Abstract
Background
Hospitalizations for infective endocarditis (IE) associated with opioid use disorder (O-IE) have increased in the USA and have been linked to high rates of discharge against medical advice (DAMA). DAMA represents a truncation of care for a severe infection, yet patient outcomes after DAMA are unknown.
Objective
This study aimed to assess readmissions following O-IE and quantify the impact of DAMA on outcomes.
Design
A retrospective study of a nationally representative dataset of persons’ inpatient discharges in the USA in 2016
Participants
A total of 6018 weighted persons were discharged for O-IE, stratified by DAMA vs. other discharge statuses. Of these, 1331 (22%) were DAMA.
Main Measures
The primary outcome of interest was 30-day readmission rates, stratified by discharge type. We also examined the total number of hospitalizations during the year and estimated the effect of DAMA on readmission.
Key Results
Compared with non-DAMA, those experiencing DAMA were more commonly female, resided in metropolitan areas, lower income, and uninsured. Crude 30-day readmission following DAMA was 50%, compared with 21% for other discharge types. DAMA was strongly associated with readmission in an adjusted logistic regression model (OR 3.72, CI 3.02–4.60). Persons experiencing DAMA more commonly had ≥2 more hospitalizations during the period (31% vs. 18%, p<0.01), and were less frequently readmitted at the same hospital (49% vs 64%, p<0.01).
Conclusions
DAMA occurs in nearly a quarter of patients hospitalized for O-IE and is strongly associated with short-term readmission. Interventions to address the root causes of premature discharges will enhance O-IE care, reduce hospitalizations and improve outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infective endocarditis (IE), an infection of the heart with potentially severe medical sequelae, is an increasingly recognized consequence of the opioid crisis. Hospitalizations for IE associated with injection drug use have sharply increased over recent years,1,2,3 driven by misuse of prescription and illicit opioids and heroin,3 and resulting in long and costly hospitalizations. The long lengths of stay stem from the prolonged courses of parenteral antimicrobials that treat IE, typically delivered in the inpatient setting, and recovery from valvuloplasty, which is often indicated in IE treatment. During this period, patients do not routinely receive medications for opioid use disorder (OUD),4,5 despite their association with a lower risk of returning to drug use,6 and support for their use voiced by major medical organizations.7,8
A substantial proportion of drug-associated IE hospitalizations results in patients’ termination of inpatient care prior to providers’ recommendation. In recent years, this phenomenon, often termed discharge against medical advice (DAMA), has risen for drug-associated IE, from 12% in 2010 to 21% in 2015.9 In contrast, DAMA during a hospitalization for IE due to other causes occurs in less than 3% of hospitalizations overall.3,9,10 DAMA for IE hospitalizations, which has been linked to substance use disorders,11 almost certainly represents a truncation in treatment for a potentially fatal infection. Furthermore, patients with untreated OUD may develop withdrawal symptoms or receive inadequate pain treatment, leading to negative in-hospital experiences.12 These and other factors, such as stigma,12,13 financial responsibilities,14 housing,15 and use of both opioids and stimulants,16 have been identified as contributors to DAMA.
There are little data on healthcare utilization and outcomes following DAMA for IE. For example, it is unknown whether patients return to resume care and when those readmissions occur. In this study, we characterized the clinical outcomes of patients after DAMA for IE and rates of readmission, aggregate lengths of stay, and costs that follow downstream from DAMA. We utilized a large, nationally representative database of US hospitalizations to describe the prevalence of DAMA following IE associated with OUD (opioid use disorder-associated IE, O-IE) and to examine short-term readmissions. We hypothesized that DAMA following O-IE was common and strongly associated with readmission in the first 30 and 90 days after discharge, considering patients’ ongoing need for IE care. Our findings characterize the complexities of caring for patients with O-IE and may help providers, health systems and public health entities better provide care.
