Abstract
Background
Older adults with diabetes rarely have only one chronic disease. As a result, there is a need to re-conceptualize research and clinical practice to address the growing number of older Americans with diabetes and concurrent chronic diseases (diabetes-multimorbidity).
Objective
To identify prevalent multimorbidity combinations and examine their association with poor functional status among a nationally representative sample of middle-aged and older adults with diabetes.
Design
A prospective cohort study of the 2012–2014 Health and Retirement Study (HRS) data. We identified the most prevalent diabetes-multimorbidity combinations and estimated negative binomial models of diabetes-multimorbidity on prospective disability.
Participants
Analytic sample included 3841 HRS participants with diabetes, aged 51 years and older.
Main Measures
The main outcome measure was the combined activities of daily living (ADL)-instrumental activities of daily living (IADL) index (range 0–11; higher index denotes higher disability). The main independent variables were diabetes-multimorbidity combination groups, defined as the co-occurrence of diabetes and at least one of six somatic chronic diseases (hypertension, cardiovascular disease, lung disease, cancer, arthritis, and stroke) and/or two mental chronic conditions (cognitive impairment and high depressive symptoms (CESD score ≥ 4).
Key Results
The three most prevalent multimorbidity combinations were, in rank-order diabetes-arthritis-hypertension (n = 694, 18.1%); diabetes-hypertension (n = 481, 12.5%); and diabetes-arthritis-hypertension-heart disease (n = 383, 10%). Diabetes-multimorbidity combinations that included high depressive symptoms or stroke had significantly higher counts of ADL-IADL limitations compared with diabetes-only. In head-to-head comparisons of diabetes-multimorbidity combinations, high depressive symptoms or stroke added to somatic multimorbidity combinations was associated with a higher count of ADL-IADL limitations (diabetes-arthritis-hypertension-high depressive symptoms vs. diabetes-arthritis-hypertension: IRR = 1.95 [1.13, 3.38]; diabetes-arthritis-hypertension-stroke vs. diabetes-arthritis-hypertension: IRR = 2.09 [1.15, 3.82]) even after adjusting for age, gender, education, race/ethnicity, BMI, baseline ADL-IADL, and diabetes duration. Coefficients were robust to further adjustment for diabetes treatment.
Conclusions
Depressive symptoms or stroke added onto other multimorbidity combinations may pose a substantial functional burden for middle-aged and older adults with diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
For older adults with diabetes, having at least one additional concurrent chronic disease is common.1 Over 80% of patients with diabetes have multimorbidity,2 and the number of co-existing diseases increases with age.3 The complex interactions of biological and non-biological factors in diabetes argue for a re-conceptualization of research and clinical practice to address the growing number of older Americans with diabetes.4 In 2013, the American Diabetes Association and the American Geriatrics Society recognized critical gaps in current diabetes knowledge around older adults with diabetes and other concurrent conditions (diabetes-multimorbidity).5 Their recommendations centered on clarifying the epidemiology of diabetes and developing evidence to support optimal care for older patients with complex disease profiles.
The complexity of caring for patients with diabetes-multimorbidity has been previously recognized6, 7 and attributed to several reasons. First, specific diabetes-multimorbidity combinations may affect patients’ ability to perform self-management activities, resulting in suboptimal diabetes control.1 Second, individuals with diabetes are at higher risk of developing mental health conditions. Rates of depression are two times greater for people with diabetes compared with those of the general population.8 Combinations of somatic and mental health conditions may impair physical function and interfere with lifestyle/medication regimen adherence.1 Third, focus on individual diseases may miss interactions between diseases and the complexities of polypharmacy. Fourth, older adults with long-standing diabetes-multimorbidity may vary substantially from those with newly diagnosed disease, further complicating treatment algorithms.5
Diabetes necessitates self-vigilance to maintain adequate glycemic control and avert diabetes-related complications. However, the challenges of having specific diabetes-multimorbidity combinations are less understood. The US Department of Health and Human Services recommended the identification of specific disease combinations and comparison of similar multimorbidity patterns as critical next steps. Because the identification of all multimorbidity permutations is infeasible and potentially uninformative, examining prevalent and clinically meaningful chronic diseases remains the recommended approach.2, 9,10,11
Overall, individuals with multimorbidity are more likely to develop functional limitations leading to premature disability and death, and specific combinations may signal high disability burdens.12 The purpose of our study is to evaluate the association between prevalent diabetes-multimorbidity combinations and prospective disability in a nationally representative sample of middle-aged and older Americans. Understanding how diabetes-multimorbidity combinations influence the functional status of older adults is of particular importance, given the high prevalence and growing economic liability of diabetes and multimorbidity in this population.
