Abstract
Background
Prior work has shown that provider network structures correlate with outcomes such as patient costs, utilization, and care. However, it remains unknown whether certain provider networks are associated with reduced disparity gaps.
Methods
We study the population of Medicare beneficiaries with diabetes who were continuously enrolled in Medicare FFS in 2016. Using multivariable regression analysis of county-level risk adjusted cost, hospitalization, emergency department visits, A1c testing, and preventable diabetes-related hospitalizations, we measure the effect that the relative network connectivity of primary care providers (PCPs) in relation to medical and surgical specialists (PCP/Specialist degree centrality ratio), derived from Medicare patient sharing data, has on non-Hispanic black-to-white disparity gaps controlling for county-level socioeconomic and demographic variables and state fixed effects.
Results
Relative to non-Hispanic white, our adjusted results show that non-Hispanic black beneficiaries have $1673 (p<0.001) higher risk adjusted total costs, 2.6 (p<0.001) more hospitalizations (per 1000 beneficiaries), 11.6 (p<0.001) more ED visits (per 1000 beneficiaries), receive 2.2% (p<0.001) less A1c testing, and have 69.4 (p<0.01) more (per 100,000) avoidable diabetes-related hospital admissions. Our main results show that increasing the PCP/Specialist degree centrality ratio by one standard deviation is associated with a disparity gap decrease of 25.3% (p<0.01) in hospitalizations, 8.3% (p<0.05) in ED visits, 2.8% (p<0.01) in A1c testing, and 26.9% (p<0.1) in the volume of preventable diabetes-related hospital admissions.
Conclusions
Network structures where PCPs are more central relative to medical and surgical specialists are associated with reduced non-Hispanic black-to-white disparity gaps, suggesting that how we organize and structure our health systems has implications for disparity gaps between non-Hispanic black and white Medicare beneficiaries with diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Diabetes is a leading cause of death and is the largest single condition contributor to overall personal health care spending in the USA.1,2,3 There are well-documented disparities by race/ethnicity across health system and clinical outcomes, with individuals from lower socioeconomic status and minority racial groups having disproportionately poorer outcomes.4,5,6,7 Primary care physicians (PCP) care for over 90% of individuals with type 2 diabetes, and recent findings indicate that PCP centric structures that align with the medical home model appear well suited for improving care and outcomes for this patient population.8,9,10 While these findings are still primarily based on observational studies, related work assessing the effect of Accountable Care Organizations on patient care has indicated evidence of a potential causal link between organizational structure and patient outcomes.11 With that noted, not all patients receive care in PCP centric structures, and many are instead confronted with fragmented care delivery, which has been shown to reduce quality of care, increase utilization, increase cost, and lead to poorer outcomes.12,13
What remains unknown is whether documented health disparities among patients with diabetes may be in part accounted for by underlying health care provider structures. As such, this study sets out to examine the relationship between Medicare provider network structure and county-level variation in risk adjusted cost, hospitalization, emergency department visits, A1c testing, and preventable diabetes hospitalizations for Medicare beneficiaries with a diagnosis of diabetes. We capture network structure using a relative degree centrality ratio measure that compares the relative connectivity of PCP and specialist (medical and surgical) providers. If our measure is equal to one, then this represents a network where PCPs and specialists occupy similar positions within the network, while ratios greater than one indicate that PCPs capture a more central (and coordinating) role within the network than do specialists. We hypothesize that counties where primary care providers serve a more central role within the provider network structure relative to medical and surgical specialists are more robust to the manifestation of racial disparities, and that these structures therefore experience lower non-Hispanic black-to-white disparities within the Medicare diabetes population.
