Abstract
Background
Guidelines recommend shared decision-making (SDM) around mammography screening for women ≥ 75 years old.
Objective
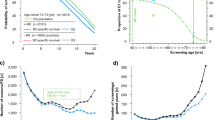
To use microsimulation modeling to estimate the lifetime benefits and harms of screening women aged 75, 80, and 85 years based on their individual risk factors (family history, breast density, prior biopsy) and comorbidity level to support SDM in clinical practice.
Design, Setting, and Participants
We adapted two established Cancer Intervention and Surveillance Modeling Network (CISNET) models to evaluate the remaining lifetime benefits and harms of screening U.S. women born in 1940, at decision ages 75, 80, and 85 years considering their individual risk factors and comorbidity levels. Results were summarized for average- and higher-risk women (defined as having breast cancer family history, heterogeneously dense breasts, and no prior biopsy, 5% of the population).
Main Outcomes and Measures
Remaining lifetime breast cancers detected, deaths (breast cancer/other causes), false positives, and overdiagnoses for average- and higher-risk women by age and comorbidity level for screening (one or five screens) vs. no screening per 1000 women.
Results
Compared to stopping, one additional screen at 75 years old resulted in six and eight more breast cancers detected (10% overdiagnoses), one and two fewer breast cancer deaths, and 52 and 59 false positives per 1000 average- and higher-risk women without comorbidities, respectively. Five additional screens over 10 years led to 23 and 31 additional breast cancer cases (29–31% overdiagnoses), four and 15 breast cancer deaths avoided, and 238 and 268 false positives per 1000 average- and higher-risk screened women without comorbidities, respectively. Screening women at older ages (80 and 85 years old) and high comorbidity levels led to fewer breast cancer deaths and a higher percentage of overdiagnoses.
Conclusions
Simulation models show that continuing screening in women ≥ 75 years old results in fewer breast cancer deaths but more false positive tests and overdiagnoses. Together, clinicians and 75 + women may use model output to weigh the benefits and harms of continued screening.
Similar content being viewed by others
Data Availability
Additional data available upon request.
References
Lee SJ, Boscardin WJ, Stijacic-Cenzer I, Conell-Price J, O’Brien S, Walter LC. Time lag to benefit after screening for breast and colorectal cancer: meta-analysis of survival data from the United States, Sweden, United Kingdom, and Denmark. BMJ. 2013;346:e8441. https://doi.org/10.1136/bmj.e8441bmj.e8441 [pii]
Tabár L, Dean PB, Chen TH, et al. The incidence of fatal breast cancer measures the increased effectiveness of therapy in women participating in mammography screening. Cancer. 2019;125(4):515-523. https://doi.org/10.1002/cncr.31840
Holmberg L, Duffy SW, Yen AMF, et al. Differences in Endpoints between the Swedish W-E (Two County) Trial of Mammographic Screening and the Swedish Overview: Methodological Consequences. J Med Screen. 2009;16(2):73-80. https://doi.org/10.1258/jms.2009.008103
McCarthy EP, Burns RB, Freund KM, et al. Mammography use, breast cancer stage at diagnosis, and survival among older women. J Am Geriatr Soc. 2000;48(10):1226-33. https://doi.org/10.1111/j.1532-5415.2000.tb02595.x
García-Albéniz X, Hernán MA, Logan RW, Price M, Armstrong K, Hsu J. Continuation of Annual Screening Mammography and Breast Cancer Mortality in Women Older Than 70 Years. Ann Intern Med. 2020;172(6):381-389. https://doi.org/10.7326/m18-1199
Yasmeen S, Hubbard RA, Romano PS, et al. Risk of advanced-stage breast cancer among older women with comorbidities. Cancer Epidemiol Biomarkers Prev. 2012;21(9):1510-9. https://doi.org/10.1158/1055-9965.Epi-12-0320
