Abstract
OBJECTIVE
Adopting features of the Chronic Care Model may reduce coronary heart disease risk and blood pressure in vulnerable populations. We evaluated a peer and practice team intervention on reduction in 4-year coronary heart disease risk and systolic blood pressure.
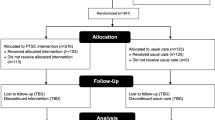
DESIGN AND SUBJECTS
A single blind, randomized, controlled trial in two adjacent urban university-affiliated primary care practices. Two hundred eighty African-American subjects aged 40 to 75 with uncontrolled hypertension.
INTERVENTION
Three monthly calls from trained peer patients with well-controlled hypertension and, on alternate months, two practice staff visits to review a personalized 4-year heart disease risk calculator and slide shows about heart disease risks. All subjects received usual physician care and brochures about healthy cooking and heart disease.
MAIN MEASURES
Change in 4-year coronary heart disease risk (primary) and change in systolic blood pressure, both assessed at 6 months.
KEY RESULTS
At baseline, the 136 intervention and 144 control subjects’ mean 4-year coronary heart disease risk did not differ (intervention = 5.8 % and control = 6.4 %, P = 0.39), and their mean systolic blood pressure was the same (140.5 mmHg, p = 0.83). Endpoint data for coronary heart disease were obtained for 69 % of intervention and 82 % of control subjects. After multiple imputation for missing endpoint data, the reduction in risk among all 280 subjects favored the intervention, but was not statistically significant (difference −0.73 %, 95 % confidence interval: -1.54 % to 0.09 %, p = 0.08). Among the 247 subjects with a systolic blood pressure endpoint (85 % of intervention and 91 % of control subjects), more intervention than control subjects achieved a >5 mmHg reduction (61 % versus 45 %, respectively, p = 0.01). After multiple imputation, the absolute reduction in systolic blood pressure was also greater for the intervention group (difference −6.47 mmHg, 95 % confidence interval: −10.69 to −2.25, P = 0.003). One patient died in each study arm.
CONCLUSIONS
Peer patient and office-based behavioral support for African-American patients with uncontrolled hypertension did not result in a significantly greater reduction in coronary heart disease risk but did significantly reduce systolic blood pressure.

Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Centers for Disease Control and Prevention. National Vital Statistic Report. Vol. 57, Num 14 Table B. http://www.cdc.gov/nchs/data/nvsr/nvsr58/nvsr58_19.pdf, accessed Jan 5, 2012.
Centers for Disease Control and Prevention. Health United States, 2008. Table 71. http://www.cdc.gov/nchs/data/hus/hus08.pdf, accessed Jan 5, 2012.
Kramer H, Han C, Post W, Goff D, Diez-Roux A, Cooper R, Jinagouda S, Shea S. Racial-ethnic differences in hypertension and hypertension treatment and control in the multi-ethnic study of atherosclerosis (MESA). Am J Hypertens. 2004;17(10):963–70.
Umscheid CA, Gross R, Weiner MG, Hollenbeak CS, Tang SS, Turner BJ. Racial disparities in hypertension control, but not treatment intensification. Am J Hypertens. 2010;23(1):54–61.
Bosworth HB, Powers B, Grubber JM, Thorpe CT, Olsen MK, Orr M, et al. Racial differences in blood pressure control: potential explanatory factors. J Gen Intern Med. 2008;23(5):692–8.
Bokhour BG, Berlowitz DR, Long JA, Kressin NR. How do providers assess antihypertensive medication adherence in medical encounters? J Gen Intern Med. 2006;21:577–83.
Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the chronic care model in the new millennium. Health Aff (Millwood). 2009;28(1):75–85.
Moy E, Valente E Jr, Levin RJ, Griner PF. Academic medical centers and the care of underserved populations. Acad Med. 1996;71(12):1370–7.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72.
Turner BJ, Weiner M, Yang C, TenHave T. Predicting adherence to colonoscopy or flexible sigmoidoscopy on the basis of physician appointment-keeping behavior. Ann Intern Med. 2004;140:528–32.
Turner BJ, Hollenbeak C, Weiner MG, Ten Have T, Roberts C. Barriers to adherence and hypertension control in a racially diverse representative sample of elderly primary care patients. Pharmacoepidemiol Drug Safe. 2009;18:672–81.
Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. 1999;282(18):1737–44.
Azjen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211.
Miller WR, Rollnick S. Motivational Interviewing: preparing People for Change. 2nd ed. New York: Guilford Press; 2002.