METHODS
Study Sample
We use county-level cost, utilization, and outcome measures from the Mapping Medicare Disparities (MMD) database in 2016.14 This source draws its county measures from 100% of CMS administrative claims data for Medicare beneficiaries continuously enrolled in the FFS program. This data excludes beneficiaries who are enrolled in a Medicare Advantage plan at any time during 2016.15 All county-level measures were obtained across both non-Hispanic black (NHB) and non-Hispanic white (NHW) Medicare beneficiaries who all had a diagnosis of diabetes (based on ICD-10 encodings). In order to maintain beneficiary confidentiality, the MMD database does not report measures for counties where the sample population contains less than 11 individuals. This means that as we stratify by race and a diagnosis of diabetes, we have areas that either do not have data or are excluded due to insufficient number of individuals. In total, depending on the measure and population race, we have between 1769 and 3124 counties covered by our outcome data. There is no age restriction for the main outcome variables; however, one of our outcome variables (A1c testing rate) is supplemented from the Dartmouth Atlas Project database, based on 2015 data representing Medicare patients aged 65–75.16 This measure is available across 2135 counties for NHW, and 1303 counties for NHB beneficiaries within our sample.
Our outcome data was combined with county-level provider patient sharing (network) data that was constructed based on 2016 Medicare claims.17 This data defines a patient sharing link on the basis of two Medicare providers having at least 11 shared patients. This link-relation cutoff is aligned with prior work in this area, and it helps reduce concerns related to the inclusion of potentially spurious network links within our analysis. 18,19 We next linked providers within our patient sharing data (using their National Provider Identifiers) with the Medicare Physician Compare dataset.20 This matching allows us to extract each provider’s specialty and location of practice, which we used for the purpose of constructing our county-specific provider networks. For our final county networks, we have PCP degree measures for 2468 of these, and PCP/Specialist degree ratios (defined below) across 2167 of the counties. Exclusion is due to (i) lack of Medicare providers located within a given area, (ii) lack of patient sharing relationships between providers within a given area, or (iii) due to the CMS data requirement of only providing data on provider patient sharing ties so long as they share at least 11 patients. Additionally, we also source a number of county-level covariates from the 2020 County Health Rankings Dataset.21 For this data, we have close to complete coverage of the US counties.
These steps result in two final analysis samples. The first pools together all county outcomes across race, and leaves us with a combined analysis sample of 2523–3866 county-by-race units of observation (depending on the outcome measure studied). The second sample only looks at counties for which we have outcome measures for both NHW and NHB Medicare beneficiaries, which is a requirement for our constructed NHB-to-NHW disparity gap measures (described below). For this sample, our coverage spans 1047–1647 counties.
Study Variables
Outcome Measures: Cost, Utilization, and Care Outcomes
The risk-adjusted average total cost is based on Medicare beneficiaries continuously enrolled in Medicare FFS Parts A and B. These costs refer to expected total costs based on the CMS Hierarchical Condition Category (HCC) risk adjustment model, and they are reported on a per beneficiary basis.15,22 Hospitalizations are based on continuously enrolled beneficiaries in Medicare Part A. The hospitalization rate is computed using the principal diagnosis codes within the Medicare administrative claims, and it is reported on a per 1000 beneficiaries basis. Emergency department (ED) visit rates are based on beneficiaries continuously enrolled in Medicare FFS Parts A and B. The ED visits rate represents the total number of ED visits within 2016 where the beneficiary was released from the outpatient setting and where the beneficiary was admitted to an inpatient setting. Our measure of the percent of beneficiaries receiving an annual A1c test is based on CPT codes 83036 and 83037 and CPT II codes 3046F and 3047F, and it is measured for Medicare patients aged 65–75.16 Our preventable hospitalization measure is based on the AHRQ Preventive Quality Indicator (PQI), which is computed using 100% of beneficiaries continuously enrolled in Medicare FFS Parts A, and it is reported on a per 100,000 beneficiary basis.
Lastly, our NHB-to-NHW ratios, related to each of the preceding outcomes, are simply obtained by taking the ratio: \( NHB/ NHWRatio=\frac{CountyOutcomeMeasure_{Black}}{CountyOutcomeMeasure_{White}} \), where CountyOutcomeMeasureBlack captures the county-level measure for the NHB Medicare beneficiaries, and CountyOutcomeMeasureWhite captures the same measure for the NHW Medicare beneficiaries.