Braithwaite D, Zhu W, Hubbard RA, et al. Screening outcomes in older US women undergoing multiple mammograms in community practice: does interval, age, or comorbidity score affect tumor characteristics or false positive rates? J Natl Cancer Inst. 2013;105(5):334-41. https://doi.org/10.1093/jnci/djs645
Kerlikowske K, Hubbard RA, Miglioretti DL, et al. Comparative effectiveness of digital versus film-screen mammography in community practice in the United States: a cohort study. Ann Intern Med. 2011;155(8):493-502. https://doi.org/10.7326/0003-4819-155-8-201110180-00005
Walter LC, Schonberg MA. Screening mammography in older women: a review. JAMA. 2014;311(13):1336-47. https://doi.org/10.1001/jama.2014.2834
Depboylu B. Treatment and patient related quality of life issues in elderly and very elderly breast cancer patients. Transl Cancer Res. 2020;9(Suppl 1):S146-s153. https://doi.org/10.21037/tcr.2019.07.08
Richman IB, Long JB, Soulos PR, Wang SY, Gross CP. Estimating Breast Cancer Overdiagnosis After Screening Mammography Among Older Women in the United States. Ann Intern Med. 2023; https://doi.org/10.7326/m23-0133
Tyrer J, Duffy SW, Cuzick J. A breast cancer prediction model incorporating familial and personal risk factors. Stat Med. 2004;23(7):1111-1130.
Colditz GA, Rosner BA, Chen WY, Holmes MD, Hankinson SE. Risk Factors for Breast Cancer According to Estrogen and Progesterone Receptor Status. JNCI: J Natl Cancer Inst. 2004;96(3):218-228. https://doi.org/10.1093/jnci/djh025
Hedenfalk I, Duggan D, Chen Y, et al. Gene-Expression Profiles in Hereditary Breast Cancer. N Engl J Med. 2001;344(8):539-548. https://doi.org/10.1056/nejm200102223440801
Nelson HD, Fu R, Cantor A, Pappas M, Daeges M, Humphrey L. Effectiveness of Breast Cancer Screening: Systematic Review and Meta-analysis to Update the 2009 U.S. Preventive Services Task Force Recommendation. Ann Intern Med. 2016;164(4):244-55. https://doi.org/10.7326/m15-0969
US Preventive Services Task Force, Davidson KW, Mangione CM et al. Collaboration and Shared Decision-Making Between Patients and Clinicians in Preventive Health Care Decisions and US Preventive Services Task Force Recommendations. JAMA. 2022;327(12):1171-1176. https://doi.org/10.1001/jama.2022.3267
Oeffinger KC, Fontham ET, Etzioni R, et al. Breast Cancer Screening for Women at Average Risk: 2015 Guideline Update From the American Cancer Society. JAMA 2015;314(15):1599-614. https://doi.org/10.1001/jama.2015.12783
Pearlman M, Jeudy M, Chelmow D & Committee on Practice Bulletins—Gynecology. Practice Bulletin Number 179: Breast Cancer Risk Assessment and Screening in Average-Risk Women. Obstet Gynecol. 2017;130(1):e1-e16. https://doi.org/10.1097/aog.0000000000002158
Hoffman RM, Lewis CL, Pignone MP, et al. Decision-making processes for breast, colorectal, and prostate cancer screening: the DECISIONS survey. Med Decis Making: An International Journal of the Society for Medical Decision Making. 2010;30(5 Suppl):53s-64s. https://doi.org/10.1177/0272989x10378701
Schonberg MA, Breslau ES, McCarthy EP. Targeting of mammography screening according to life expectancy in women aged 75 and older. J Am Geriatr Soc. 2013;61(3):388-95. https://doi.org/10.1111/jgs.12123
Schoenborn NL, Huang J, Sheehan OC, Wolff JL, Roth DL, Boyd CM. Influence of Age, Health, and Function on Cancer Screening in Older Adults with Limited Life Expectancy. J Gen Intern Med. 2019;34(1):110-117. https://doi.org/10.1007/s11606-018-4717-y
Schonberg MA. Decision-Making Regarding Mammography Screening for Older Women. J Am Geriatr Soc. 2016;64(12):2413-2418. https://doi.org/10.1111/jgs.14503
Schoenborn NL, Boyd CM, Pollack CE. Different Types of Patient Health Information Associated With Physician Decision-making Regarding Cancer Screening Cessation for Older Adults. JAMA Netw Open. 2023;6(5):e2313367. https://doi.org/10.1001/jamanetworkopen.2023.13367
Schonberg MA, Ramanan RA, McCarthy EP, Marcantonio ER. Decision making and counseling around mammography screening for women aged 80 or older. J Gen Intern Med. 2006;21(9):979-85.