Methods
Data Source
We analyzed the 2016 Nationwide Readmissions Database (NRD), developed by the Agency for Healthcare Research and Quality.17 The NRD comprises all hospital discharges and in-state readmissions from 27 states and includes weights to provide nationally representative estimates (Appendix Table 1). NRD domains include demographics, diagnoses, procedures, charges, disposition, and an internal identifier allowing individuals to be tracked across in-state readmissions within a calendar year. Analyses were performed using weighted estimates, accounting for clustering of discharges at the hospital of the index hospitalization, except for the assessment of readmission reasons, which was performed on unweighted data. The study was reviewed by the University of North Carolina institutional review board and deemed exempt from full human subjects’ research review.
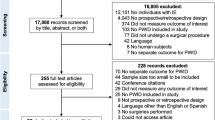
Inclusion Criteria
We included people aged ≥18 years who had a hospital discharge with an International Classification of Diseases, Tenth Revision (ICD-10-CM) diagnosis code of IE and a diagnosis code that reflected OUD. We used the same codes for OUD recently employed in a study of O-IE hospitalizations.18
The first discharge in the calendar year coded for both OUD and IE was labeled the index discharge for O-IE. Persons with an index discharge in January were excluded because there was no way to ascertain whether it was a short-term readmission from a hospitalization in the prior year. To allow a minimum of 30 days of potential follow-up time, persons with index discharges occurring in December were excluded.
Discharge Against Medical Advice and Readmission
The main exposure was DAMA, which was coded (Yes/No) based on the patient discharge disposition variable in the NRD. Those discharged under any other status were labeled non-DAMA. Readmission was determined by any subsequent discharge (all-cause) during the follow-up period. The primary outcome was readmission within 30 days. Secondary outcomes included 90-day readmission (among those contributing at least 90 days of follow-up time), readmission to the same hospital as the initial hospitalization (vs. another), in-hospital death during a subsequent admission, and the primary reason for readmission.
Analysis
We first examined the proportion of index hospitalization discharges with a disposition of DAMA. We then estimated failure curves for time to readmission, stratified by DAMA status, and used the log-rank test to determine if the curves differed.
Among O-IE patients, we estimated the proportion experiencing readmission within 30-days, stratified by DAMA, and among those with at least 90 days of follow-up, we examined 90-day readmissions. We estimated hospital costs accrued per individual over the calendar year, defined as the sum of hospital charges for the index hospitalization and all readmissions. Hospital charges were converted to costs using charge-to-cost ratios published with the NRD.
We assessed the association between DAMA and 30-day readmission using a logistic regression model, controlling for age, gender, metropolitan residence, insurance status, polysubstance use, alcohol use disorder, any selected psychiatric disorder (mood, anxiety or psychotic diagnosis), heart valve surgery during the index hospitalization and length of stay during the index hospitalization (dichotomized at <=14 days and >14). These covariates for adjustment were chosen to include basic sociodemographics, as well as mental health conditions that have been associated with DAMA and readmissions, or a competing outcome such as death.19,20,21,22,23 Polysubstance use has been linked to increased risk of DAMA among patients with IE.24 Heart valve surgery and length of stay were chosen based on a priori assessment that they would be linked to both DAMA and readmission. To control for severity, we also assessed the Charlson comorbidity index score (CCI), a mortality prediction score based on 19 medical comorbidities, using a previously published algorithm that was developed for use with administrative data in ICD-10-CM 25. CCI was dichotomized at <=2 and >2 and included in the adjusted analysis. Polysubstance use was defined as a code for the use of at least one illicit substance other than opioids that could conceivably be injected (i.e., other than marijuana). Heart valve surgery was defined as the presence of an ICD-10 procedure code for surgery that could be used to treat IE. A full list of ICD-10 codes used in the analysis is in the Appendix Tables.