D'Agostino RB, Russell MW, Huse DM, Ellison RC, Silbershatz H, Wilson PW, et al. Primary and subsequent coronary risk appraisal: new results from the Framingham study. Am Heart J. 2000;139(2 Pt 1):272–81. Erratum in: Am Heart J. 2002;143(1):21.
Benner JS, Erhardt L, Flammer M, Moller RA, Rajicic N, Changela K, et al. A novel programme to evaluate and communicate 10-year risk of CHD reduces predicted risk and improves patients' modifiable risk factor profile. Int J Clin Pract. 2008;62(10):1484–98.
Shaffer ML, Chinchilli VM. Including multiple imputation in a sensitivity analysis for clinical trials with treatment failures. Contemp Clin Trials. 2007;28(2):130–7.
Raghunathan TW, Lepkowksi JM, Van Hoewyk J, Solenbeger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol. 2001;27:85–95.
Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley and Sons; 1987.
Barg FK, Weiner MG, Joseph S, Pandit K, Turner BJ. Qualitative analysis of peer coaches' experiences with counseling African Americans about reducing heart disease risk. J Gen Intern Med. 2012;27(2):167–72.
Houston TK, Allison JJ, Sussman M, Horn W, Holt CL, Trobaugh J, et al. Culturally appropriate storytelling to improve blood pressure: a randomized trial. Ann Intern Med. 2011;154(2):77–84.
Wu J, Kraja AT, Oberman A, Lewis CE, Ellison RC, Arnett DK, et al. A summary of the effects of antihypertensive medications on measured blood pressure. Am J Hypertens. 2005;18:935–42.
Heisler M, Vijan S, Makki F, Piette JD. Diabetes control with reciprocal peer support versus nurse care management: a randomized trial. Ann Intern Med. 2010;153(8):507–15.
Smith SM, Paul G, Kelly A, Whitford DL, O'Shea E, O'Dowd T. Peer support for patients with type 2 diabetes: cluster randomised controlled trial. BMJ. 2011;342. doi:10.1136/bmj.d715.
Kressin NR, Orner MB, Manze M, Glickman ME, Berlowitz D. Understanding contributors to racial disparities in blood pressure control. Circ Cardiovasc Qual Outcomes. 2010;3(2):173–80.
Koelewijn-van Loon MS, van der Weijden T, Ronda G, van Steenkiste B, Winkens B, Elwyn G, et al. Improving lifestyle and risk perception through patient involvement in nurse-led cardiovascular risk management: a cluster-randomized controlled trial in primary care. Prev Med. 2010;50(1–2):35–44.
Svetkey LP, Pollak KI, Yancy WS Jr, Dolor RJ, Batch BC, Samsa G, et al. Hypertension improvement project: randomized trial of quality improvement for physicians and lifestyle modification for patients. Hypertension. 2009;54(6):1226–33.
Centers for Disease Control and Prevention. CDC health disparities and inequality report–United States 2011. MMWR. 2011;60(Suppl):1–20.
Acknowledgments
We would like to thank our funding support from the Robert Wood Johnson Foundation and the staff of the Finding Answers, Disparities Research for Change Program. We also received an unrestricted grant from Pfizer, Inc., for the conduct of this study.
We would also like to thank the American Heart Association and especially Laura Dawson, Director, Cultural Health Initiatives, Great Rivers Affiliate, American Heart Association for her support throughout the project. We thank our peer coaches and community advisors, especially Mrs. Claire Walters, our lead peer coach, for her incredible talent and dedication to this project. We would like to also thank Josh Benner, PhD, for his assistance in the development of this project.
Conflict of Interest
The project received an unrestricted supplementary grant from Pfizer, Inc., to the University of Pennsylvania. The authors declare that they have no other conflicts.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial Registration: (ClinicalTrials.gov number NCT00948714 Support for Cardiovascular Health in African American Primary Care Patients). Funded by the Robert Wood Johnson Foundation Informing Disparities program and Pfizer, Inc.
Rights and permissions
About this article
Cite this article
Turner, B.J., Hollenbeak, C.S., Liang, Y. et al. A Randomized Trial of Peer Coach and Office Staff Support to Reduce Coronary Heart Disease Risk in African-Americans with Uncontrolled Hypertension. J GEN INTERN MED 27, 1258–1264 (2012). https://doi.org/10.1007/s11606-012-2095-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2095-4