ABSTRACT
BACKGROUND
Guidelines for anticoagulant therapy in patients with atrial fibrillation (AF) conflict with each other. The American College of Chest Physicians (ACCP) guidelines suggest no anticoagulant therapy for patients with a CHADS2 score of 0. The European Society of Cardiology (ESC) prefer anticoagulant therapy for patients with a CHA2DS2-VASc of 1, which includes 65–74-year-olds with a CHADS2 score of 0. Resolving this conflicting advice is important, because these guidelines have potential to change anticoagulant therapy in 10 % of the AF population.
METHODS
Using the National Registry of Atrial Fibrillation (NRAF) II data set, we compared these guidelines using stroke equivalents. Based on structured review of 23,657 patient records, we identified 65–74-year-old patients with a CHADS2 stroke score of 0 and no contraindication to warfarin. We used Medicare claims data to ascertain rates of ischemic stroke, intracranial hemorrhage, and other hemorrhage. We calculated net stroke equivalents for these (N = 478) patients using a weight of 1.5 for intracranial hemorrhages (ICH) and 1.0 for ischemic stroke. In a multivariate analysis, we used 14,466 records with documented atrial fibrillation and adjusted for CHADS2 and HEMORR2 HAGES score.
RESULTS
In 65–74-year-old patients with a CHADS2 stroke score of 0, the stroke equivalents per 100 patient-years was 2.6 with warfarin and 2.9 without warfarin; the difference between these two strategies was not significant (0.3 stroke equivalents, 95 % CI −3.2 to 3.7). However, rates of hemorrhage per 100 patient-years were nearly tripled (hazard ratio 2.9; 95 % CI 1.5–5.4; p = 0.0011) with warfarin (21.1) versus without it (7.4). The most common site for major hemorrhage was gastrointestinal (ICD-9 code 578.9).
CONCLUSIONS
By expanding warfarin use to 65-–74-year-olds with a CHADS2 score of 0, rates of hemorrhages would rise without a significant reduction in stroke equivalents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Atrial fibrillation (AF) is the most common cardiac arrhythmia, and stroke prevention is a cornerstone of treatment in these patients. However, guidelines regarding anticoagulant therapy conflict with one another. The 2012 American College of Chest Physicians (ACCP) guidelines recommend the use of oral anticoagulant therapy in patients with AF who have a Congestive heart failure, Hypertension, Age > 75, Diabetes mellitus, and prior Stroke (CHADS2) score of 1 or greater.1 ACCP suggests no anticoagulant therapy for patients with a CHADS2 score of 0.1 However, the ACCP guidelines remark that there are other factors, such as age 65 to 74 years, female gender, vascular disease, and patient preferences, that may influence the choice of therapy for some patients.
These guidelines differ from the 2010 European Society of Cardiology (ESC) (Table 1) guidelines, which “prefer” anticoagulant therapy over aspirin in 65–74-year-old patients with a CHADS2 score of 0.2 The 2012 ESC AF Focused Update3 and the 2014 American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS)4 recommend anticoagulant therapy if AF patients age 65–74 are female or have vascular disease (because their CHA2DS2-VASc score would be 2 or more). However, for other 65–74-year-old patients with a CHADS2 score of 0 they state that either no antithrombotic therapy or treatment with an oral anticoagulant should (2012 ESC) or may (AHA/ACC/HRS) be considered because their CHA2DS2-VASc score would be 1.
These guidelines have not been directly compared. Such a comparison is important because of the potential of newer guidelines to expand use of oral anticoagulants in the AF population by 10 %.5 , 6 Although warfarin reduces stroke risk by 64 %,7 liberal use of oral anticoagulants exposes more patients to risks of therapy. Older cohort studies averaged 0.6 fatal hemorrhages per 100 patient-years of warfarin therapy.8 Contemporary trials of carefully selected participants, have 0.04 to 0.5 fatal hemorrhages per 100 patient-years of anticoagulant therapy.9
Here, we compare real-world outcomes [stroke, intracranial hemorrhage (ICH), and extracranial hemorrhage] in AF patients age 65 or older: specifically, we calculate the net clinical benefit of prescribing warfarin therapy to patients with a CHADS2 score of 0 who are age 65–74 years.