The reasons for the first readmission were assessed by taking the first diagnosis code listed for the discharge and categorizing it within the Clinical Classification Software Refined, an AHRQ system which groups ICD diagnoses into clinically relevant categories.26 Statistical comparisons of survey-weighted continuous variables were performed with R (RStudio Team, Boston, MA). All other analyses were performed with SAS, version 9.4 (SAS Institute, Cary, NC).
Results
Study Population
In total, 3222 individuals with ≥1 hospitalization for O-IE met the inclusion criteria. This corresponded to 6,018 weighted persons in the analysis, of which 1331 (22%) were DAMA and 4686 (78%) were not. Compared to other patients, DAMA patients were significantly younger, more commonly female, and more likely to have a metropolitan residence, lower income, and self-pay insurance status. Compared to other patients, DAMA patents also had significantly lower comorbidity, were less likely to undergo heart valve surgery, and had shorter lengths of stay during their index hospitalization (Table 1 and Appendix Table 9).
Readmissions
Among persons with a DAMA disposition on their index discharge record, 50% were readmitted within 30 days (Table 2 and Appendix Table 10). In contrast, fewer non-DAMA patients were readmitted within 30 days (21%, p<0.001). Of the 4863 weighted participants contributing at least 90 days of follow-up time, 90-day readmission occurred in 59% and 34%, respectively (p<0.001). The probability of readmission was higher in the DAMA group than in the non-DAMA group across the entirety of the 10-month observation period (Fig. 1, p<0.001).
Time to first readmission following opioid use disorder-associated infective endocarditis. Figure legend: Cumulative all-cause readmissions following inpatient discharge for a hospitalization for opioid use disorder-associated infective endocarditis. Data is drawn from the 2016 National Readmissions Database (Agency for Healthcare Research and Quality). Shaded areas represent 95% Hall-Wellner bands.
The primary reason for the first readmission was significantly different between DAMA and non-DAMA groups (p<0.001). The most common reason in both groups was endocarditis; however, this comprised a larger share of readmissions after DAMA (44%), compared with non-DAMA (29%). The second most common reason was septicemia, comprising 23% of post-DAMA readmissions, compared with 19% of non-DAMA readmissions.
Readmission Trajectories and Costs
More persons in the DAMA group had three or more hospitalizations during the ten-month observation period, compared with non-DAMA (31% vs. 18%, p<0.001) (Table 2). However, those in the DAMA group spent fewer total days hospitalized during the period (median 19 vs. 25, p<0.001) and accrued less total hospital costs over the course of the period (median $51,472 vs. $68,975, p<0.001). Readmissions mostly occurred early in the DAMA group (Fig. 1) and a minority (49%) took place at the same hospital as the index hospitalization, significantly less than the non-DAMA group (64%, p<0.001). There was no difference between groups in the proportion who died during a subsequent hospitalization.
Factors Associated with 30-Day Readmission
In the bivariate models, DAMA was associated with readmission (Odds Ratio [OR] 3.68, 95% confidence intervals [CI] 3.01–4.50), as was a higher comorbidity score (OR 1.41, CI 1.10–1.81) (Table 3). The receipt of heart valve surgery during the index admission was linked with lower odds of readmission, as was a longer length of stay during the initial hospitalization and having private insurance. In the adjusted logistic regression model, the magnitude of the association between DAMA and readmission (OR 3.72, CI 3.04–4.56) was similar to the unadjusted association.
Discussion
In this nationally representative analysis of over 6000 weighted persons hospitalized with O-IE, DAMA was exceptionally common, occurring in one of five hospitalizations. This finding is consistent with previously-described DAMA rates in both national and local studies.2,9,10 In addition, we found a strong link between DAMA and short-term readmission. This latter finding suggests that preventing DAMA and addressing its underlying causes could improve treatment completion rates during the initial O-IE hospitalization and lessen the risk of adverse outcomes and readmissions.