METHODS
Data
The Health and Retirement Study (HRS) is a nationally representative biennial survey of non-institutionalized middle-aged and older adults (51 years and older). HRS survey waves 2012–2014 were used in this study.
Population
Of the 18,851 respondents in 2012 and 17,090 respondents in 2014 who were alive, not in nursing homes, and cohort eligible, 16,501 respondents were surveyed in both waves. We excluded 522 participants with proxy interviews in 2012 because they were not asked the depressive symptoms battery of questions; 11,927 participants who had not reported a diabetes diagnosis by 2012; and 211 participants who reported fewer than two chronic conditions. The final analytic sample included 3841 respondents with diabetes-multimorbidity.
Variables
Functional Status
Respondents were asked about difficulty performing a variety of everyday tasks to assess physical function, including (1) Nagi items, such as walking several blocks, climbing stairs, and pushing a heavy object; (2) activities of daily living (ADL), including dressing, walking across a room, eating, bathing, toileting, and transferring from bed; and, (3) instrumental activities of daily living (IADL), including meal preparation, grocery shopping, using a telephone, taking medication, and managing money.
ADL Index
Nagi items were used to determine if respondents should be routed to ADL questions. Respondents reporting no difficulties with Nagi items were not asked about ADLs. Respondents reporting one Nagi item difficulty but no difficulty dressing were not asked any additional ADL questions. These respondents were defined as having no ADL disability. The remaining respondents were asked all ADL questions and were defined as having a specific ADL disability if (1) the respondent reported difficulty with the ADL due to a health or memory problem or (2) the respondent needed help with the ADL. We created an ADL index, representing the count of ADL disabilities for each respondent who had a least one non-missing ADL response (range 0–6; higher number indicates higher ADL disability).
IADL Index
All respondents were asked about difficulty with IADLs. Each IADL disability was defined as (1) difficulty performing the IADL due to a health or memory problem, (2) not performing the IADL due to a health or memory problem, or (3) needing help to perform the IADL. We created an IADL index, representing the count of IADL disabilities for each respondent who had at least one non-missing IADL response (range 0–5; higher number indicates higher IADL disability).
ADL-IADL Index
The primary outcome variable, ADL-IADL index, was created by summing ADL and IADL indices (range 0–11; higher number indicates higher disability). Combining the ADL and IADL domains into a single index captures a greater range of functional disability prevalence and has been previously described and validated in studies of disability among older adults.13,14,15
Chronic Disease
Seven self-reported, physician-diagnosed chronic diseases, each prompted by “Has a doctor ever told you that you have…,” were included: heart disease (myocardial infarction, coronary heart disease, angina, congestive heart failure, or other heart problems); hypertension (i.e., high blood pressure); stroke (but not TIA); diabetes; arthritis; lung disease (including chronic bronchitis or emphysema, and excluding asthma); and cancer (any malignant tumors, except skin cancer). We defined respondents as having the chronic disease if they reported a diagnosis prior to or in the 2012 wave.