METHODS
Registry Data Sources
As previously detailed, the National Registry of Atrial Fibrillation (NRAF) II data set was created from 23,657 anonymous patient records gathered by Quality Improvement Organizations for the National Stroke Project.10 The project was managed by the Iowa Foundation for Medical Care and overseen by one of us (DSN). Participants were selected as a stratified random sample from Medicare beneficiaries who were hospitalized with AF [International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 427.31 in any diagnostic position] between 1 April 1998, and 31 March 1999. The first hospitalization in this time frame was defined as the baseline hospitalization. The NRAF II data set includes both Medicare Part A (MEDPAR A) claims records and medical record-abstracted data for these 23,657 patients at 3,586 hospitals from all 50 states. From MEDPAR files, we obtained information on principal and secondary diagnoses, diagnosis-related groups, and in-hospital procedures from the baseline hospitalization and from previous hospitalizations. From the Medicare denominator files, we obtained the date of death. Data collected from structured medical record abstractions was used to confirm the diagnosis of AF, determine the anticoagulant therapy prescribed at discharge, and identify comorbid conditions. Review of medical records to ascertain risk factors included inpatient records only. All data were de-identified before being transferred to Washington University in St. Louis, where the statistical analyses were performed. The Human Research Protection Office classified the research as exempt.
Identification of Stroke Risk Factors
We identified heart failure (HF), hypertension (HTN), age, diabetes (DM), stroke, transient ischemic attack (TIA), and female sex from structured medical record abstraction. The median inter-rater reliability for medical record abstractions on these elements was 97.9 % (interquartile range 93.8–99.1 %).11 Through medical record review, cardiovascular disease was defined as the presence of ischemic heart disease, angina, myocardial infarction, percutaneous transluminal coronary angioplasty or coronary artery bypass grafting performed during hospital stay.
Identification of Bleeding Risk Factors
Using systematic medical record abstraction, abstractors identified risk factors of the HEMORR2HAGES acronym and clinical prediction rule12: Hepatic disease or renal disease, Ethanol abuse, Malignancy (excluding skin cancer), Older age (>75), Reduced platelet count or reduced platelet function (e.g. taking aspirin), Rebleeding risk (i.e. history of major bleeding), Uncontrolled Hypertension, Anemia (admission hematocrit <30), Excess fall risk or neuropsychiatric disease (defined as: Alzheimer’s disease, other dementia/senility, chronic confusion, Parkinson’s disease, schizophrenia, or psychosis) and Stroke (previously). Genetic factors were not available in this data set. We chose the HEMORR2HAGES scheme as it has been validated using Medicare claims12 and includes some risk factors for bleeding (malignancy and excessive fall risk) that are not included in similar bleeding schemes.13
Medical record review was used to identify aspirin or warfarin prescription at the time of hospital discharge, but warfarin use after hospital discharge was not ascertained.
Exclusion Criteria
We excluded patients who were aged <65 years, died during the baseline hospitalization or within 30 days of hospital discharge, or had any of the following during index admission: a terminal illness, a complication related to warfarin or were at high risk for bleeding from warfarin, a history of hemorrhage, a bleeding disorder or thrombocytopenia, an intracranial surgery during their hospitalization, or a history of a heart valve replacement or repair. Patients who died within 30 days of hospital discharge were excluded from the main analysis, but included in a sensitivity analysis.