Network Measures
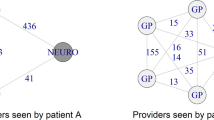
We utilize a relative degree centrality measure to capture the structure of the county-level networks. This measure is obtained by computing the average number of links for primary care physicians (PCPs) and medical and surgical specialists (Specialists) providers within a given county (this is the degree centrality), and then by calculating the ratio of these two averages. If the resulting ratio is equal to one, then this represents a network where PCPs and specialists occupy similar positions within the network, while ratios greater than one indicate that PCPs capture a more central (and coordinating) role within the network than do specialists, while a ratio less than one captures the reverse. Regarding the designation of PCPs within our data, these are defined as providers reporting a primary specialty of family practice, general practice, pediatric medicine, internal medicine, or obstetrics/gynecology within the Medicare Physician Compare registry. In terms of a more formal definition for our network measure, we define the degree centrality for provider i in network g as \( {C}_i^{degree}(g)={\eta}_i(g) \), where ηi(g) denotes the degree (or number of patient sharing relationships) of provider i in network g.23,24 Based on this definition, our relative PCP to Specialist degree centrality ratio is defined as \( R{C}^{degree}(g)=\frac{C_{PCP}^{degree}(g)}{C_{Specialist}^{degree}(g)} \). This relative degree centrality measure will be higher in counties where the PCPs occupy relatively more central positions within the local network structures. As an example, a county where PCPs have many patient sharing relationships with other providers, but where Specialist collaborations are coordinated by a central PCP (rather than between the Specialists directly), will have a higher relative PCP to Specialist degree centrality ratio than one where Specialists do not use a central coordinator for patient care. An example of our measure, and the presented intuition, can be seen within Figure 1. In Figure 1, Network A presents an example where PCPs and Specialists occupy similar positions within the network (and hence we observe a degree centrality ratio of 1), while Network B presents a case where PCPs are more central coordinators of care (resulting in a ratio of 2). Similar degree centrality ratio measures have previously been employed within hospital and regional level analysis of patient sharing networks.18,25
PCP/Specialist Centrality Ratio Example. Network A represents a network where the PCP/Specialist Centrality Ratio is equal to unity; while Network B represents one where PCPs serve a more central and coordinating role than do Specialists, and which has a PCP/Specialist Centrality Ratio equal to two.
Covariates
The county-level median household income is computed as the median of total income, and this variable is sourced from the US Census Bureau’s Small Area Income and Poverty Estimates program 2018 data. The unemployment rate is based on the percentage of the county’s civilian labor force, ages 16 and older, that is unemployed but seeking work, and this variable is obtained from 2018 Bureau of Labor Statistics data. Our diabetes prevalence measure captures the percentage of adults aged 20 and above with a diagnosis of diabetes, and it is obtained from the CDC diabetes Interactive Atlas 2016 database. Finally, we use the Census Bureau’s 2018 Population Estimates data for county measures on the percent 65 and older, percent NHB, percent females, and overall county population.
Statistical Analysis
We use multivariable regression methods in order to perform two analyses. The first estimates the adjusted disparity gap across NHW and NHB patients and identifies whether network structure effects are heterogenous across these patient populations. The second estimates the direct effect of provider network structure on our cost, utilization, and care outcome disparity gap measures. Given the inherent limitations of observational study designs, we take two steps in order to ameliorate concerns pertaining to potential confounding due to unobserved variables. First, we control for a rich set of county-level variables that have been identified as important for explaining county-level variation within our outcomes. Second, we also control for state-level fixed effects in order to control for any unobserved state-level differences that might affect both our network measure and our outcome measures, and therefore bias our estimated network effect.
In terms of the regression model specification for our first analysis, this is given by:
Here, Yir represents our county-level outcome measure of interest, \( {RC}_i^{degree} \) is the county-level average degree centrality ratio between PCPs and Specialists, NHBir is an indicator variable that takes the value of one if the outcome pertains to NHB beneficiaries, and a value of zero if it pertains to NHW beneficiaries, and \( \left({RC}_i^{degree}\ast {NHB}_{ir}\right) \) captures the interaction term between our network measure and the NHB indicator variable. Additionally, X is a vector with all of our covariates (previously defined), and ϕs captures the state fixed effects. As such, the marginal effects pertaining to our network measures (τ, γ ), and our NHW to NHB disparity gap effect (δ), are identified using within state variation conditional on the controls.
