e152. https://doi.org/10.1097/FJC.0000000000001183
Patoulias DI, Boulmpou A, Teperikidis E, et al. Cardiovascular efficacy and safety of dipeptidyl peptidase-4 inhibitors: A meta-analysis of cardiovascular outcome trials. World Journal of Cardiology. 2021;13(10):585-592. https://doi.org/10.4330/wjc.v13.i10.585
Monami M, Genovese S, Mannucci E. Cardiovascular safety of sulfonylureas: a meta-analysis of randomized clinical trials. Diabetes Obes Metab. 2013;15(10):938-953. https://doi.org/10.1111/dom.12116
Zhou J, Zhang G, Chang C, et al. Metformin versus sulphonylureas for new onset atrial fibrillation and stroke in type 2 diabetes mellitus: a population-based study. Acta Diabetol. 2022;59(5):697-709. https://doi.org/10.1007/s00592-021-01841-4
Jensen PN, Johnson K, Floyd J, Heckbert SR, Carnahan R, Dublin S. A systematic review of validated methods for identifying atrial fibrillation using administrative data. Pharmacoepidemiology and Drug Safety. 2012;21(S1):141-147. https://doi.org/10.1002/pds.2317
Chamberlain AM, Roger VL, Noseworthy PA, et al. Identification of Incident Atrial Fibrillation From Electronic Medical Records. Journal of the American Heart Association. 2022;11(7):e023237. https://doi.org/10.1161/JAHA.121.023237
Inker LA, Eneanya ND, Coresh J, et al. New Creatinine- and Cystatin C–Based Equations to Estimate GFR without Race. N Engl J Med. 2021;385:1737-1749. https://doi.org/10.1056/NEJMoa2102953
Quan H, Sundararajan V, Halfon P, et al. Coding Algorithms for Defining Comorbidities in ICD-9-CM and ICD-10 Administrative Data. Medical Care. 2005;43(11):1130-1139.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology. 1992;45(6):613-619. https://doi.org/10.1016/0895-4356(92)90133-8
Zheng J, Heidenreich PA, Kohsaka S, Fearon WF, Sandhu AT. Variability in Coronary Artery Disease Testing for Patients With New-Onset Heart Failure. Journal of the American College of Cardiology. 2022;79(9):849-860. https://doi.org/10.1016/j.jacc.2021.11.061
Austin PC. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behavioral Research. 2011;46(3):399-424. https://doi.org/10.1080/00273171.2011.568786
Webster-Clark M, Stürmer T, Wang T, et al. Using propensity scores to estimate effects of treatment initiation decisions: State of the science. Stat Med. 2021;40(7):1718-1735. https://doi.org/10.1002/sim.8866
Zhu J, Yu X, Zheng Y, et al. Association of glucose-lowering medications with cardiovascular outcomes: an umbrella review and evidence map. The Lancet Diabetes & Endocrinology. 2020;8(3):192-205. https://doi.org/10.1016/S2213-8587(19)30422-X
Monami M, Nreu B, Scatena A, et al. Glucagon-like peptide-1 receptor agonists and atrial fibrillation: a systematic review and meta-analysis of randomised controlled trials. J Endocrinol Invest. 2017;40(11):1251-1258. https://doi.org/10.1007/s40618-017-0698-7
Nreu B, Dicembrini I, Tinti F, Sesti G, Mannucci E, Monami M. Major cardiovascular events, heart failure, and atrial fibrillation in patients treated with glucagon-like peptide-1 receptor agonists: An updated meta-analysis of randomized controlled trials. Nutrition, Metabolism and Cardiovascular Diseases. 2020;30(7):1106-1114. https://doi.org/10.1016/j.numecd.2020.03.013
Hamedi Z, Mishriky BM, Okunrintemi V, Powell JR, Cummings DM. GLP-1 RA and atrial fibrillation in the cardiovascular outcome trials. Diabetes/Metabolism Research and Reviews. 2021;37(5):e3436. https://doi.org/10.1002/dmrr.3436
Boulmpou A, Patoulias D, Papadopoulos CE, Teperikidis E, Doumas M, Vassilikos V. Meta-analysis of cardiovascular outcome trials assessing the impact of glucagon-like peptide-1 receptor agonists on major cardiac arrhythmias. Acta Cardiologica. 2022;0(0):1-6. https://doi.org/10.1080/00015385.2022.2087839
Wei J, Wang R, Ye H, Wang Y, Wang L, Zhang X. Effects of GLP-1 receptor agonists on arrhythmias and its subtypes in patients with type 2 diabetes: A systematic review and meta-analysis. Front Endocrinol (Lausanne). 2022;13:910256. https://doi.org/10.3389/fendo.2022.910256
Yin DG, Ding LL, Zhou HR, Qiu M, Duan XY. Comprehensive analysis of the safety of semaglutide in type 2 diabetes: a meta-analysis of the SUSTAIN and PIONEER trials. Endocr J. 2021;68(6):739-742. https://doi.org/10.1507/endocrj.EJ21-0129
Shi W, Zhang W, Zhang D, et al. Comparison of the effect of glucose-lowering agents on the risk of atrial fibrillation: A network meta-analysis. Heart Rhythm. 2021;18(7):1090-1096. https://doi.org/10.1016/j.hrthm.2021.03.007