Outcomes
We identified ischemic strokes from validated11 ICD-9-CM codes (433.x1, 434.x1, 437.1, 437.9) that were the principal diagnosis in Medicare Part A records after the index admission. To improve specificity for acute stroke, we omitted ICD-9-CM codes for transient cerebral ischemia (435), for late effects of cerebrovascular disease (438.x), and for occlusion of the precerebral or cerebral arteries that did not have infarction (433.x0 or 434.x0), as recommended.11 We identified hemorrhages using the set of ICD-9 codes from a prior study.12 Major hemorrhages were defined as extracranial hemorrhages that met one or more criteria: (1) resulted in a length of stay > 24 h, (2) were fatal, or (3) required a transfer to another hospital. We classified non-fatal hemorrhages that had a length of stay of ≤ 1 day as “non-major, clinically relevant.”
We calculated net (ischemic) stroke equivalents using the methods of Singer et al.14 Specifically, we defined the net clinical benefit as the annual rate of ischemic stroke prevented by warfarin, minus 1.5 times the annual rate of intracranial hemorrhage attributable to warfarin. Intracranial hemorrhages have a worse score than ischemic strokes, because of the greater morbidity and mortality after an intracranial hemorrhage.15
Statistical Analysis
In the adjusted analysis, we used an exponential survival model to predict the annual rates of stroke, of intracranial hemorrhage, and of extracranial hemorrhage.16 The exponential survival models allowed us to use consistent hazard rates for adverse events that were adjusted for covariates. Specifically, the stroke rates were adjusted for CHADS2 score and warfarin prescription at time of discharge. The adjusted intracranial hemorrhage and extracranial hemorrhage rates were adjusted for HEMORR2AGES scores.12 We confirmed the appropriateness of using an exponential survival model graphically.17
We re-sampled the NRAF data set 1,000 times with replacement and used the binomial theorem and bootstrap18 to calculate 95 % CI for event rates and stroke equivalents. We performed statistical analyses using the SAS, version 9.2 (SAS Inc., Cary, NC). All p values were two-sided using an alpha of 0.05.
RESULTS
Participants
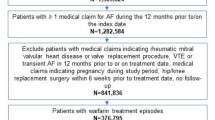
The NRAF II data set contained medical records from 23,657 Medicare beneficiaries with medical-record–documented AF. For this study, we sequentially excluded 837 patients younger than age 65 years, 528 of whom died within 30 days of hospitalization, 838 with a terminal illness, 6,155 with a recent hemorrhage or high risk of bleeding (as documented in the medical record), and 833 with a heart valve replacement/repair (Fig. 1). Of the remaining 14,466 patients, their average length of follow-up was 10 months. We focused our analysis on the 478 Medicare beneficiaries who had a CHADS2 score of 0 and the 2020 Medicare beneficiaries with a CHADS2 score of 1 (Tables 2 and 3). Because we excluded patients younger than 65 years, all patients with a CHADS2 score of 0 had at least one moderate risk factor for stroke (age 65–74 years).
Events in 65–74-Year-Old Patients with a CHADS2 Score of 0
Among patients with a CHADS2 score of 0, there were three ischemic strokes in patients on warfarin and six in patients not on warfarin. There was one intracranial hemorrhage in a patient on warfarin, and no intracranial hemorrhages in the non-warfarin group (on-line appendix). The stroke rate per 100 patient-years (Table 4) was 1.7 with warfarin and 2.9 without it (p = 0.40). The stroke equivalents per 100 patient-years (Table 4) were more similar (p = 0.84): 2.6 with warfarin and 2.9 without warfarin for a nonsignificant reduction of 0.3 (95 % CI −3.2 to 3.7) stroke equivalents. When we included patients who died within the first 30 days of hospitalization, results were identical.
Rates of hemorrhage per 100 patients-years (Table 5) were significantly greater with warfarin (21.1) than without it (7.4) (HR 2.9 (95 % CI 1.5–5.4) p = 0.0011). The most common site for major hemorrhage was gastrointestinal (ICD-9 code 578.9); the most common non-major hemorrhage was hematuria (ICD-9 code 599.7). The rate of extracranial hemorrhage per 100 patient-years was 20.5 with warfarin and 7.4 without it, for an absolute increase of 13.1 (95 % CI 4.8–21.4).