Two mental chronic conditions were included: high depressive symptoms and cognitive impairment. Concordant with HRS data user guides and previous studies, four or more responses indicating a depressive effect on the CESD instrument were defined as having high depressive symptomatology.16, 17 Cognitive ability was assessed using a multidimensional measure of cognitive function, based on the Telephone Interview for Cognitive Status. In accordance with HRS data user guide criteria and prior studies, cognitive impairment was defined as a score of 10 or less on a 35-point scale for respondents aged 65 and older, and a score of 5 or less on a 27-point scale for respondents aged 51–64.18,19,20,21
Treatment and Duration of Diabetes
Respondents were defined as undergoing treatment for diabetes if they responded “yes” to at least one of the following questions: “In order to treat or control your diabetes, are you now taking medication that you swallow?” or “Are you now using insulin shots or a pump?”. Respondents were asked “In what year was your diabetes first diagnosed?” The duration of respondent’s diabetes diagnosis was calculated by subtracting the year of diagnosis from 2012.
Covariates
Sociodemographic covariates measured in 2012 included age (years), female gender, education (years), and race/ethnicity (mutually exclusive indicator variables). Body mass index was calculated according to the established formula (BMI = weight [pounds] × 703 / height^2 [inches]) using first self-reported height (HRS does not record height at follow-up) and self-reported weight.
Analysis
Characteristics of the study population were summarized using frequencies and percentages for categorical variables, and means and standard deviations for continuous variables. To assess the relationship between multimorbidity in 2012 and ADL-IADL disability in 2014, groups of respondents with similar combinations of diabetes plus one or more additional chronic diseases in 2012 were identified and ranked according to their frequency. We calculated each group’s mean ADL-IADL index. An a priori criterion of ≥ 1.5% prevalence in the study population for the multimorbidity groups was chosen to ensure sufficient sample size in each multimorbidity group. Sequentially adjusted negative binomial regression models were used to evaluate the count of ADL-IADL disabilities for various diabetes-multimorbidity combinations, as well as account for overdispersion. To control for multiple comparisons, we employed the Benjamini-Hochberg procedure in which our uncorrected α-level was 0.050 and our corrected α-level was 0.029.22
To investigate the incremental burden of disability associated with multimorbidity in individuals with diabetes, we compared the ADL-IADL index in each diabetes-multimorbidity group with the ADL-IADL index in respondents with diabetes-only and respondents with diabetes and one additional disease within their multimorbidity combination. Subsequently, we compared the count of ADL-IADL disabilities between specific diabetes-multimorbidity groups. For each comparison, the following models were tested: (1) unadjusted, (2) minimally adjusted (age, gender, education, race/ethnicity, and BMI), and (3) fully adjusted (additionally adjusted by baseline ADL-IADL index and diabetes duration). Finally, sensitivity analyses were performed to account for potential confounding associated with medication treatment for diabetes. For all analyses, model coefficients represent the log of the ratio of expected ADL-IADL counts. The exponentiated coefficients comparing the ADL-IADL index between diabetes-multimorbidity combination groups should be interpreted as follows: “A is expected to have an ADL-IADL disability count X.XX times greater than B”. Exponentiated coefficients and 95% confidence intervals are reported.
The HRS over-samples African-Americans, Hispanics, and older individuals from Florida. Thus, we present weighted multivariate analyses to account for the complex survey design. All analyses were conducted in STATA/SE 13.1 (StataCorp, College Station, TX).
RESULTS
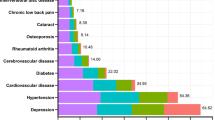
The study sample (Table 1) consisted of 3841 middle-aged and older adults with diabetes-multimorbidity, with a mean age of 68 years (SD = 9.5). Fifty-six percent of the participants were female, 54% were non-Hispanic white, and the mean number of chronic conditions was 3.7 (SD = 1.3). Table 2 presents the 17 most prevalent diabetes-multimorbidity combinations (with ≥ 1.5% prevalence in the study sample) and corresponding mean number of ADL-IADL limitations. The most prevalent combination was diabetes-arthritis-hypertension (n = 694), followed by diabetes-hypertension (n = 481), and diabetes-arthritis-hypertension-heart disease (n = 383). Four of the combinations included high depressive symptomatology (groups 5, 8, 11, and 17).