Chan YH, Chao TF, Chen SW, et al. The risk of incident atrial fibrillation in patients with type 2 diabetes treated with sodium glucose cotransporter-2 inhibitors, glucagon-like peptide-1 receptor agonists, and dipeptidyl peptidase-4 inhibitors: a nationwide cohort study. Cardiovasc Diabetol. 2022;21(1):118. https://doi.org/10.1186/s12933-022-01549-x
Hsiao FC, Yen KC, Chao TF, Chen SW, Chan YH, Chu PH. New-Onset Atrial Fibrillation in Patients With Type 2 Diabetes Treated With Novel Glucose-Lowering Therapies. J Clin Endocrinol Metab. 2022;107(9):2493-2499. https://doi.org/10.1210/clinem/dgac402
Lui DTW, Tang EHM, Wu T, et al. Risks of stroke, its subtypes and atrial fibrillation associated with glucagon-like peptide 1 receptor agonists versus sodium-glucose cotransporter 2 inhibitors: a real-world population-based cohort study in Hong Kong. Cardiovascular Diabetology. 2023;22(1):40. https://doi.org/10.1186/s12933-023-01772-0
Zhuo M, D’Andrea E, Paik JM, et al. Association of Sodium-Glucose Cotransporter-2 Inhibitors With Incident Atrial Fibrillation in Older Adults With Type 2 Diabetes. JAMA Netw Open. 2022;5(10):e2235995. https://doi.org/10.1001/jamanetworkopen.2022.35995
Huxley RR, Alonso A, Lopez FL, et al. Type 2 diabetes, glucose homeostasis and incident atrial fibrillation: the Atherosclerosis Risk in Communities Study. Heart. 2012;98(2):133-138. https://doi.org/10.1136/heartjnl-2011-300503
Seyed Ahmadi S, Svensson AM, Pivodic A, Rosengren A, Lind M. Risk of atrial fibrillation in persons with type 2 diabetes and the excess risk in relation to glycaemic control and renal function: a Swedish cohort study. Cardiovasc Diabetol. 2020;19(1):1-12. https://doi.org/10.1186/s12933-019-0983-1
Engström A, Wintzell V, Melbye M, et al. Sodium-Glucose Cotransporter 2 Inhibitor Treatment and Risk of Atrial Fibrillation: Scandinavian Cohort Study. Diabetes Care. 2023;46(2):351-360. https://doi.org/10.2337/dc22-0714
Funding
Research reported in this publication was supported by R01 DK115534 and K24 HL155861 (PI: Dr. Grams), and K01 DK121825 (PI: Dr. Shin) from the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. The funding sources had no role in the design and conduct of the study, analysis or interpretation of the data, and preparation or final approval of the manuscript before publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest:
A. Chang reports having consultancy agreements with Amgen, Novartis, and Reata; reports receiving research funding from a Novo Nordisk Investigator Sponsored Study; reports having an advisory or leadership role with Reata, Relypsa; and reports having other interests or relationships with National Kidney Foundation grant support and the NKF Patient Network. E. Selvin reports receiving research support from the Foundation for the National Institutes of Health and the National Institutes of Health; reports receiving royalty payments from Wolters Kluwer for chapters and laboratory monographs in UpToDate on measurements of glycemic control and screening tests for type 2 diabetes; and reports having an advisory or leadership role with Diabetes Care and Diabetologia Editorial Board, the American Diabetes Association, and the American Heart Association. L. Inker reports having consultancy agreements with Diamtrix; reports receiving research funding to the institution for research and contracts with the National Institutes of Health, National Kidney Foundation, Omeros, Reata Pharmaceuticals; reports having consulting agreements to her institution with Omeros and Tricida Inc.; reports having an advisory or leadership role with the Alport Syndrome Foundation; and reports having other interests or relationships as a member of the American Society of Nephrology, the National Kidney Disease Education Program, and the National Kidney Foundation. M. Grams reports having an advisory or leadership role with AJKD, CJASN, JASN Editorial Board, KDIGO Executive Committee, NKF Scientific Advisory Board, and the USRDS Scientific Advisory Board; and reports having other interests or relationships with grant funding from NKF, which receives funding from multiple pharmaceutical companies, and grant funding from the National Institutes of Health. J. Shin reports receiving research funding from Merck and the National Institutes of Health. The remaining authors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, Y., Boyle, T.A., Lyu, B. et al. Glucagon-like peptide-1 receptor agonists and the risk of atrial fibrillation in adults with diabetes: a real-world study. J GEN INTERN MED (2024). https://doi.org/10.1007/s11606-023-08589-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11606-023-08589-3