Number Needed to Treat
Based on the 0.3 stroke equivalents potentially prevented, the number needed to treat with warfarin to prevent one stroke equivalent is 333 patients (with a CHADS2 score of 0 aged 65–74). This expansion of warfarin use would cause ∼44 extracranial hemorrhages per 333 patients. Because 6.8 % of the extracranial hemorrhages were fatal, expanding warfarin use would cause ∼three fatal extracranial hemorrhages per one stroke equivalent saved.
Sensitivity Analysis
Next, we repeated our main analysis to include ICD-9 codes in any position, rather than only the principal diagnosis. Strokes rates (per 100 patient-years) were higher—3.4 without warfarin and 3.0 with warfarin—but intracranial hemorrhage rates were unchanged. Thus, in this analysis, warfarin use “increased” stroke equivalents by 0.5.
We also studied patients who had a CHADS2 score of 1: Warfarin use (as recommended by the ACCP guidelines) was associated with 1.7 fewer stroke equivalents per 100 patient-years of warfarin for a need-to-treat number of ∼60.
Adjusted Event Rates—Benefits of Warfarin
We repeated the analysis of stroke equivalents using all 14,466 patients without a contraindication to warfarin. In this multivariate analysis, which adjusted for CHADS2 and HEMORR2HAGEs scores and use of warfarin, warfarin “prevented” 0.02 stroke equivalents per 100 patient-years of therapy prescribed to 65–74-year-olds with a CHADS2 score of 0. The number needed to treat was 5,000.
DISCUSSION
Using the NRAF II Registry, we found no statistically significant reduction in stroke equivalents when adhering to the ESC and AHA/ACC/HRS guidelines, rather than to the ACCP guidelines. When 65–74-year-old patients with a CHADS2 score of 0 received warfarin therapy, 0.3 (95 % CI −3.2 to 3.7) stroke equivalents were “prevented” per 100 patient-years of therapy, which did not reach statistical significance. In the multivariate analysis of 14,466 patients, even fewer stroke equivalents were prevented (0.02) per 100 patient-years of warfarin prescribed to 65- to 74-year-old patients with a CHADS2 score of 0.
Although prior studies have not compared the ESC and AHA/ACC/HRS guidelines with the ACCP guidelines, they have examined outcomes in patients with a CHA2DS2-VASc score of 1. Multiple studies in diverse settings, have found stroke rates of one to two per 100 patient-years without anticoagulant therapy in 65–74-year-old patients with a CHADS2 score of 0.5 , 19 – 23 Cha et al. recommend that non-major risk factors (age 65–74 years, vascular disease, and female sex) receive lower weights than the CHADS2 factors, in proportion to their lower risk for stroke. Tsadok et al. found that in AF, female sex had only a 1.14 hazard ratio for stroke, and this ratio was even lower in women younger than 75 years.24 In summary, prior studies also have found low stroke rates in 65–74-year-old patients with a CHADS2 score of 0 who did not receive warfarin therapy, even in the setting of non-major risk factors.
An important difference between the present study and prior studies25 is that prior studies tended to comingle patients with a CHADS2 score of 1 and patients with a CHA2DS2-VASc score of 1. By lumping patients who had major (i.e., CHADS2) risk factors with patients who had only vascular disease, age 65–74 years, or female gender, prior studies did not quantify the risks and benefits of extending anticoagulant therapy as proposed by the ESC and AHA/ACC/HRS guidelines. Thus, prior work may have inadvertently inflated the trivial gain in stroke equivalents attributed to prescribing warfarin to 65–74-year-old patients with a CHADS2 score of 0.
In contrast to the insignificant gain in stroke equivalents associated with prescribing warfarin to 65–74-year-old patients with a CHADS2 score of 0, we found 2.9-fold more extracranial hemorrhages associated with this practice: To prevent one stroke equivalent, ∼333 patients would need to be prescribed warfarin, which would result in ∼44 extracranial hemorrhages, of which ∼three (6.8 %) would be fatal. Thus, expanding warfarin use to this low-risk population would increase mortality without a significant reduction in stroke equivalents.