Table 3 presents comparisons between the ADL-IADL indices of each diabetes-multimorbidity group and respondents with diabetes-only and respondents with diabetes and one additional disease within their multimorbidity combination. Overall, fully adjusted models that indicate 13 of the 17 most prevalent diabetes-multimorbidity combinations were associated with significantly higher ADL-IADL disability compared with diabetes-only. Groups 5, 13, and 17 had the highest prospective ADL-IADL index compared with diabetes-only in the fully adjusted models (IRRs = 8.24, 12.23, and 18.15, respectively). Compared to having diabetes and one additional disease in the combination was associated with greater ADL-IADL disability in four diabetes-multimorbidity combinations: groups 5, 11, 13, and 17.
Table 4 presents nested and head-to-head comparisons of diabetes-multimorbidity combinations for model specifications 1–3 (unadjusted to fully adjusted). Estimated coefficients across unadjusted and minimally adjusted models were generally similar across comparisons, with large attenuations occurring upon final adjustment for baseline ADL-IADL index and diabetes duration.
Mental-Somatic vs Somatic Combinations
The addition of high depressive symptoms to less complex combinations of somatic conditions was associated with greater ADL-IADL limitations. In nested comparisons, added high depressive symptoms to diabetes and hypertension (group 11 vs. group 2) resulted in 3.55 times greater ADL-IADL limitations in the fully adjusted model (CI = 1.67, 7.56). Similarly, added high depressive symptoms to diabetes-arthritis-hypertension (group 5 vs. group 1) were associated with 1.95 times greater ADL-IADL limitations in the fully adjusted model (CI = 1.13, 3.38).
Mental-Somatic vs. Somatic-Stroke
The addition of high depressive symptoms and stroke, respectively, to identical somatic combinations, was associated with statistically similar findings. Head-to-head comparison of group 5 (high depressive symptoms added to the combination of diabetes-arthritis-hypertension) and group 15 (stroke added to the same combination) or group 8 (high depressive symptoms added to diabetes-arthritis-hypertension-heart disease) against group 13 (stroke added to the same combination) showed no significant difference in ADL-IADL limitations across model specifications.
Somatic-Stroke vs. Somatic
Nested comparisons between group 15 and group 1 indicated that the addition of stroke to the combination of diabetes-arthritis-hypertension was associated with 2.09 times greater ADL-IADL limitations in the fully adjusted model (CI = 1.15, 3.82). The nested comparison of added stroke to the combination of diabetes-arthritis-hypertension-heart disease (group 13 vs. group 3) indicated 2.30 times greater ADL-IADL limitations in the fully adjusted model (CI = 1.36, 3.88).
Somatic-Heart vs. Somatic
Nested comparisons involving added heart disease to various combinations of diabetes-arthritis-hypertension-cancer (group 6); diabetes-arthritis-hypertension-lung disease (group 10); and diabetes-arthritis-hypertension-stroke (group 16) yielded non-significant findings.
Nested Mental-Somatic Combinations
The nested comparisons of added arthritis to the combination of diabetes-hypertension-high depressive symptoms (group 5 vs. group 11) and added heart disease to the combination of diabetes-arthritis-hypertension-high depressive symptoms (group 8 vs. group 5) indicated no incremental burden of ADL-IADL limitations associated with the more complex combinations after full covariate adjustment.
Sensitivity Analyses
Sensitivity analyses of model specifications adjusted for diabetes treatment were conducted but were not substantively different from our fully adjusted model findings, indicating incremental and non-significant contribution of this factor (not presented, available upon request).
DISCUSSION
This study adds to our understanding of the challenges facing adults living with diabetes by identifying multimorbidity combinations associated with greater disability in mid- and late-life. We found that disease combinations with high depressive symptoms or stroke were associated with greatest prospective ADL-IADL disability compared with diabetes-only and diabetes plus one additional component disease in the combination, across models that progressively adjusted for sociodemographic characteristics, baseline functional status, and diabetes duration. In comparing prevalent diabetes-multimorbidity combinations to each other, we also found that combinations that included high depressive symptoms or stroke were associated with greater numbers of ADL-IADL limitations relative to nested or similar somatic combinations.