For our secondary disparity gap analysis, the regression model specification is:
Here, NHB/NHWRatioi denotes the county-level NHB to NHW disparity ratio at county i. The controls and fixed effects measures are the same as defined for the first analysis in Eq. (1).
RESULTS
County Characteristics and Between-County Variation
Table 1 provides county-level summary statistics across our outcome, network, and control variables. We see that the risk adjusted total costs per beneficiary tend to be about $1728 (p<0.001) higher for NHB Medicare beneficiaries than for NHW beneficiaries. NHB patients further have 3 (p<0.001) more hospitalizations (per 1000 beneficiaries), and 12.4 (p<0.001) more ED visits (per 1000 beneficiaries), on average. Pertaining to appropriateness of care, we see that annual A1c testing is about 1.7% (p<0.001) higher among NHW beneficiaries than among NHB beneficiaries. For the PQI measure, we note a gap of 94.96 (p<0.001) per 100,000 admissions between NHB and NHW beneficiaries.
In terms of our NHB-to-NHW ratios, we see that NHB beneficiaries have 10% higher risk adjusted total costs, 91% more hospitalizations per 1000 beneficiaries, 168% more ED visits per 1000 beneficiaries, 3% less A1c testing, and 52% more discharges for preventable complications.
For our network measures, we note that the PCP to Specialist average degree ratio is 0.85 (SD=0.53). This indicates that PCP providers on average are 15% less central than specialist providers; however, the large standard deviation further indicates significant variation within this measure across different counties.
Adjusted Disparity Gaps and Heterogenous Responses to Provider Network Structure by Race
Table 2 presents fully adjusted regression results. First, looking at the NHB coefficient estimates, we see that compared to NHW, NHB beneficiaries have on average $1673 (p<0.01) higher total costs, 2.63 (p<0.01) more hospitalizations per 1000 individuals, 11.56 (p<0.01) more ED visits per 1000 individuals, a 2.15% lower A1c testing rate, and 69.39 more avoidable hospital admissions (resulting from diabetes) per 100,000 individuals.
In terms of the effect of network structure upon our outcome measures, we see that these vary depending on race. By looking at the significance of the interaction between our network measure and the NHB indicator, we note that these network effects are significantly different (p<0.01) across four out of our five outcome measures (hospitalizations, ED visits, rate of A1c testing, and PQI). We also see that greater PCP centrality relative to Specialists appears to primarily benefit NHB patients.
Provider Network Structure and Diabetes Non-Hispanic Black-to-White Disparity Gaps
Table 3 reports results that are again adjusted for the same controls and fixed effects as those in Table 2, but which use the NHB-to-NHW average county ratios as its outcomes. From Table 3, we note that an increase in the relative centrality of PCPs compared to Specialists is associated with significantly lower disparity gaps across Hospitalizations (−0.23, p<0.01), ED visits (−0.14, p<0.05), percentage A1c testing (0.01, p<0.01), and PQI (−0.14, p<0.1).
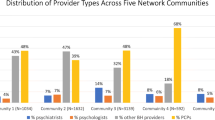
If we combine these point estimates (related to the disparity ratio change) with the actual NHB-to-NHW disparity ratios (estimated within Table 2) then we can compute the percentage decrease (of these disparity gaps) that result from a one standard deviation increase in the relative centrality of PCPs to Specialists. It is worth noting that a one standard deviation increase within our data represents us on average moving from a network structure where Specialists are more central in terms of the patient sharing network to one where the reverse is true, that is, one where PCPs are more central in terms of patient sharing than Specialists. The result of such a change is presented in Figure 2. Here we see that increasing the PCP/Specialist degree centrality ratio by one standard deviation is associated with a disparity gap decrease of 25.3% (p<0.01) in Hospitalizations, 8.3% (p<0.05) in ED visits, 2.8% (p<0.01) in A1c testing, and 26.9% (p<0.1) in the volume of preventable diabetes-related hospital admissions. As such, we note a significant association between network structure and NHB-to-NHW disparity gaps.