Our findings for O-IE starkly contrast with DAMA and readmissions among all-cause hospitalizations. Among all-cause hospitalizations, 1-2% of discharges are for DAMA, with 20% readmitted within 30 days.21,27 In contrast, the rate of DAMA for O-IE (22%) is approximately 10-20 times higher than for all conditions, and the 30-day readmission rate for O-IE (50%) is more than double that for all conditions.21,27
We found nearly a third accrued at least two readmissions during the 10-month follow-up period. This pattern suggests that DAMA is not an isolated event, but rather occurs in a cycle of protracted and fragmented inpatient care. That fragmentation is reflected in the high proportion (>50%) of readmissions among DAMA patients occurring at hospitals other than the index hospital. In contrast, 36% of readmissions among non-DAMA patients occurred at a different hospital. Similar although less extreme patterns have been observed for readmissions among DAMA and non-DAMA patients following all-cause hospitalizations.21 Given the complexity of treating O-IE (which is most typically caused by Staphylococcus aureus28,29,30) and the severity of its sequelae, uncoordinated care due to interruptions and transitions between institutions may be especially harmful. Our findings also suggest that, in designing studies to assess O-IE readmissions, particularly following DAMA, it is unrealistic to assume that readmissions will predominantly occur at the index hospital.
A quarter of those undergoing DAMA were uninsured, compared with 15% among non-DAMA. The threat of high self-pay costs may contribute to DAMA. Alternatively, noninsurance may be a surrogate for other sociodemographic factors that may modulate DAMA, such as inadequate care for OUD and unstable housing.
The median costs accrued among DAMA patients, over $50,000, is likely an underestimate considering that some participants were followed for as little as one month. Although not captured in our data, we speculate that the long-term costs likely continue to mount for DAMA patients as readmissions will occur in subsequent calendar years, whereas patients who do not leave against medical advice and receive a full course of therapy accrue fewer total hospitalizations. The NRD does not permit assessments across calendar years barring assessment of longer-term costs, and further study with longer-term datasets is needed to investigate long-term costs of care. Nonetheless, the care of O-IE has the potential to strain healthcare systems, which may receive little remuneration for the care of uninsured patients. Providers and administrators should therefore invest in addressing the factors that lead to DAMA to ensure that patients’ index hospitalization results in definitive treatment.
Our findings suggest a need for inpatient management strategies to reduce DAMA. The receipt of inpatient pharmacotherapy for OUD has been associated with lower DAMA and readmission,31,32 although the long-term effect remains uncertain as patients also need ongoing engagement in OUD care after discharge.33 A recent large study of hospitalizations for injection drug-related IE found that nearly a third of DAMAs occurred in the first 2 days of hospitalizations,9 suggesting that short-term withdrawal symptoms may have precipitated the early discharge, and highlighting a small window of opportunity to prevent DAMA for certain patients. In our study, while a quarter of DAMA patients left within 2 days, the median length of stay was 6 days, suggesting that early post-admission withdrawal is unlikely the primary or sole factor driving DAMA. Additionally, patients with O-IE are often hospitalized for their entire course of therapy, which presents significant lifestyle challenges. One possible remedy is to identify patients who are candidates for outpatient parenteral antibiotics34, thereby reducing their burden of inpatient care.