Our findings highlight several points. When comparing mental-somatic to somatic-only combinations, the addition of depressive symptoms to a less complex combination of somatic conditions has a substantial negative impact on functional status. Older adults with more complex somatic combinations had similar levels of disability with or without the addition of high depressive symptoms. In addition, we found penalties to function in combinations of stroke and other somatic conditions, even among already complex combinations of disease. The triangular relationship between diabetes, depression or stroke, and disability has been previously investigated. Prior studies reported higher risk of disability and lower likelihood of recovery from disability after stroke among patients with diabetes,23,24,25 as well as a substantially higher risk of disability among patients with diabetes and major depression (compared with diabetes-only and/or depression-only).26, 27 To our knowledge, this is the first study to estimate the incremental functional burden of added stroke or depressive symptoms in the context of prevalent multimorbidity combinations in patients with diabetes. This is of particular importance given that multimorbidity, depressive disorders, and stroke are highly prevalent among older adults with diabetes8, 28,29,30 and are associated with poor self-management and negative individual health outcomes,28, 31 and with increased healthcare utilization and expenditures.32, 33 Thus, identifying specific disease combinations to target for screening and treatment of depression, stroke prevention, and post-stroke rehabilitation may help maintain or improve functional status for older patients with diabetes.
Our results show limited functional impact of heart disease added onto other diabetes-multimorbidity combinations. We hypothesize that “survivor bias” due to differences in the severity of concomitant potentially life-shortening conditions may account for these puzzling results. In other words, individuals who experience less severe/advanced life-limiting disease in their respective combinations are more likely to survive long enough to develop heart disease.
This study draws from a number of strengths. First, the HRS provides a long-standing, ongoing, and robust longitudinal dataset generalizable to the US population of adults 51 and older. Second, the prospective design of the HRS permits assessment of time-sequencing between multimorbidity combinations and the main dependent variable (ADL-IADL disability). Third, this study contributes to the emerging literature on multimorbidity among individuals living with diabetes, by identifying and comparing the most prevalent diabetes-multimorbidity combinations as they occur in a nationally representative sample, an improvement over prior work that examines single diseases in isolation, total disease counts, or pre-specified dyads/triads of co-occurring diseases. Our study contributes to this evolving literature by comparing prevalent and clinically meaningful diabetes-multimorbidity groupings, to identify the combinations that pose the greatest risk to the preservation of functional status and may, in turn, cascade to rapid loss of independence and institutionalization.
This study also has several limitations. Severity of disease is notoriously difficult to ascertain from self-reported data and across the multitude of diagnoses and combinations.34 While we account for aspects of severity via diabetes duration and treatment, future iterations need to incorporate severity in the context of multimorbidity. In addition, individuals with more severe combinations of diabetes-multimorbidity may have disproportionately died prior to being captured in the study population, introducing severity-related mortality bias. Finally, this study assessed a limited observation period of two interview waves. Comprehensive long-term longitudinal studies of multimorbidity progression and differential mortality are needed to better understand the functional burden associated with diabetes-multimorbidity combinations.
Recent advancements provide clinical insights into the functional consequences of specific multimorbidity combinations with diabetes.1, 2, 11, 35, 36 This knowledge is essential in order to design interventions and optimize the clinical care for patients with diabetes-multimorbidity.8 Our research highlights the importance of depressive disorders and stroke within larger multimorbidity combinations in patients with diabetes. Our results may help focus clinical management targets, and broker conversations between patients and clinicians regarding screening, prevention, and treatment priorities, particularly for mental disorders and vascular brain events that portend vast functional burdens and threaten functional independence. The prevalence of patients with diabetes-multimorbidity is increasing in the USA and worldwide, raising important questions regarding the organization and delivery of care for chronic conditions that carry a high functional penalty and may be difficult to manage in older adult populations.
References
Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29(3):725–31.