Schechter CB, Near AM, Jayasekera J, Chandler Y, Mandelblatt JS. Structure, Function, and Applications of the Georgetown-Einstein (GE) Breast Cancer Simulation Model. Med Decis Making: an international journal of the Society for Medical Decision Making. 2018;38(1_suppl):66s-77s. https://doi.org/10.1177/0272989x17698685
Mandelblatt JS, Stout NK, Schechter CB, et al. Collaborative Modeling of the Benefits and Harms Associated With Different U.S. Breast Cancer Screening Strategies. Ann Intern Med. 2016;164(4):215-25. https://doi.org/10.7326/m15-1536
Mandelblatt JS, Cronin KA, Bailey S, et al. Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med. 2009;151(10):738-47. https://doi.org/10.7326/0003-4819-151-10-200911170-00010
Jayasekera J, Li Y, Schechter CB, et al. Simulation Modeling of Cancer Clinical Trials: Application to Omitting Radiotherapy in Low-risk Breast Cancer. J Natl Cancer Inst. 2018;110(12):1360-1369. https://doi.org/10.1093/jnci/djy059
Alagoz O, Ergun MA, Cevik M, et al. The University of Wisconsin Breast Cancer Epidemiology Simulation Model: An Update. Med Decis Making: An International Journal of the Society for Medical Decision Making. 2018;38(1_suppl):99s-111s. https://doi.org/10.1177/0272989x17711927
Caswell-Jin JL, Plevritis SK, Tian L, et al. Change in Survival in Metastatic Breast Cancer with Treatment Advances: Meta-Analysis and Systematic Review. JNCI Cancer Spectr. 2018;2(4):pky062. https://doi.org/10.1093/jncics/pky062
Early Breast Cancer Trialists' Collaborative Group (EBCTCG), Peto R, Davies C, et al. Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet (London, England). 2012;379(9814):432–44. https://doi.org/10.1016/S0140-6736(11)61625-5
Lansdorp-Vogelaar I, Gulati R, Mariotto AB, et al. Personalizing age of cancer screening cessation based on comorbid conditions: model estimates of harms and benefits. Ann Intern Med. 2014;161(2):104-12. https://doi.org/10.7326/m13-2867
Ballard-Barbash R, Taplin SH, Yankaskas BC, et al. Breast Cancer Surveillance Consortium: a national mammography screening and outcomes database. AJR Am J Roentgenol. 1997;169(4):1001-8. https://doi.org/10.2214/ajr.169.4.9308451
Gangnon RE, Stout NK, Alagoz O, Hampton JM, Sprague BL, Trentham-Dietz A. Contribution of Breast Cancer to Overall Mortality for US Women. Med Decis Making: an international journal of the Society for Medical Decision Making. 2018;38(1_suppl):24S-31S. https://doi.org/10.1177/0272989X17717981
Mandelblatt JS, Near AM, Miglioretti DL, et al. Common Model Inputs Used in CISNET Collaborative Breast Cancer Modeling. Med Decis Making: An International Journal of the Society for Medical Decision Making. 2018;38(1_suppl):9s-23s. https://doi.org/10.1177/0272989x17700624
Trentham-Dietz A, Chapman CH, Bird J, Gangnon RE. Recent Changes in the Patterns of Breast Cancer as a Proportion of All Deaths According to Race and Ethnicity. Epidemiology. 2021;32(6):904-913. https://doi.org/10.1097/EDE.0000000000001394
Rockhill B, Byrne C, Rosner B, Louie MM, Colditz G. Breast cancer risk prediction with a log-incidence model: evaluation of accuracy. J Clin Epidemiol. 2003;56(9):856–61. S0895435603001240 [pii]