People hospitalized with substance use disorders frequently experience stigmatizing interactions with hospital staff.12 In a survey of persons with soft tissue infections, 54% cited “judgment or mistreatment” as motivating DAMA, and 60% said those concerns led to subsequently delaying or avoiding care.13 Some hospitals impose restrictions upon persons who use drugs such as limiting visitors, requiring security searches, and temporarily confiscating cellphones.35 Such policies likely compound experiences of stigma and they reportedly motivate DAMA.12 The numerous negative experiences that culminate in DAMA may explain why patients may understandably seek readmission at a different hospital. Increasingly, hospitals are piloting multidisciplinary efforts to address the holistic needs of O-IE patients to integrate medications for OUD, peer support, harm reduction, and linkage to post-discharge care.36,37
In infective endocarditis, the standard of care is often six weeks of parenteral antibiotics.38 Yet after DAMA, 40% of study O-IE patients were not readmitted within three months. The longitudinal outcomes of these patients are unknown. Patients who are never readmitted may have adverse out-of-hospital outcomes, such as progressive endocarditis or overdose. Alternatively, it is feasible that some either clear or temporize their infection following the short hospitalization. Clinical trials have supported two-week therapy for uncomplicated tricuspid endocarditis in select cases of injection drug-related IE.38 In our analysis, >25% of patients stayed for over two weeks prior to DAMA, suggesting that some may have completed a substantial fraction of their treatment. Additionally, some may receive oral antibiotics at the time of DAMA. A recent observational study found improved outcomes among patients who received antibiotics at the time of DAMA, compared with those who did not.39
The value of designating discharges as against medical advice has been reevaluated, with critics noting that it disproportionately impacts socially vulnerable individuals, may further alienate them from care, and adds no benefit to patients.40 In the case of substance use-related infections, which impact a population that is already reluctant to seek medical care due to negative healthcare experiences,13 the risk of further stigmatizing them to the healthcare system could be dire. All discharges should focus on advancing patient care, even when patient preferences do not align with those of the provider.40 Some have advocated for the term “patient-directed discharge” to replace DAMA.16,41 To be consistent with data elements in the NRD, we opted to use the term DAMA in this article. However, a reconsideration of both the concept and terminology surrounding DAMA is necessary.
Importantly, providers caring for O-IE patients should develop best practices for engaging patients at the time of DAMA in a plan for follow-up care, linkage to resources, such as harm reduction programs, and prescription of necessary oral medications. In one cross-sectional study against medical advice discharges from a large academic hospital, only a third were given a follow-up appointment at discharge.42 Further research is needed to both qualitatively examine the contemporary reasons that motivate DAMA among patients with invasive drug-related infections, such as O-IE, and to trial interventions to enhance engagement in inpatient and post-discharge care.
This study is subject to several limitations. First, the performance of the algorithm identifying O-IE cases cannot be validated in this database. However, the demographics of O-IE patients did resemble closely the socio-demographic profile of persons with injection drug-related IE seen in numerous other studies.43 Second, we were unable to confirm that the O-IE hospitalization that we designated as the index was not a readmission or recurrent infection. The vast majority of readmissions occurred within the first 30 days; therefore, our approach of excluding hospitalizations occurring in January likely excluded most readmissions from being labeled as index hospitalizations. Third, we focused only on OUD-associated IE, but this does not represent all injection drug-related IE. Fourth, our population may be underpowered to detect fine associations. Finally, we only identified readmissions within the same state as the index hospitalization. Although this undercounts readmissions, we believe the number of out-of-state readmissions is low.
Conclusions
DAMA is common in O-IE, occurring in nearly a quarter of persons, and is linked to frequent and early readmission. Patients who experience DAMA are at risk of uncoordinated and protracted care for a severe infection. Inadequate addiction care in the hospital may contribute to DAMA, but DAMA may also be a symptom of structural failings in how inpatient care is delivered to vulnerable patients with OUD. Stemming premature discharge will improve the initial care for O-IE and likely reduce further hospitalizations. Finally, efforts to reframe DAMA and enhance patient engagement post-hospitalization can help imbue patient-centered care into patient-directed discharges.
References
Wurcel AG, Anderson JE, Chui KKH, et al. Increasing Infectious Endocarditis Admissions Among Young People Who Inject Drugs. Open Forum Infect Dis. 2016;3(3). https://doi.org/10.1093/ofid/ofw157
Meisner JA, Anesi J, Chen X, Grande D. Changes in infective endocarditis admissions in Pennsylvania during the opioid epidemic. Clin Infect Dis. https://doi.org/10.1093/cid/ciz1038
Schranz AJ, Fleischauer A, Chu VH, Wu LT, Rosen DL. Trends in Drug Use-Associated Infective Endocarditis and Heart Valve Surgery, 2007 to 2017: A Study of Statewide Discharge Data. Ann Intern Med. 2019;170(1):31. https://doi.org/10.7326/M18-2124.