Magnan EM, Bolt DM, Greenlee RT, Fink J, Smith MA. Stratifying patients with diabetes into clinically relevant groups by combination of chronic conditions to identify gaps in quality of care. Health Serv Res. 2018;53(1):450–68.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the Concepts of Disability, Frailty, and Comorbidity: Implications for Improved Targeting and Care. J Gerontol A Biol Sci Med Sci. 2004;59(3):M255–63.
Tinetti ME, Fried T. The end of the disease era. Am J Med. 2004;116(3):179–85.
Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, Halter JB, et al. Diabetes in older adults. Diabetes Care. 2012;35(12):2650–64.
Kerr EA, Heisler M, Krein SL, Kabeto M, Langa KM, Weir D, et al. Beyond comorbidity counts: how do comorbidity type and severity influence diabetes patients’ treatment priorities and self-management? J Gen Intern Med. 2007;22(12):1635–40.
Huang ES. Management of diabetes mellitus in older people with comorbidities. BMJ. 2016;353:i2200.
Ducat L, Philipson LH, Anderson BJ. The Mental Health Comorbidities of Diabetes. JAMA. 2014;312(7):691–2.
Goodman RA, Posner S, Huang ES, Parekh AK, Koh HK. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev Chronic Dis. 2013;10:E66.
Goodman RA, Ling SM, Briss PA, Parrish RG, Salive ME, Finke BS. Multimorbidity Patterns in the United States: Implications for Research and Clinical Practice. J Gerontol Biol Sci Med Sci. 2016;71(2):215–20.
Quiñones AR, Markwardt S, Thielke S, Rostant O, Vásquez E, Botoseneanu A. Prospective Disability in Different Combinations of Somatic and Mental Multimorbidity. J Gerontol Ser A. 2018;73(2):204–10.
Vogeli C, Shields AE, Lee TA, Gibson TB, Marder WD, Weiss KB, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. 2007;22 Suppl 3:391–5.
Spector WD, Fleishman JA. Combining activities of daily living with instrumental activities of daily living to measure functional disability. J Gerontol B Psychol Sci Soc Sci. 1998;53(1):S46–57.
Thomas VS, Rockwood K, McDowell I. Multidimensionality in Instrumental and Basic Activities of Daily Living. J Clin Epidemiol. 1998;51(4):315–21.
Liang J, Bennett JM, Shaw BA, Quiñones AR, Ye W, Xu X, et al. Gender differences in functional status in middle and older age: are there any age variations? J Gerontol B Psychol Sci Soc Sci. 2008;63(5):S282–92.
Steffick DE. Documentation of affective functioning measures in the Health and Retirement Study. Ann Arbor, Michigan: Institute for Social Research, University of Michigan; 2000.
Quiñones AR, Markwardt S, Botoseneanu A. Multimorbidity Combinations and Disability in Older Adults. J Gerontol Med Sci. 2016;71(6):823–30.
Ofstedal MB, Fisher GG, Herzog AR. Documentation of cognitive functioning measures in the Health and Retirement Study. Ann Arbor, Michigan: Institute for Social Research, University of Michigan; 2005.
Crimmins EM, Kim JK, Langa KM, Weir DR. Assessment of Cognition Using Surveys and Neuropsychological Assessment: The Health and Retirement Study and the Aging, Demographics, and Memory Study. J Gerontol Ser B. 2011;66B(suppl_1):i162–71.
Langa KM, Larson EB, Crimmins EM, Faul JD, Levine DA, Kabeto MU, et al. A comparison of the prevalence of dementia in the United States in 2000 and 2012. JAMA Intern Med. 2017;177(1):51–8.
Cook SE, Marsiske M, McCoy KJM. The use of the modified Telephone Interview for Cognitive Status (TICS-M) in the detection of amnestic mild cognitive impairment. J Geriatr Psychiatry Neurol. 2009;22(2):103–9.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol. 1995;57(1):289–300.
Megherbi S-E, Milan C, Minier D, Couvreur G, Osseby G-V, Tilling K, et al. Association between diabetes and stroke subtype on survival and functional outcome 3 months after stroke: data from the European BIOMED stroke project. Stroke. 2003;34(3):688–94.