LIMITATIONS AND ROBUSTNESS
Three particular study limitations are important to highlight. First, given the observational design of this study, and the fact that this is not a patient level analysis, we are unable to make claims of causality. As such, these effects are to be interpreted as important associations that we believe deserve further exploration. With that said, it is also important to highlight that our results do condition on a number of county-level covariates, along with state-level fixed effects.
Second, the choice of network structure measure may importantly matter for the results one obtains. In order to explore the sensitivity of our results to the choice of our PCP/Specialist degree ratio, we also performed an analysis using a pure PCP degree centrality measure. Using this alternative network measure yields qualitatively similar results, and these are reported within the Supplementary Appendix B.
Third, the definition of a provider network based on a set organizational structure, or geographical unit, is inherently challenging as this definition may influence what patient sharing relationships (between providers) that are (and are not) accounted for within the final analysis. This is a limitation that holds for this literature at large; however, in order to explore the sensitivity of our results to the geographical level at which we define our networks, we also explored defining these networks at a Hospital-Referral-Region level. Using this approach, we compute provider-specific degree centrality measures at the Hospital-Referral-Region and then obtain averages on a county-by-county basis. The results from this exercise show qualitatively similar results to those presented within the main text and can be found within Supplementary Appendix C.
DISCUSSION
This study finds that there exists a significant relationship between the structure of regional provider networks, based on shared patient relationships, and the county-level cost, utilization, and appropriateness of care that Medicare beneficiaries with diabetes receive. These findings contribute to the growing literature concerned with mapping out the relationship between network structure and patient outcomes,18,25,26,27,28,29 as well as the literature on regional variations in health care outcomes.30,31,32,33,34 We also document that outcomes for NHB beneficiaries seem more sensitive to the underlying provider network structures than do NHW Medicare beneficiaries, and perhaps most interesting, that there exists a significant association between county-level provider network structure and NHB-to-NHW disparity gaps for Medicare beneficiaries with a diabetes diagnosis. These findings in turn contribute to a broad literature on racial disparities in health care.35,36,37
The presented work suggests a number of research avenues for future work. First is the question about the mechanism through which network structures act to reduce costs and improve care outcomes. Second is the question of how certain network structures act to reduce NHB-to-NHW disparity gaps. Are the observed disparities between NHB and NHW Medicare patients driven by beneficiaries having access to different local provider networks? Or, perhaps these findings may suggest a link between network structure and what we have come to learn from the literature on bias within the medical profession.38,39 Lastly, it is important to explore the effect that current policies and industry-wide trends in terms of Medical Home Model and Accountable Care Organization adoption, or horizontal hospital mergers and vertical practice to system integrations, have on not only health outcomes, but also on the noted racial disparity gaps. Additionally, it appears important to further explore the degree to which regional differences within these trends help explain some of the network structure differences that we have noted with the present study.
In summary, these findings suggest that how we organize and structure our health systems may have important implications for disparity gaps between NHB and NHW Medicare beneficiaries with a diagnosis of diabetes.
References
Centers for Disease Control and Prevention. National diabetes statistics report, 2020. Centers for Disease Control and Prevention: Atlanta, 2020. Accessed from: https://www.cdc.gov/diabetes/library/features/diabetes-stat-report.html. Accessed on: December, 16, 2020.
Dieleman JL, Baral R, Birger M, et al. US spending on personal health care and public health, 1996-2013. JAMA 2016;316(24):2627–46.
American Diabetes Association. Statistics about diabetes: overall numbers. American Diabetes Association: Arlington. 2020. Accessed from: https://www.diabetes.org/resources/statistics/statistics-about-diabetes#:~:text=Prevalence%3A%20In%202018%2C%2034.2%20million,of%20the%20population%2C%20had%20diabetes.&text=Undiagnosed%3A%20Of%20the%2034.2%20million,and%207.3%20million%20were%20undiagnosed. Accessed on: September 24, 2020.