The rate of major hemorrhage (6.2 per 100 patient-years of warfarin) observed here is similar or slightly greater than other real-world studies. Hylek et al. found that patients aged 65–74 years who had a CHADS2 of 0 had 3.12 major bleeds per 100 patient-years of warfarin therapy.26 Gomes et al. reported that patients with a CHADS2 score of 0 had 1.8 major bleeds per 100 patient-years overall, but 7.2 major bleeds during the initial 30 days of warfarin.27 Ghate et al. found that AF patients averaged 0.4 intracranial hemorrhages per 100 patient-years of warfarin.28 The greater hemorrhage rate in our population, may reflect the high prevalence of risk factors for hemorrhage in Medicare inpatients12 and frequent warfarin initiation.
Because of this risk of hemorrhage, it is premature to recommend anticoagulant therapy for AF patients without major risk factors. Although newer anticoagulants have lower risks of intracranial hemorrhage, their risks of extracranial hemorrhage are significant and their net benefit in patients with a CHADS2 score of 0 is unknown.29 , 30 Rivaroxaban or apixaban may be safer than dabigatran 150 mg twice daily,31 but may be less efficacious.32 , 33
Although the present analysis compared AF guidelines, rather than clinical prediction rules, our results also inform clinicians about the usefulness of CHADS2 and CHA2DS2-VASc. Both of these prediction rules guide anticoagulant therapy, with oral anticoagulants typically offered to patients with scores of 1 or greater.20 , 23 , 25 Here, we found that prescribing warfarin to patients with a CHADS2 score of 1 reduced stroke equivalents by 1.7 per 100 patient-years of anticoagulant therapy. In contrast, prescribing oral anticoagulants to patients with a CHA2DS2-VASc score ≥ 1 (and CHADS2 score of 0) reduced stroke equivalents minimally (0.02 or 0.3)—not enough to justify the increased risk of extracranial bleeding. A recent Canadian study found that prescribing warfarin to a similar population resulted in no decrease in cerebrovascular events.5 The Fushimi AF Registry also found no reduction in cerebrovascular events from warfarin, but the average INR was only 1.82.34 Thus, adoption of CHA2DS2-VASc could expand the use of anticoagulants without improving health.
Our study has potential limitations. First, we used ICD-9-CM to determine adverse events. To decrease the risk of misclassification, we used ICD-9-CM codes that have been validated.35 , 36 Second, we knew the therapy prescribed at discharge, but could not determine compliance with warfarin and warfarin monitoring. Third, the weight of 1.5 per intracranial hemorrhage is based on precedent, but other weights are also possible.19 Fourth, our analysis is based on older data that precede use of newer oral anticoagulants. Finally, laboratory-based definitions could not be used to define major hemorrhage because the number of units of transfused blood was not available in the administrative data.
The limitations are offset by several strengths. First, we studied a diverse, real-world population who had multiple co-morbid conditions. Thus, warfarin was managed per standard care, rather than in the setting of a carefully managed clinical trial. Second, risk factors and medications were determined directly from review of all 23,657 records. Third, the size of the NRAF II was large enough for us to detect a statistically significant increase in hemorrhage risk when warfarin was prescribed to the subset of 65–75-year-olds who had a CHADS2 score of 0.
With rising costs in the health care field, net clinical benefit analyses can guide use of expensive treatments that are not necessarily benign. As compared to the ACCP guidelines, adherence to the ESC and AHA/ACC/HRS may increase hemorrhage, including fatal hemorrhages, without a commensurate reduction in stroke equivalents.
REFERENCES
You JJ, Singer DE, Howard PA, et al. Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e531S–e575S. doi:10.1378/chest. 11-2304.
Camm AJ, Kirchhof P, Lip GY, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010;31(19):2369–2429. doi:10.1093/eurheartj/ehq278.