Otiniano ME, Du XL, Ottenbacher K, Markides KS. The effect of diabetes combined with stroke on disability, self-rated health, and mortality in older Mexican Americans: results from the Hispanic EPESE. Arch Phys Med Rehabil. 2003;84(5):725–30.
Newman GC, Bang H, Hussain SI, Toole JF. Association of diabetes, homocysteine, and HDL with cognition and disability after stroke. Neurology. 2007;69(22):2054–62.
Egede LE. Diabetes, major depression, and functional disability among U.S. adults. Diabetes Care. 2004;27(2):421–8.
Black SA, Markides KS, Ray LA. Depression predicts increased incidence of adverse health outcomes in older mexican americans with type 2 diabetes. Diabetes Care. 2003;26(10):2822–8.
Lin P-J, Kent DM, Winn A, Cohen JT, Neumann PJ. Multiple chronic conditions in type 2 diabetes mellitus: prevalence and consequences. Am J Manag Care. 2015;21(1):e23–34.
Finkelstein EA, Bray JW, Chen H, Larson MJ, Miller K, Tompkins C, et al. Prevalence and costs of major depression among elderly claimants with diabetes. Diabetes Care. 2003;26(2):415–20.
Peters SAE, Huxley RR, Woodward M. Diabetes as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 64 cohorts, including 775 385 individuals and 12 539 strokes. The Lancet. 2014;383(9933):1973–80.
Schmitt A, Reimer A, Hermanns N, Kulzer B, Ehrmann D, Krichbaum M, et al. Depression is linked to hyperglycaemia via suboptimal diabetes self-management: A cross-sectional mediation analysis. J Psychosom Res. 2017;94:17–23.
Egede LE, Walker RJ, Bishu K, Dismuke CE. Trends in costs of depression in adults with diabetes in the United States: medical expenditure panel survey, 2004-2011. J Gen Intern Med. 2016;31(6):615–22.
Gruneir A, Markle-Reid M, Fisher K, Reimer H, Ma X, Ploeg J. Comorbidity burden and health services use in community-living older adults with diabetes mellitus: a retrospective cohort study. Can J Diabetes. 2016;40(1):35–42.
Boyd CM, Weiss CO, Halter J, Han KC, Ershler WB, Fried LP. Framework for Evaluating disease severity measures in older adults with comorbidity. J Gerontol Ser A. 2007;62(3):286–95.
Calderón-Larrañaga A, Abad-Díez JM, Gimeno-Feliu LA, Marta-Moreno J, González-Rubio F, Clerencia-Sierra M, et al. Global health care use by patients with type-2 diabetes: Does the type of comorbidity matter? Eur J Intern Med. 2015;26(3):203–10.
Chima CC, Salemi JL, Wang M, Mejia de Grubb MC, Gonzalez SJ, Zoorob RJ. Multimorbidity is associated with increased rates of depression in patients hospitalized with diabetes mellitus in the United States. J Diabetes Complications. 2017;31(11):1571–9.
Funding
This study was supported by the American Diabetes Association career development award (ADA 7-13-CD-08 to ARQ) and the National Institute on Aging of the National Institutes of Health award (R01AG055681 to ARQ; AG-024824 and UL1TR000433 support for AB).
Author information
Authors and Affiliations
Contributions
ARQ contributed to the literature search, study design, data interpretation, and drafting of the manuscript. AB contributed to the study design, data interpretation, and editing of the manuscript. SM contributed to the data management, data analysis, data interpretation, writing, and editing of the manuscript. All authors approved the final version of the manuscript. ARQ and SM had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the American Diabetes Association or the National Institutes of Health.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Quiñones, A.R., Markwardt, S. & Botoseneanu, A. Diabetes-Multimorbidity Combinations and Disability Among Middle-aged and Older Adults. J GEN INTERN MED 34, 944–951 (2019). https://doi.org/10.1007/s11606-019-04896-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-04896-w