Rosenthal ES, Karchmer AW, Theisen-Toupal J, Castillo RA, Rowley CF. Suboptimal Addiction Interventions for Patients Hospitalized with Injection Drug Use-Associated Infective Endocarditis. The American Journal of Medicine. 2016;129(5):481-485. https://doi.org/10.1016/j.amjmed.2015.09.024
Serota DP, Niehaus ED, Schechter MC, et al. Disparity in Quality of Infectious Disease vs Addiction Care Among Patients With Injection Drug Use–Associated Staphylococcus aureus Bacteremia. Open Forum Infect Dis. 2019;6(7). https://doi.org/10.1093/ofid/ofz289
Liebschutz JM, Crooks D, Herman D, et al. Buprenorphine Treatment for Hospitalized, Opioid-Dependent Patients. JAMA. Intern Med. 2014;174(8):1369-1376. https://doi.org/10.1001/jamainternmed.2014.2556
Medication Treatment for Opioid Use Disorder in the Inpatient Hospital Setting. National Institute on Drug Abuse. Published --. Accessed September 11, 2022. https://nida.nih.gov/nidamed-medical-health-professionals/science-to-medicine/medication-treatment-opioid-use-disorder/medication-treatment-opioid-use-disorder-in-inpatient
Baddour LM, Weimer MB, Wurcel AG, et al. Management of Infective Endocarditis in People Who Inject Drugs: A Scientific Statement From the American Heart Association. Circulation. 0(0):https://doi.org/10.1161/CIR.0000000000001090.
Kimmel SD, Kim JH, Kalesan B, Samet JH, Walley AY, Larochelle MR. Against medical advice discharges in injection and non-injection drug use-associated infective endocarditis: A nationwide cohort study. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa1126
Thakarar K, Rokas KE, Lucas FL, et al. Mortality, morbidity, and cardiac surgery in Injection Drug Use (IDU)-associated versus non-IDU infective endocarditis: The need to expand substance use disorder treatment and harm reduction services. PLOS ONE. 2019;14(11):e0225460. https://doi.org/10.1371/journal.pone.0225460
Spooner KK, Salemi JL, Salihu HM, Zoorob RJ. Discharge Against Medical Advice in the United States, 2002-2011. Mayo Clinic Proceedings. 2017;92(4):525-535. https://doi.org/10.1016/j.mayocp.2016.12.022
Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: A qualitative study. Substance Abuse. 2019;0(0):1-7. https://doi.org/10.1080/08897077.2019.1671942
Summers PJ, Hellman JL, MacLean MR, Rees VW, Wilkes MS. Negative experiences of pain and withdrawal create barriers to abscess care for people who inject heroin. A mixed methods analysis. Drug and Alcohol Dependence. 2018;190:200-208. https://doi.org/10.1016/j.drugalcdep.2018.06.010
Green P, Watts D, Poole S, Dhopesh V. Why patients sign out against medical advice (AMA): factors motivating patients to sign out AMA. American Journal of Drug & Alcohol Abuse. 2004;30(2):489-493. https://doi.org/10.1081/ADA-120037390
Ti L, Milloy MJ, Buxton J, et al. Factors Associated with Leaving Hospital against Medical Advice among People Who Use Illicit Drugs in Vancouver, Canada. PLoS One. 2015;10(10). https://doi.org/10.1371/journal.pone.0141594
Serota DP, Bartholomew TS, Tookes HE. Evaluating Differences in Opioid and Stimulant Use-associated Infectious Disease Hospitalizations in Florida, 2016–2017. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa1278
NRD Database Documentation. Healthcare Cost and Utilization Project. Published December 1, 2020. Accessed December 20, 2020. https://www.hcup-us.ahrq.gov/db/nation/nrd/nrddbdocumentation.jsp