Camm AJ, Lip GY, De Caterina R, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33(21):2719–2747. doi:10.1093/eurheartj/ehs253.
January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation. 2014. doi:10.1161/CIR.0000000000000041.
Sandhu RK, Bakal JA, Ezekowitz JA, McAlister FA. Risk stratification schemes, anticoagulation use and outcomes: the risk–treatment paradox in patients with newly diagnosed non-valvular atrial fibrillation. Heart. 2011;97(24):2046–2050. doi:10.1136/heartjnl-2011-300901.
Mason PK, Lake DE, Dimarco JP, et al. Impact of the CHA(2)DS(2)-VASc Score on Anticoagulation Recommendations for Atrial Fibrillation. Am J Med. 2012;125(6):603 e1-6. doi:10.1016/j.amjmed.2011.09.030.
Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146(12):857–867.
Landefeld SC, Beyth R. Anticoagulant-related bleeding: clinical epidemiology, prediction and prevention. Am J Med. 1993;95:315–328.
Agarwal S, Hachamovitch R, Menon V. Current trial-associated outcomes with warfarin in prevention of stroke in patients With nonvalvular atrial fibrillation: a meta-analysis. Arch Intern Med. 2012;172(8):623–631. doi:10.1001/archinternmed.2012.121.
Jencks SF, Cuerdon T, Burwen DR, et al. Quality of medical care delivered to Medicare beneficiaries: a profile at state and national levels. JAMA. 2000;284(13):1670–1676.
Birman-Deych E, Waterman AD, Yan Y, Nilasena DS, Radford MJ, Gage BF. Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care. 2005;43(5):480–485.
Gage BF, Yan Y, Milligan PE, et al. Clinical classification schemes for predicting hemorrhage: results from the National Registry of Atrial Fibrillation (NRAF). Am Heart J. 2006;151(3):713–719.
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093–1100. doi:10.1378/chest. 10-0134.
Singer DE, Chang Y, Fang MC, et al. The net clinical benefit of warfarin anticoagulation in atrial fibrillation. Ann Intern Med. 2009;151(5):297–305.
Gathier CS, Algra A, Rinkel GJ, van der Worp HB. Long-term outcome after anticoagulation-associated intracerebral haemorrhage with or without restarting antithrombotic therapy. Cerebrovasc Dis. 2013;36(1):33–37. doi:10.1159/000351151.
Lee. Statistical Methods for Survival Data Analysis. 2nd ed: John Wiley & Sons; 1992.
Allison PD. Survival Analysis Using the SAS System: A Practical Guide. Cary, NC: SAS Institute Inc; 1995.
Efron B, Tibshirani R. In: Cox DR, Hinkley DV, Reid N, Rubin DB, Silverman BW, eds. An Introduction to the Bootstrap. New York: Chapman & Hall; 1993.
Toda E, Lip GYH, Uchiyama S, et al. Sub-analysis of the Japan Thrombosis Registry for atrial fibrillation, coronary or cerebrosvascular events (J-TRACE) [abstract]. J Am Coll Cardiol. 2012;59(13s1):E674-E.
Olesen JB, Lip GY, Hansen ML, et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;342:d124. doi:10.1136/bmj.d124 bmj.d124.
Cha MJ, Oh GC, Hahn S, Choi EK, Oh S. Thromboembolic risk evaluation in patients with atrial fibrillation using a modified CHADS(2) scoring system. J Cardiovasc Electrophysiol. 2012;23(2):155–162. doi:10.1111/j.1540-8167.2011.02181.x.
Becattini C, Agnelli G, Schenone A, et al. Aspirin for preventing the recurrence of venous thromboembolism. N Engl J Med. 2012;366(21):1959–1967. doi:10.1056/NEJMoa1114238.
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285(22):2864–2870.