Breast Cancer Surveillance Consortium. Comparative Effectiveness of Breast Cancer Screening and Diagnostic Evaluation by Extent of Breast Density. 2023. Patient‐Centered Outcomes Research Institute (PCORI) Website. https://www.pcori.org/research-results/2016/comparing-effectiveness-breast-cancer-screening-and-diagnostic-tests-among-women-different-breast-densities-bcsc-advance-study#top_section. Accessed November 08, 2023.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-83. https://doi.org/10.1016/0021-9681(87)90171-8
Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53(12):1258-67. https://doi.org/10.1016/s0895-4356(00)00256-0
Owens DK, Davidson KW, Krist AH, et al. Medication Use to Reduce Risk of Breast Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;322(9):857-867. https://doi.org/10.1001/jama.2019.11885
Breast Cancer Surveillance Consortium (BCSC). Breast Cancer Surveillance Consortium Risk Calculator. 2015. BCSC website. https://tools.bcsc-scc.org/bc5yearrisk/calculator.htm. Accessed January 31, 2023.
Siu AL. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2016;164(4):279-96. https://doi.org/10.7326/m15-2886
Chapman CH, Schechter CB, Cadham CJ, et al. Identifying Equitable Screening Mammography Strategies for Black Women in the United States Using Simulation Modeling. Ann Intern Medi. 2021;174(12):1637-1646. https://doi.org/10.7326/M20-6506
Eddy DM, Hollingworth W, Caro JJ, et al. Model transparency and validation: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force-7. Med Decis Making: An International Journal of the Society for Medical Decision Making. 2012;32(5):733-43. https://doi.org/10.1177/0272989X12454579
Plevritis SK, Munoz D, Kurian AW, et al. Association of Screening and Treatment With Breast Cancer Mortality by Molecular Subtype in US Women, 2000-2012. JAMA. 2018;319(2):154-164. https://doi.org/10.1001/jama.2017.19130
National Cancer Institute (NCI). Probability of Developing or Dying of Cancer Software, Version 6.7.9 Surveillance Research Program, Statistical Methodology and Applications. 2012. NCI Website. http://surveillance.cancer.gov/devcan/. Accessed August 31, 2023.
Lahmann PH, Hoffmann K, Allen N, et al. Body size and breast cancer risk: findings from the European Prospective Investigation into Cancer And Nutrition (EPIC). Int J Cancer. 2004;111(5):762-71. https://doi.org/10.1002/ijc.20315
Trentham-Dietz A, Chapman, CH, Jayasekera J et al. Breast Cancer Screening with Mammography: An Updated Decision Analysis for the U.S. Preventive Services Task Force (USPSTF). 2023 Technical Report. USPSTF Website. Available at https://www.uspreventiveservicestaskforce.org/uspstf/document/draft-modeling-report/breast-cancer-screening-adults. Accessed August 31, 2023.
Institute of M. The National Academies Collection: Reports funded by National Institutes of Health. Integrating Large-Scale Genomic Information into Clinical Practice: Workshop Summary. National Academies Press (US) Copyright © 2012, National Academy of Sciences.; 2012.