Barocas JA, Morgan JR, Wang J, McLoone D, Wurcel A, Stein MD. Outcomes Associated With Medications for Opioid Use Disorder Among Persons Hospitalized for Infective Endocarditis. Clin Infect Dis. 2021;72(3):472-478. https://doi.org/10.1093/cid/ciaa062
Saitz R, Ghali WA, Moskowitz MA. The Impact of Leaving Against Medical Advice on Hospital Resource Utilization. J Gen Intern Med. 2000;15(2):103-107. https://doi.org/10.1046/j.1525-1497.2000.12068.x
Kuo CJ, Tsai SY, Liao YT, Lee WC, Sung XW, Chen CC. Psychiatric discharge against medical advice is a risk factor for suicide but not for other causes of death. J Clin Psychiatry. 2010;71(6):808-809. https://doi.org/10.4088/JCP.09l05404blu
Tan SY, Feng JY, Joyce C, Fisher J, Mostaghimi A. Association of Hospital Discharge Against Medical Advice With Readmission and In-Hospital Mortality. JAMA Netw Open. 2020;3(6). https://doi.org/10.1001/jamanetworkopen.2020.6009
Sreenivasan J, Kaul R, Khan MS, Malik A, Usman MS, Michos ED. Mental health disorders and readmissions following acute myocardial infarction in the United States. Sci Rep. 2022;12(1):3327. https://doi.org/10.1038/s41598-022-07234-z
Ahmedani BK, Solberg LI, Copeland LA, et al. Psychiatric Comorbidity and 30-Day Readmissions After Hospitalization for Heart Failure, AMI, and Pneumonia. PS. 2015;66(2):134-140. https://doi.org/10.1176/appi.ps.201300518
Serota DP, Bartholomew TS, Tookes HE. Evaluating Differences in Opioid and Stimulant Use-associated Infectious Disease Hospitalizations in Florida, 2016–2017. Clinical Infectious Diseases. 2021;73(7):e1649-e1657. https://doi.org/10.1093/cid/ciaa1278
Glasheen WP, Cordier T, Gumpina R, Haugh G, Davis J, Renda A. Charlson Comorbidity Index: ICD-9 Update and ICD-10 Translation. Am Health Drug Benefits. 2019;12(4):188-197.
Clinical Classifications Software Refined (CCSR) for ICD-10-CM Diagnoses. Accessed May 11, 2020. https://www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp#user
Kumar N. Burden of 30-Day Readmissions Associated With Discharge Against Medical Advice Among Inpatients in the United States. The American Journal of Medicine. 2019;132(6):708-717.e4. https://doi.org/10.1016/j.amjmed.2019.01.023
Geirsson A, Schranz A, Jawitz O, et al. The Evolving Burden of Drug Use Associated Infective Endocarditis in the United States. Ann Thorac Surg. 2020;110(4):1185-1192. https://doi.org/10.1016/j.athoracsur.2020.03.089
Rodger L, Glockler-Lauf SD, Shojaei E, et al. Clinical Characteristics and Factors Associated With Mortality in First-Episode Infective Endocarditis Among Persons Who Inject Drugs. JAMA Netw Open. 2018;1(7):e185220-e185220. https://doi.org/10.1001/jamanetworkopen.2018.5220
Huang G, Barnes EW, Peacock JE. Repeat Infective Endocarditis in Persons Who Inject Drugs: “Take Another Little Piece of my Heart”. Open Forum Infect Dis. 2018;5(12). https://doi.org/10.1093/ofid/ofy304
Marks LR, Munigala S, Warren DK, Liang SY, Schwarz ES, Durkin MJ. Addiction Medicine Consultations Reduce Readmission Rates for Patients With Serious Infections From Opioid Use Disorder. Clin Infect Dis. 2019;68(11):1935-1937. https://doi.org/10.1093/cid/ciy924