Centers for Disease Control and Prevention. Prevalence of both diagnosed and undiagnosed diabetes. Centers for Disease Control and Prevention. 2020. Accessed from: https://www.cdc.gov/diabetes/data/statistics-report/diagnosed-undiagnosed-diabetes.html Accessed on: December, 16, 2020.
Rosenstock S, Whitman S, West JF, Balkin M. Racial Disparities in Diabetes Mortality in the 50 Most Populous US Cities. J Urban Health 2014;91(5):873–85.
Mansour O, Golden SH, Yeh HC. Disparities in mortality among adults with and without diabetes by sex and race. J Diabetes Complicat 2020;34(3):107496.
Centers for Medicare & Medicaid Services. Racial and Ethnic Disparities in the Diabetes Prevalence, Self-Management, and Health Outcomes among Medicare Beneficiaries. Centers for Medicare & Medicaid Services. 2017. Accessed from: https://www.cms.gov/About-CMS/Agency-Information/OMH/Downloads/March-2017-Data-Highlight.pdf Accessed on: December, 16, 2020
Davis J, Lim E, Taira DA, Chen J. Relation of the networks formed by diabetic patients sharing physicians with emergency department visits and hospitalizations. Med Care 2020;58(9):800–4.
Solberg L, Carlin C, Peterson K, Milton E. Differences in Diabetes Care With and Without Certification as a Medical Home. Ann Fam Med 2020;18(1):66–72.
Shrivastav M, Gibson W, Shrivastav R, et al. Type 2 diabetes management in primary care: The role of retrospective, professional continuous glucose monitoring. Diabetes Spectrum 2018;31(3):279–87.
McWilliams JM, Chernew ME, Landon BE, Schwartz AL. Performance Differences in Year 1 of Pioneer Accountable Care Organizations. N Engl J Med 2015;372(20):1927–36.
Agha L, Frandsen B, Rebitzer JB. Fragmented division of labor and healthcare costs : Evidence from moves across regions. J Public Econ 2019;169:144–59.
Brigham R. Frandsen P, Karen E, Joynt MM, James B, Rebitzer P, and Ashish K, Jha MM. Care Fragmentation, Quality, and Costs Among Chronically Ill Patients. Am J Manag Care 2015;21(May 2015 5):355–62.
Centers For Medicare and Medicaid Services. Mapping Medicare Disparities 2016 Data . 2020; Accessed from: https://data.cms.gov/mapping-medicare-disparities. Accessed on: December, 16, 2020.
NORC at the University of Chicago. The Mapping Medicare Disparities Tool: Technical Documentation. 2020.
Dartmouth Atlas Project. Selected Primary Care Access and Quality Measures. Accessed from: https://www.dartmouthatlas.org/interactive-apps/primary-care-access-quality-measures/ Accessed on: December, 16, 2020
CareSet Systems. Medicare Patient Sharing Data . 2020; Accessed from: https://careset.com/datasets/ Accessed on: December, 16, 2020.
Barnett ML, Christakis NA, O’Malley J, Onnela JP, Keating NL, Landon BE. Physician patient-sharing networks and the cost and intensity of care in US hospitals. Med Care 2012;50(2):152–60.
Linde S. The formation of physician patient sharing networks in medicare: Exploring the effect of hospital affiliation. Health Econ 2019;28(12):1435–48.
Centers for Medicare and Medicaid Services. Physician Compare Datasets . 2020; Accessed from: https://data.medicare.gov/data/physician-compare Accessed on: December, 16, 2020.
County Health Rankings and Roadmaps. Data & Documentation. 2020. Accessed from: https://www.countyhealthrankings.org/explore-health-rankings/measures-data-sources Accessed on: December, 16, 2020.