Jayasekera J, Zhao A, Schechter C, et al. Reassessing the Benefits and Harms of Risk-Reducing Medication Considering the Persistent Risk of Breast Cancer Mortality in Estrogen Receptor–Positive Breast Cancer. J Clin Oncol. 0(0):JCO.22.01342. https://doi.org/10.1200/jco.22.01342
Jayasekera J, Sparano JA, O'Neill S, et al. Development and Validation of a Simulation Model–Based Clinical Decision Tool: Identifying Patients Where 21-Gene Recurrence Score Testing May Change Decisions. J Clin Oncol. 2021;39(26):2893-2902. https://doi.org/10.1200/jco.21.00651
Schonberg MA, Silliman RA, Ngo LH, et al. Older women's experience with a benign breast biopsy—a mixed methods study. J Gen Intern Med. 2014;29(12):1631-40. https://doi.org/10.1007/s11606-014-2981-z
Burnside ES, Lee SJ, Bennette C, et al. Using Collaborative Simulation Modeling to Develop a Web-Based Tool to Support Policy-Level Decision Making About Breast Cancer Screening Initiation Age. MDM Policy Pract. 2017 Jul;2(2):2381468317717982. https://doi.org/10.1177/2381468317717982. Epub 2017 Jul 8.
Ozanne EM, Schneider KH, Soeteman D, et al. onlineDeCISion.org: a web-based decision aid for DCIS treatment. Breast Cancer Res Treat. 2015;154(1):181–90. https://doi.org/10.1007/s10549-015-3605-y
Soeteman DI, Stout NK, Ozanne EM, et al. Modeling the effectiveness of initial management strategies for ductal carcinoma in situ. J Natl Cancer Inst. 2013;105(11):774-81. https://doi.org/10.1093/jnci/djt096
Gulati R, Feuer EJ, Etzioni R. Conditions for Valid Empirical Estimates of Cancer Overdiagnosis in Randomized Trials and Population Studies. Am J Epidemiol. 2016;184(2):140-7. https://doi.org/10.1093/aje/kwv342
United States Food and Drug Administration. MQSA National Statistics. 2023. Website. https://www.fda.gov/radiation-emitting-products/mqsa-insights/mqsa-national-statistics. Accessed August 31, 2023
Schousboe JT, Sprague BL, Abraham L, et al. Cost-Effectiveness of Screening Mammography Beyond Age 75 Years: A Cost-Effectiveness Analysis. Ann Intern Med. 2022; 175(1):11-19. https://doi.org/10.7326/M20-8076
Acknowledgements
The authors acknowledge the data provided by the Breast Cancer Surveillance Consortium, and initial data analysis conducted by Joanna Eavey with guidance from Charlotte Gard to develop the input parameters on breast cancer risk, screening performance, and stage distributions.
Funding
Research reported in this publication was supported by the National Institutes of Health (NIH) under the National Institute on Aging grant R01AG065311 and in part under the National Cancer Institute (NCI) grants U01CA152958 and U01CA253911 (CISNET). Dr. Jayasekera was supported by the Division of Intramural Research at the National Institute on Minority Health and Health Disparities of the NIH, and the NIH Distinguished Scholars Program. Dr. Mandelblatt’s effort was supported in part by R35CA197289; a pilot award supported by the Georgetown University Lombardi Cancer Center Support Grant (5P30CA051008).
Breast Cancer Surveillance Consortium (http://www.bcsc-research.org) data collection was supported by the National Cancer Institute (P01CA154292, U54CA163303). Dr. Schonberg’s effort was also supported by a NIA K24AG071906.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The study funders had no role in the design of the study; the collection, analysis, or interpretation of the data; the writing of the manuscript; or the decision to submit the manuscript for publication. The contents and views in this manuscript are those of the authors and should not be construed to represent the views of the National Institutes of Health. Opinions and comments expressed in this article belong to the authors and do not necessarily reflect those of the U.S. Government, Department of Health and Human Services, National Institutes of Health, or the National Institute on Minority Health and Health Disparities.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jayasekera, J., Stein, S., Wilson, O.W.A. et al. Benefits and Harms of Mammography Screening in 75 + Women to Inform Shared Decision-making: a Simulation Modeling Study. J GEN INTERN MED 39, 428–439 (2024). https://doi.org/10.1007/s11606-023-08518-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08518-4