Wang SJ, Wade E, Towle J, et al. Effect of Inpatient Medication-Assisted Therapy on Against-Medical-Advice Discharge and Readmission Rates. The American Journal of Medicine. 2020;133(11):1343-1349. https://doi.org/10.1016/j.amjmed.2020.04.025
Suzuki J, Johnson JA, Montgomery MW, et al. Medications for Opioid Use Disorder Demonstrate Clear Benefit for Patients With Invasive Infections: Letter-in-reply. J Addict Med. 2020;14(6):518-519. https://doi.org/10.1097/ADM.0000000000000651
Price CN, Solomon DA, Johnson JA, Montgomery MW, Martin B, Suzuki J. Feasibility and Safety of Outpatient Parenteral Antimicrobial Therapy in Conjunction With Addiction Treatment for People Who Inject Drugs. The Journal of Infectious Diseases. 2020;222(Supplement_5):S494-S498. https://doi.org/10.1093/infdis/jiaa025
Meyer H. U. of Tenn. Medical Center admits drug-addicted patients under strict conduct rules. Modern Healthcare. Published July 7, 2018. . https://www.modernhealthcare.com/article/20180707/NEWS/180709961/u-of-tenn-medical-center-admits-drug-addicted-patients-under-strict-conduct-rules
Serota DP, Tookes HE, Hervera B, et al. Harm reduction for the treatment of patients with severe injection-related infections: description of the Jackson SIRI Team. Ann Med. 53(1):1960-1968. https://doi.org/10.1080/07853890.2021.1993326
Englander H, Weimer M, Solotaroff R, et al. Planning and Designing the Improving Addiction Care Team (IMPACT) for Hospitalized Adults with Substance Use Disorder. J Hosp Med. 2017;12(5):339-342. https://doi.org/10.12788/jhm.2736
Baddour LM, Wilson WR, Bayer AS, et al. Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications. Circulation. Published online January 1, 2015. https://doi.org/10.1161/CIR.0000000000000296
Marks LR, Liang SY, Muthulingam D, et al. Evaluation of partial oral antibiotic treatment for persons who inject drugs and are hospitalized with invasive infections. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa365
Alfandre D, Brenner J, Onukwugha E. Against Medical Advice Discharges. J Hosp Med. 2017;12(10):843-845. https://doi.org/10.12788/jhm.2796
Eaton EF, Westfall AO, McClesky B, et al. In-Hospital Illicit Drug Use and Patient-Directed Discharge: Barriers to Care for Patients With Injection-Related Infections. Open Forum Infect Dis. 2020;7(3). https://doi.org/10.1093/ofid/ofaa074
Tummalapalli SL, Chang BA, Goodlev ER. Physician Practices in Against Medical Advice Discharges. J Healthc Qual. 2020;42(5):269-277. https://doi.org/10.1097/JHQ.0000000000000227
Schranz A, Barocas JA. Infective Endocarditis in Persons Who Use Drugs: Epidemiology, Current Management, and Emerging Treatments. Infect Dis Clin North Am. 2020;34(3):479-493. https://doi.org/10.1016/j.idc.2020.06.004
Funding
AJS was supported by the National Institute of Allergy and Infectious Diseases (T32AI070114) and the National Institute on Drug Abuse (K23DA049946). LTW was supported by the National Institute on Drug Abuse (UG1DA040317).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 43 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schranz, A.J., Tak, C., Wu, LT. et al. The Impact of Discharge Against Medical Advice on Readmission After Opioid Use Disorder-Associated Infective Endocarditis: a National Cohort Study. J GEN INTERN MED 38, 1615–1622 (2023). https://doi.org/10.1007/s11606-022-07879-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07879-6