Avgil-Tsadok M, Jackevicius CA, Rahme E, Humphries KH, Behlouli H, Pilote L. Sex differences in stroke risk among older patients with recently diagnosed atrial fibrillation. JAMA. 2012;307(18):1952–1958. doi:10.1001/jama.2012.3490.
Olesen JB, Lip GY, Lindhardsen J, et al. Risks of thromboembolism and bleeding with thromboprophylaxis in patients with atrial fibrillation: a net clinical benefit analysis using a ‘real world’ nationwide cohort study. Thromb Haemost. 2011;106(4):739–749. doi:10.1160/TH11-05-0364.
Hylek EM, Evans-Molina C, Shea C, Henault LE, Regan S. Major hemorrhage and tolerability of warfarin in the first year of therapy among elderly patients with atrial fibrillation. Circulation. 2007;115(21):2689–2696.
Gomes T, Mamdani MM, Holbrook AM, Paterson JM, Hellings C, Juurlink DN. Rates of hemorrhage during warfarin therapy for atrial fibrillation. CMAJ. 2013;185(2):E121-7. doi:10.1503/cmaj.121218.
Ghate SR, Biskupiak J, Ye X, Kwong WJ, Brixner DI. All-cause and bleeding-related health care costs in warfarin-treated patients with atrial fibrillation. J Manag Care Pharm. 2011;17(9):672–684.
Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–1151. doi:10.1056/NEJMoa0905561.
Fox KA, Piccini JP, Wojdyla D, et al. Prevention of stroke and systemic embolism with rivaroxaban compared with warfarin in patients with non-valvular atrial fibrillation and moderate renal impairment. Eur Heart J. 2011;32(19):2387–2394. doi:10.1093/eurheartj/ehr342.
Lip GY, Larsen TB, Skjoth F, Rasmussen LH. Indirect comparisons of new oral anticoagulant drugs for efficacy and safety when used for stroke prevention in atrial fibrillation. J Am Coll Cardiol. 2012. doi:10.1016/j.jacc.2012.03.019.
Connolly SJ, Eikelboom J, Joyner C, et al. Apixaban in patients with atrial fibrillation. N Engl J Med. 2011;364(9):806–817. doi:10.1056/NEJMoa1007432.
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–891. doi:10.1056/NEJMoa1009638.
Akao M, Chun YH, Esato M, et al. Inappropriate use of oral anticoagulants for patients with atrial fibrillation. Circ J. 2014;78(9):2166–2172.
White RH, Beyth RJ, Zhou H, Romano PS. Major bleeding after hospitalization for deep-venous thrombosis. Am J Med. 1999;107(5):414–424.
Wahl PM, Rodgers K, Schneeweiss S, et al. Validation of claims-based diagnostic and procedure codes for cardiovascular and gastrointestinal serious adverse events in a commercially-insured population. Pharmacoepidemiol Drug Saf. 2010;19(6):596–603. doi:10.1002/pds.1924.
Acknowledgements
We thank the Iowa Foundation for Medical Care, the Quality Improvement Organizations that participated in NRAF, and the Centers for Medicare and Medicaid Services for providing the anonymous data used in these analyses. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of commercial products imply endorsement of them by the US Government. The conclusions presented are solely those of the authors, who assume full responsibility for the accuracy and completeness of the ideas presented.
We thank Barbara Lutey, MD, for her comments on an earlier version of the manuscript.
Funding Sources
This work was supported by the Mentors in Medicine Program at Washington University in St. Louis and the American Heart Association.
Conflicts of Interest
Dr. Gage consulted for Boehringer Ingelheim in 2013, with payment donated to charity and/or Washington University in St. Louis. All other authors declare that they do not have any conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 35 kb)
Rights and permissions
About this article
Cite this article
Andrade, A.A., Li, J., Radford, M.J. et al. Clinical Benefit of American College of Chest Physicians versus European Society of Cardiology Guidelines for Stroke Prophylaxis in Atrial Fibrillation. J GEN INTERN MED 30, 777–782 (2015). https://doi.org/10.1007/s11606-015-3201-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-015-3201-1