ABSTRACT
BACKGROUND
At some academic hospitals, medical procedure services are being developed to provide supervision for residents performing bedside procedures in hopes of improving patient safety and resident education. There is limited knowledge of the impact of such services on procedural complication rates and resident procedural training opportunities.
OBJECTIVE
To determine the impact of a medical procedure service (MPS) on patient safety and resident procedural training opportunities.
DESIGN
Retrospective cohort analysis comparing characteristics and outcomes of procedures performed by the MPS versus the primary medical service.
PARTICIPANTS
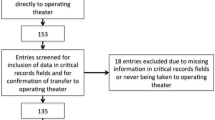
Consecutive adults admitted to internal medicine services at a large academic hospital who underwent a bedside medical procedure (central venous catheterization, thoracentesis, paracentesis, lumbar puncture) between 1 July 2010 and 31 December 2011.
MAIN MEASURES
The primary outcome was a composite rate of major complications. Secondary outcomes included resident participation in bedside procedures and use of “best practice” safety process measures.
KEY RESULTS
We evaluated 1,707 bedside procedures (548 by the MPS, 1,159 by the primary services). There were no differences in the composite rate of major complications (1.6 % vs. 1.9 %, p = 0.71) or resident participation in bedside procedures (57.0 % vs. 54.3 %, p = 0.31) between the MPS and the primary services. Procedures performed by the MPS were more likely to be successfully completed (95.8 % vs. 92.8 %, p = 0.02) and to use best practice safety process measures, including use of ultrasound guidance when appropriate (96.8 % vs. 90.0 %, p = 0.0004), avoidance of femoral venous catheterization (89.5 vs. 82.7 %, p = 0.02) and involvement of attending physicians (99.3 % vs. 57.0 %, p < 0.0001).
CONCLUSIONS
Although use of a MPS did not significantly affect the rate of major complications or resident opportunities for training in bedside procedures, it was associated with increased use of best practice safety process measures.
Similar content being viewed by others
REFERENCES
Hicks CM, Gonzalez R, Morton MT, Gibbons RV, Wigton RS, Anderson RJ. Procedural experience and comfort level in internal medicine trainees. J Gen Intern Med. 2000;15:716–722.
Mourad M, Kohlwes J, Maselli J, Auerbach AD. Supervising the supervisors—procedural training and supervision in internal medicine residency. J Gen Intern Med. 2010;25:351–356.
Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324:370–376.
Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, et al. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324:377–384.
Lenhard A, Moallem M, Marrie RA, Becker J, Garland A. An intervention to improve procedure education for internal medicine residents. J Gen Intern Med. 2008;23:288–293.
Lucas BP, Asbury JK, Wang Y, Lee K, Kumapley R, Mba B, et al. Impact of a bedside procedure service on general medicine inpatients: a firm-based trial. J Hosp Med. 2007;2:143–149.
Mourad M, Auerbach AD, Maselli J, Sliwka D. Patient satisfaction with a hospitalist procedure service: is bedside procedure teaching reassuring to patients? J Hosp Med. 2011;6:219–224.
Smith CC, Gordon CE, Feller-Kopman D, Huang GC, Weingart SN, Davis RB, et al. Creation of an innovative inpatient medical procedure service and a method to evaluate house staff competency. J Gen Intern Med. 2004;19:510–513.
Huang GC, Smith CC, Gordon CE, Feller-Kopman DJ, Davis RB, Phillips RS, et al. Beyond the comfort zone: residents assess their comfort performing inpatient medical procedures. Am J Med. 2006;119:71e17–71e24.
Mourad M, Ranji S, Sliwka D. A randomized controlled trial of the impact of a teaching procedure service on the training of internal medicine residents. J Grad Med Educ. 2012;4:170–175.
O’Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2011;39:S1–S34.
Graham AS, Ozment C, Tegtmeyer K, Lai S, Braner DA. Videos in clinical medicine. Central venous catheterization. N Engl J Med. 2007;356:e21.
Havelock T, Teoh R, Laws D, Gleeson F. Pleural procedures and thoracic ultrasound: British thoracic society pleural disease guideline 2010. Thorax. 2010;65(Suppl 2):ii61–ii76.
Marschall J, Mermel LA, Classen D, Arias KM, Podgorny K, Anderson DJ, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008;29(Suppl 1):S22–S30.
Miranda JA, Trick WE, Evans AT, Charles-Damte M, Reilly BM, Clarke P. Firm-based trial to improve central venous catheter insertion practices. J Hosp Med. 2007;2:135–142.
Accreditation Council for Graduate Medical Education. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/140_internal_medicine_07012013.pdf. Accessed September 17 2013.
American Board of Internal Medicine. http://www.abim.org/certification/policies/imss/im.aspx. Accessed September 17 2013.
Wickstrom GC, Kolar MM, Keyserling TC, Kelley DK, Xie SX, Bognar BA, et al. Confidence of graduating internal medicine residents to perform ambulatory procedures. J Gen Intern Med. 2000;15:361–365.
Wigton RS, Alguire P. The declining number and variety of procedures done by general internists: a resurvey of members of the American College of Physicians. Ann Intern Med. 2007;146:355–360.
Barsuk JH, McGaghie WC, Cohen ER, Balachandran JS, Wayne DB. Use of simulation-based mastery learning to improve the quality of central venous catheter placement in a medical intensive care unit. J Hosp Med. 2009;4:397–403.
Barsuk JH, McGaghie WC, Cohen ER, O’Leary KJ, Wayne DB. Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Crit Care Med. 2009;37:2697–2701.
Lucas BP, Asbury JK, Franco-Sadud R. Training future hospitalists with simulators: a needed step toward accessible, expertly performed bedside procedures. J Hosp Med. 2009;4:395–396.
Wayne DB, Barsuk JH, O’Leary KJ, Fudala MJ, McGaghie WC. Mastery learning of thoracentesis skills by internal medicine residents using simulation technology and deliberate practice. J Hosp Med. 2008;3:48–54.
Acknowledgements
Research Funding
Dr. Wiener is supported by the National Cancer Institute [Grant K07 CA 138772] and the Department of Veterans Affairs.
Prior Presentations
American Thoracic Society International Conference, San Francisco, CA, May 2012.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Disclaimer
The views expressed herein are those of the authors and do not necessarily represent the policy or position of the Dept. of Veterans Affairs or the United States government.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tukey, M.H., Wiener, R.S. The Impact of a Medical Procedure Service on Patient Safety, Procedure Quality and Resident Training Opportunities. J GEN INTERN MED 29, 485–490 (2014). https://doi.org/10.1007/s11606-013-2709-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-013-2709-5