Centers for Medicare and Medicaid Services. Risk Adjustment 2015 Model Software. 2020; Accessed from: https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Risk-Adjustors-Items/Risk2015?DLPage=1&DLEntries=10&DLSort=0&DLSortDir=descending Accessed on: December, 16, 2020
Jackson MO. Social and economic networks. Princeton university press; 2010.
Goyal S. Connections: an introduction to the economics of networks. Princeton University Press; 2012.
Landon BE, Keating NL, Onnela JP, Zaslavsky AM, Christakis NA, James O’Malley A. Patient-sharing networks of physicians and health care utilization and spending among medicare beneficiaries. JAMA Intern Med 2018;178(1):66–73.
Barnett ML, Landon BE, O’Malley AJ, Keating NL, Christakis NA. Mapping physician networks with self-reported and administrative data. Health Serv Res 2011;46(5):1592–609.
Geissler KH, Lubin B, Marzilli Ericson KM. The association between patient sharing network structure and healthcare costs. PLoS One 2020;15(6 June):1–13.
Pollack CE, Weissman G, Bekelman J, Liao K, Armstrong K. Physician social networks and variation in prostate cancer treatment in three cities. Health Serv Res 2012;47(1 PART 2):380–403.
Pollack CE, Wang H, Bekelman JE, et al. Physician Social Networks and Variation in Rates of Complications after Radical Prostatectomy. Value Health 2014;17(5):611–8.
Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder ÉL. The Implications of Regional Variations in Medicare Spending. Part 1: The Content, Quality, and Accessibility of Care. Ann Intern Med 2003;138(4):273–87.
Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder ÉL. The implications of regional variations in Medicare spending. Part 2: Health outcomes and satisfaction with care. Ann Intern Med 2003;138(4):288–98.
Walker RJ, Neelon B, Davis M, Egede LE. Racial differences in spatial patterns for poor glycemic control in the Southeastern United States. Ann Epidemiol 2018;28(3):153–9.
Egede LE, Gebregziabher M, Hunt KJ, et al. Regional, geographic, and ethnic differences in medication adherence among adults with type 2 diabetes. Ann Pharmacother 2011;45(2):169–78.
Egede LE, Gebregziabher M, Hunt KJ, et al. Regional, geographic, and racial/ethnic variation in glycemic control in a national sample of veterans with diabetes. Diabetes Care 2011;34(4):938–43.
Simmons M, Bishu KG, Williams JS, Walker RJ, Dawson AZ, Egede LE. Racial and Ethnic Differences in Out-of-Pocket Expenses among Adults with Diabetes. J Natl Med Assoc 2019;111(1):28–36.
Ozieh MN, Bishu KG, Dismuke CE, Egede LE. Trends in health care expenditure in U.S. adults with Diabetes: 2002-2011. Diabetes Care 2015;38(10):1844–51.
Dawson AZ, Bishu KG, Walker RJ, Egede LE. Trends in Medical Expenditures by Race/Ethnicity in Adults with Type 2 Diabetes 2002-2011. J Natl Med Assoc 2020;1–10.
Rathore SS, Lenert LA, Weinfurt KP, et al. The effects of patient sex and race on medical students’ ratings of quality of life. Am J Med 2000;108(7):561–6.
Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci U S A 2016;113(16):4296–301.
Acknowledgements
SL and LEE designed the study. SL acquired and analyzed the data. SL drafted the manuscript. LEE reviewed and revised the manuscript. All authors critically revised for intellectual content and approved the final manuscript.
SL and LEE are guarantors of the work.
Effort for this study was partially supported by the National Institute of Diabetes and Digestive Kidney Disease (K24DK093699, R01DK118038, R01DK120861, PI: Egede) and the National Institute for Minority Health and Health Disparities (R01MD013826, PI: Egede/Walker).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 111 kb)
Rights and permissions
About this article
Cite this article
Linde, S., Egede, L.E. Provider Network Structure and Black-to-White Disparity Gaps for Medicare Patients with Diabetes: County-Level Analysis of Cost, Utilization, and Clinical Care. J GEN INTERN MED 37, 753–760 (2022). https://doi.org/10.1007/s11606-021-06975-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-06975-3